Ann Surg Treat Res.
2019 May;96(5):209-215. 10.4174/astr.2019.96.5.209.
Implementation of a resident night float system in a surgery department in Korea for 6 months: electronic medical record-based big data analysis and medical staff survey
- Affiliations
-
- 1Department of Surgery, Seoul National University Bundang Hospital, Seongnam, Korea. tslee@snubh.org
- 2Department of Surgery, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2443583
- DOI: http://doi.org/10.4174/astr.2019.96.5.209
Abstract
- PURPOSE
To evaluate superiority of a night float (NF) system in comparison to a traditional night on-call (NO) system for surgical residents at a single institution in terms of efficacy, safety, and satisfaction.
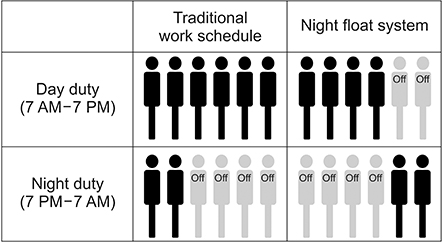
METHODS
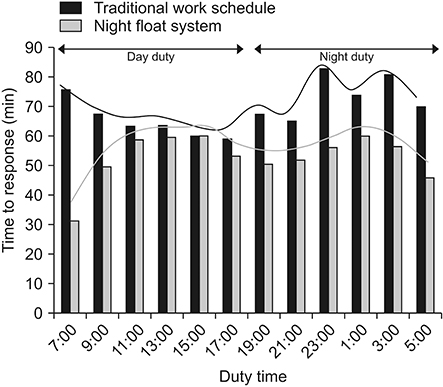
A NF system was implemented from March to September 2017 and big data analysis from electronic medical records was performed for all patients admitted for surgery or contacted from the emergency room (ER). Parameters including vital signs, mortality, and morbidity rates, as well as promptness of response to ER calls, were compared against a comparable period (March to September 2016) during which a NO system was in effect. A survey was also performed for physicians and nurses who had experienced both systems.
RESULTS
A total of 150,000 clinical data were analyzed. Under the NO and NF systems, a total of 3,900 and 3,726 patients were admitted for surgery. Mortality rates were similar but postoperative bleeding was significantly higher in the NO system (0.5% vs. 0.2%, P = 0.031). From the 1,462 and 1,354 patients under the NO and NF systems respectively, that required surgical consultation from the ER, the time to response was significantly shorter in the NF system (54.5 ± 70.7 minutes vs. 66.8 ± 83.8 minutes, P < 0.001). Both physicians (90.4%) and nurses (91.4%) agreed that the NF system was more beneficial.
CONCLUSION
This is the first report of a NF system using big data analysis in Korea, and potential benefits of this new system were observed in both ward and ER patient management.
MeSH Terms
Figure
Reference
-
1. Johns MM, Ulmer C, Wolman DM. Resident duty hours: enhancing sleep, supervision, and safety. Washington (DC): National Academies Press (US);2009.2. Landrigan CP, Rothschild JM, Cronin JW, Kaushal R, Burdick E, Katz JT, et al. Effect of reducing interns' work hours on serious medical errors in intensive care units. N Engl J Med. 2004; 351:1838–1848.
Article3. Jagsi R, Kitch BT, Weinstein DF, Campbell EG, Hutter M, Weissman JS. Residents report on adverse events and their causes. Arch Intern Med. 2005; 165:2607–2613.
Article4. Leape LL. The girl who died twice: every patient's nightmare: the libby zion case and the hidden hazards of hospitals. JAMA. 1996; 275:1031.
Article5. Pastores SM, O'Connor MF, Kleinpell RM, Napolitano L, Ward N, Bailey H, et al. The Accreditation Council for Graduate Medical Education resident duty hour new standards: history, changes, and impact on staffing of intensive care units. Crit Care Med. 2011; 39:2540–2549.
Article6. Trontell MC, Carson JL, Taragin MI, Duff A. The impact of the night float system on internal medicine residency programs. J Gen Intern Med. 1991; 6:445–449.
Article7. Oh SH, Kim JS, Lee PS. A survey on training and working conditions of residents in 2015. J Korean Med Assoc. 2015; 58:1179–1189.
Article8. Arnedt JT, Owens J, Crouch M, Stahl J, Carskadon MA. Neurobehavioral performance of residents after heavy night call vs after alcohol ingestion. JAMA. 2005; 294:1025–1033.
Article9. Jacques CH, Lynch JC, Samkoff JS. The effects of sleep loss on cognitive performance of resident physicians. J Fam Pract. 1990; 30:223–229.10. Arzalier-Daret S, Buleon C, Bocca ML, Denise P, Gerard JL, Hanouz JL. Effect of sleep deprivation after a night shift duty on simulated crisis management by residents in anaesthesia. A randomised crossover study. Anaesth Crit Care Pain Med. 2018; 37:161–166.
Article11. Resident duty hours in the learning and working environment. Comparison of 2003 and 2011 standards [Internet]. Chicago (IL): Accreditation Council for Graduate Medical Education;2000–2019. cited 2014 Jul 18. Available from: http://www.acgme.org/Portals/0/PDFs/dh-ComparisonTable2003v2011.pdf.12. Ahmed N, Devitt KS, Keshet I, Spicer J, Imrie K, Feldman L, et al. A systematic review of the effects of resident duty hour restrictions in surgery: impact on resident wellness, training, and patient outcomes. Ann Surg. 2014; 259:1041–1053.13. Sterling L, McCaffrey C, Secter M, Rich R, Green J, Shirreff L, et al. Development of a night float call model for obstetrics and gynaecology residency: the process and residents' perceptions. J Obstet Gynaecol Can. 2016; 38:1061–1064.
Article14. Jo JH. Will sudden death of 9 years old boy lead to a new law for patient safety? OhmyNews [Internet]. 2013. 04. 08. cited 2018 Sep 12. Available from: http://m.ohmynews.com/NWS_Web/Mobile/at_pg.aspx?CNTN_CD=A0001852173#cb.4081.15. Kwack EK, Kim DJ, Park TI, Cho KR, Kwon IH, Sohn YK. Neural toxicity induced by accidental intrathecal vincristine administration. J Korean Med Sci. 1999; 14:688–692.
Article16. Mann SM, Borschneck DP, Harrison MM. Implementation of a novel night float call system: resident satisfaction and quality of life. Can J Surg. 2014; 57:15–20.
Article17. Namdari S, Baldwin KD, Weinraub B, Mehta S. Changes in the number of resident publications after inception of the 80-hour work week. Clin Orthop Relat Res. 2010; 468:2278–2283.
Article18. Jones AM, Jones KB. The 88-hour family: effects of the 80-hour work week on marriage and childbirth in a surgical residency. Iowa Orthop J. 2007; 27:128–133.19. Ferguson CM, Kellogg KC, Hutter MM, Warshaw AL. Effect of work-hour reforms on operative case volume of surgical residents. Curr Surg. 2005; 62:535–538.
Article20. Brasel KJ, Fata P, Flynn TC. Members of the Evidence Based Reviews in Surgery Group. Impact of the 80-hour resident work week on mortality and morbidity in trauma patients. Can J Surg. 2013; 56:204–206.
Article21. Anderson JE, Goodman LF, Jensen GW, Salcedo ES, Galante JM. Restrictions on surgical resident shift length does not impact type of medical errors. J Surg Res. 2017; 212:8–14.
Article22. Kim HJ, Kim JH, Park KD, Choi KG, Lee HW. A survey of sleep deprivation patterns and their effects on cognitive functions of residents and interns in Korea. Sleep Med. 2011; 12:390–396.
Article23. Shirreff L, Shapiro JL, Yudin MH. Perceptions of a night float system of resident call within an obstetrics and gynaecology residency training program. J Obstet Gynaecol Can. 2014; 36:957–961.
Article24. Goitein L, Shanafelt TD, Nathens AB, Curtis JR. Effects of resident work hour limitations on faculty professional lives. J Gen Intern Med. 2008; 23:1077–1083.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Nursing Records of Open Heart Surgery Patients before and after Implementation of Electronic Nursing Record
- Multicenter Implementation of a New Electronic Medical Record System Leads to Longer Procedure Times and Poor Staff Satisfaction
- Adaptation Trends of Emergency Medical Personnel after Implementation of the Electronic Medical Record System into Emergency Care
- Methodological Round: Prospect of Artificial Intelligence Based on Electronic Medical Record
- Satisfaction with Paper-Based Dental Records and Perception of Electronic Dental Records among Dental Professionals in Myanmar