World J Mens Health.
2019 May;37(2):128-137. 10.5534/wjmh.180078.
Review of Guidelines for the Evaluation and Treatment of Leukocytospermia in Male Infertility
- Affiliations
-
- 1College of Medicine and Life Sciences, University of Toledo, Toledo, OH, USA.
- 2Department of Urology, College of Medicine and Life Sciences, University of Toledo, Toledo, OH, USA. jhdemeter@gmail.com
- KMID: 2443228
- DOI: http://doi.org/10.5534/wjmh.180078
Abstract
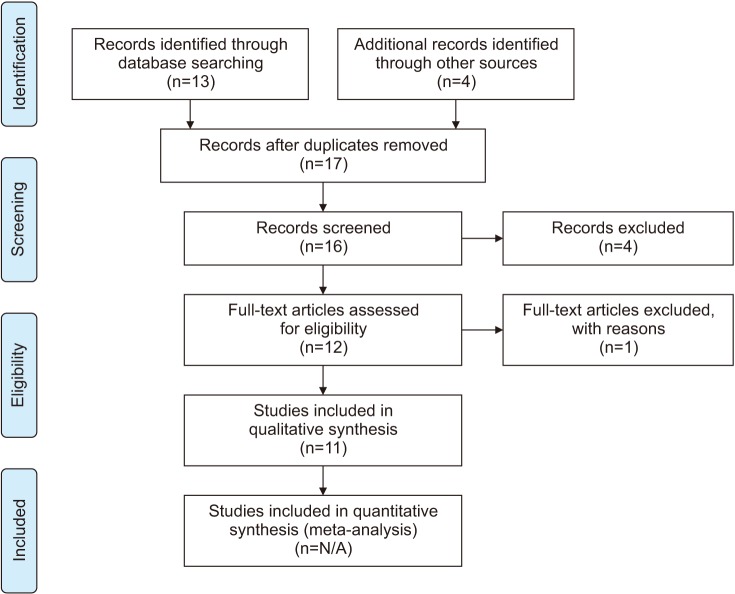
- Leukocytospermia is an ill-defined and poorly understood condition affecting up to 30% of male factor infertility. Current guidelines on leukocytospermia vary significantly, although it has been linked to increased rates of infertility, uncertainty about its clinical significance, diagnosis, and treatment remains. The guidelines are conflicting with sparse data scattered across different specialties and continents. This study aims to compare and contrast available international guidelines and recommendations. In addition to these guidelines, we sought to consolidate the findings of trials over the last several decades. English language articles on human observational studies, retrospective, prospective, clinical trials and randomized control trials were searched for using the following terms: "leukocytospermia, pyospermia, and male infertility." Articles about treatment and management of leukocytospermia that were published between January 2010 and April 2018 were included, as well as four articles referenced in best practice and guideline statements from urological and andrological associations. Disagreements on this topic are highlighted as some guidelines describe no correlation between leukocytospermia and infertility while others show that treatment leads to improvement of sperm quality by many measures including improved pregnancy rate. Various treatments have been suggested including antibiotics, anti-inflammatory medications, and frequent ejaculation. There is a need for definitive characterization of Leukocytospermia as an infectious or inflammatory marker and a re-evaluation of the leukocyte concentration threshold. Additional studies investigating rates of conception as a measure of outcome are needed, to provide greater level of evidence and generalizability of leukocytopsermia management.
Keyword
MeSH Terms
Figure
Reference
-
1. Gnoth C, Godehardt E, Frank-Herrmann P, Friol K, Tigges J, Freundl G. Definition and prevalence of subfertility and infertility. Hum Reprod. 2005; 20:1144–1147. PMID: 15802321.
Article2. Thonneau P, Marchand S, Tallec A, Ferial ML, Ducot B, Lansac J, et al. Incidence and main causes of infertility in a resident population (1,850,000) of three French regions (1988–1989). Hum Reprod. 1991; 6:811–816. PMID: 1757519.3. Agarwal A, Mulgund A, Hamada A, Chyatte MR. A unique view on male infertility around the globe. Reprod Biol Endocrinol. 2015; 13:37. PMID: 25928197.
Article4. Sandoval JS, Raburn D, Muasher S. Leukocytospermia: overview of diagnosis, implications, and management of a controversial finding. Middle East Fertil Soc J. 2013; 18:129–134.
Article5. Bachir BG, Jarvi K. Infectious, inflammatory, and immunologic conditions resulting in male infertility. Urol Clin North Am. 2014; 41:67–81. PMID: 24286768.
Article6. Shy KK, Stenchever MA, Muller CH. Sperm penetration assay and subsequent pregnancy: a prospective study of 74 infertile men. Obstet Gynecol. 1988; 71:685–690. PMID: 3357655.7. Gambera L, Serafini F, Morgante G, Focarelli R, De Leo V, Piomboni P. Sperm quality and pregnancy rate after COX-2 inhibitor therapy of infertile males with abacterial leukocytospermia. Hum Reprod. 2007; 22:1047–1051. PMID: 17208944.
Article8. Domes T, Lo KC, Grober ED, Mullen JB, Mazzulli T, Jarvi K. The incidence and effect of bacteriospermia and elevated seminal leukocytes on semen parameters. Fertil Steril. 2012; 97:1050–1055. PMID: 22341372.
Article9. Jung JH, Kim MH, Kim J, Baik SK, Koh SB, Park HJ, et al. Treatment of leukocytospermia in male infertility: a systematic review. World J Mens Health. 2016; 34:165–172. PMID: 28053945.
Article10. World Health Organization. WHO laboratory manual for the examination and processing of human semen. 5th ed. Geneva: World Health Organization;2010.11. Jarow J, Sigman M, Kolettis PN, Lipshultz LR, McClure RD, Nangia AK, et al. The optimal evaluation of the infertile male: AUA best practice statement. Linthicum: American Urological Association, Inc.;2011.12. Wolff H, Anderson DJ. Immunohistologic characterization and quantitation of leukocyte subpopulations in human semen. Fertil Steril. 1988; 49:497–504. PMID: 3342902.13. Nickel JC. Prostatitis. Can Urol Assoc J. 2011; 5:306–315. PMID: 22031609.14. Jungwirth A, Giwercman A, Tournaye H, Diemer T, Kopa Z, Dohle G, et al. European Association of Urology Working Group on Male Infertility. European Association of Urology guidelines on male infertility: the 2012 update. Eur Urol. 2012; 62:324–332. PMID: 22591628.
Article15. Tomlinson MJ, Barratt CL, Cooke ID. Prospective study of leukocytes and leukocyte subpopulations in semen suggests they are not a cause of male infertility. Fertil Steril. 1993; 60:1069–1075. PMID: 8243688.
Article16. Weidner W, Krause W, Ludwig M. Relevance of male accessory gland infection for subsequent fertility with special focus on prostatitis. Hum Reprod Update. 1999; 5:421–432. PMID: 10582781.
Article17. Comhaire FH, Rowe PJ, Farley TM. The effect of doxycycline in infertile couples with male accessory gland infection: a double blind prospective study. Int J Androl. 1986; 9:91–98. PMID: 3539821.
Article18. Branigan EF, Muller CH. Efficacy of treatment and recurrence rate of leukocytospermia in infertile men with prostatitis. Fertil Steril. 1994; 62:580–584. PMID: 7520396.19. Yamamoto M, Hibi H, Katsuno S, Miyake K. Antibiotic and ejaculation treatments improve resolution rate of leukocytospermia in infertile men with prostatitis. Nagoya J Med Sci. 1995; 58:41–45. PMID: 7659146.20. Yanushpolsky EH, Politch JA, Hill JA, Anderson DJ. Antibiotic therapy and leukocytospermia: a prospective, randomized, controlled study. Fertil Steril. 1995; 63:142–147. PMID: 7805903.21. Erel CT, Sentürk LM, Demir F, Irez T, Ertüngealp E. Antibiotic therapy in men with leukocytospermia. Int J Fertil Womens Med. 1997; 42:206–210. PMID: 9222805.22. Pajovic B, Radojevic N, Vukovic M, Stjepcevic A. Semen analysis before and after antibiotic treatment of asymptomatic Chlamydia- and Ureaplasma-related pyospermia. Andrologia. 2013; 45:266–271. PMID: 22897222.
Article23. Vicari E. Effectiveness and limits of antimicrobial treatment on seminal leukocyte concentration and related reactive oxygen species production in patients with male accessory gland infection. Hum Reprod. 2000; 15:2536–2544. PMID: 11098023.
Article24. Oliva A, Multigner L. Ketotifen improves sperm motility and sperm morphology in male patients with leukocytospermia and unexplained infertility. Fertil Steril. 2006; 85:240–243. PMID: 16412767.
Article25. Milardi D, Luca G, Grande G, Ghezzi M, Caretta N, Brusco G, et al. Prednisone treatment in infertile patients with oligozoospermia and accessory gland inflammatory alterations. Andrology. 2017; 5:268–273. PMID: 28125168.
Article26. Lackner JE, Herwig R, Schmidbauer J, Schatzl G, Kratzik C, Marberger M. Correlation of leukocytospermia with clinical infection and the positive effect of antiinflammatory treatment on semen quality. Fertil Steril. 2006; 86:601–605. PMID: 16782098.
Article27. Henkel R, Kierspel E, Stalf T, Mehnert C, Menkveld R, Tinneberg HR, et al. Effect of reactive oxygen species produced by spermatozoa and leukocytes on sperm functions in non-leukocytospermic patients. Fertil Steril. 2005; 83:635–642. PMID: 15749492.
Article28. Sharma RK, Pasqualotto AE, Nelson DR, Thomas AJ Jr, Agarwal A. Relationship between seminal white blood cell counts and oxidative stress in men treated at an infertility clinic. J Androl. 2001; 22:575–583. PMID: 11451354.29. Menkveld R, Kruger TF. Sperm morphology and male urogenital infections. Andrologia. 1998; 30(Suppl 1):49–53.
Article30. Punab M, Lõivukene K, Kermes K, Mändar R. The limit of leucocytospermia from the microbiological viewpoint. Andrologia. 2003; 35:271–278. PMID: 14535854.
Article31. Lackner J, Schatzl G, Horvath S, Kratzik C, Marberger M. Value of counting white blood cells (WBC) in semen samples to predict the presence of bacteria. Eur Urol. 2006; 49:148–152. discussion 152-3. PMID: 16314032.
Article32. Thomas J, Fishel SB, Hall JA, Green S, Newton TA, Thornton SJ. Increased polymorphonuclear granulocytes in seminal plasma in relation to sperm morphology. Hum Reprod. 1997; 12:2418–2421. PMID: 9436676.
Article33. Hamada A, Agarwal A, Sharma R, French DB, Ragheb A, Sabanegh ES Jr. Empirical treatment of low-level leukocytospermia with doxycycline in male infertility patients. Urology. 2011; 78:1320–1325. PMID: 22137697.
Article34. Ricci G, Granzotto M, Luppi S, Giolo E, Martinelli M, Zito G, et al. Effect of seminal leukocytes on in vitro fertilization and intracytoplasmic sperm injection outcomes. Fertil Steril. 2015; 104:87–93. PMID: 25936234.