Dement Neurocogn Disord.
2015 Jun;14(2):53-69. 10.12779/dnd.2015.14.2.53.
Understanding of Antipsychotics in Elderly Patients with Dementia
- Affiliations
-
- 1Department of Neurology, Hyoja Geriatric Hospital, Yongin, Korea. kwakdr@gmail.com
- 2Department of Neurology, Seoul Veterans Hospital, Seoul, Korea.
- 3Department of Psychiatry, Yong-in Mental Hospital, Yongin, Korea.
- KMID: 2443003
- DOI: http://doi.org/10.12779/dnd.2015.14.2.53
Abstract
- Elderly patients affected with dementia frequently accompany delusions, hallucinations and other psychotic symptoms. As such, these patients are commonly prescribed antipsychotic medications for the treatment of psychosis. However, in recent years, the use of antipsychotics has been widely debated for reasons concerning their efficacy and safety in these patients. Conventional antipsychotics have been widely used for behavioral psychological symptoms in dementia (BPSD) in the past. Atypical antipsychotics showed an efficacy superior to placebo in randomized studies in BPSD treatment, with a better tolerability profile versus conventional drugs. However, in 2002, the Food and Drug Administration alert the possible increase in cerebrovascular adverse events after using antipsychotics and consequent studies reported various adverse (including fatalities) events. Notwithstanding controversial data, antipsychotics are probably the best option for short-term treatment of severe BPSD. However, due to possible serious adverse events, long-term therapy is not recommended and clinician should decrease the dosage and discontinue treatment wherever a sufficient control of behavioral symptoms has been obtained. Before prescribing an antipsychotic drug, the possible risk factor should be structurally reviewed and monitored. The aim of this review is to asses systematically the efficacy and safety concern of antipsychotics in treating elderly patients with BPSD. And we also review how and what we should prescribe and monitor, if once antipsychotic medication is decided.
MeSH Terms
Figure
Cited by 1 articles
-
Anxiety in Dementia
Yong Tae Kwak, YoungSoon Yang, Min-Seong Koo
Dement Neurocogn Disord. 2017;16(2):33-39. doi: 10.12779/dnd.2017.16.2.33.
Reference
-
1. Jeste DV, Blazer D, Casey D, Meeks T, Salzman C, Schneider L, et al. ACNP White Paper: update on use of antipsychotic drugs in elderly persons with dementia. Neuropsychopharmacology. 2008; 33:957–970.
Article2. Ray WA, Chung CP, Murray KT, Hall K, Stein CM. Atypical antipsychotic drugs and the risk of sudden cardiac death. N Engl J Med. 2009; 360:225–235.
Article3. Wang PS, Schneeweiss S, Avorn J, Fischer MA, Mogun H, Solomon DH, et al. Risk of death in elderly users of conventional vs. atypical antipsychotic medications. N Engl J Med. 2005; 353:2335–2341.
Article4. Gareri P, De Fazio P, Stilo M, Ferreri G, De Sarro G. Conventional and atypical antipsychotics in the elderly : a review. Clin Drug Investig. 2003; 23:287–322.5. Gareri P, De Fazio P, De Fazio S, Marigliano N, Ferreri Ibbadu G, De Sarro G. Adverse effects of atypical antipsychotics in the elderly: a review. Drugs Aging. 2006; 23:937–956.6. Markowitz JS, Brown CS, Moore TR. Atypical antipsychotics. Part I: Pharmacology, pharmacokinetics, and efficacy. Ann Pharmacother. 1999; 33:73–85.
Article7. Seeman P. Atypical antipsychotics: mechanism of action. Can J Psychiatry. 2002; 47:27–38.
Article8. Burris KD, Molski TF, Xu C, Ryan E, Tottori K, Kikuchi T, et al. Aripiprazole, a novel antipsychotic, is a high-affinity partial agonist at human dopamine D2 receptors. J Pharmacol Exp Ther. 2002; 302:381–389.
Article9. Shayegan DK, Stahl SM. Atypical antipsychotics: matching receptor profile to individual patient's clinical profile. CNS Spectr. 2004; 9:10 Suppl 11. 6–14.
Article10. Leucht S, Arbter D, Engel RR, Kissling W, Davis JM. How effective are second-generation antipsychotic drugs? A meta-analysis of placebo-controlled trials. Mol Psychiatry. 2009; 14:429–447.
Article11. Khan AY, Preskorn SH. Examining concentration-dependent toxicity of clozapine: role of therapeutic drug monitoring. J Psychiatr Pract. 2005; 11:289–301.
Article12. Pollock BG. Psychotropic drugs and the aging patient. Geriatrics. 1998; 53:Suppl 1. S20–S24.13. Schoemaker H, Claustre Y, Fage D, Rouquier L, Chergui K, Curet O, et al. Neurochemical characteristics of amisulpride, an atypical dopamine D2/D3 receptor antagonist with both presynaptic and limbic selectivity. J Pharmacol Exp Ther. 1997; 280:83–97.14. Shahid M, Walker GB, Zorn SH, Wong EH. Asenapine: a novel psychopharmacologic agent with a unique human receptor signature. J Psychopharmacol. 2009; 23:65–73.
Article15. Maher AR, Theodore G. Summary of the comparative effectiveness review on off-label use of atypical antipsychotics. J Manag Care Pharm. 2012; 18:5 Suppl B. S1–S20.
Article16. Salzman C, Jeste DV, Meyer RE, Cohen-Mansfield J, Cummings J, Grossberg GT, et al. Elderly patients with dementia-related symptoms of severe agitation and aggression: consensus statement on treatment options, clinical trials methodology, and policy. J Clin Psychiatry. 2008; 69:889–898.
Article17. Herrmann N, Lanctôt KL. Pharmacologic management of neuropsychiatric symptoms of Alzheimer disease. Can J Psychiatry. 2007; 52:630–646.
Article18. Correll CU. Real-life dosing with second-generation antipsychotics. J Clin Psychiatry. 2005; 66:1610–1611.
Article19. Lacro JP, Kuczenski R, Roznoski M, Warren KA, Harris MJ, Jeste DV. Serum haloperidol levels in older psychotic patients. Am J Geriatr Psychiatry. 1996; 4:229–236.
Article20. Kwak YT, Yang Y, Koo MS. Late-onset psychosis; is it real? Dement Neurocognitive Disord. 2015; 14:1–11.
Article21. Kwak YT, Yang Y, Koo MS. Delusions in Alzheimer's Disease. Dement Neurocognitive Disord. 2014; 13:63–73.
Article22. Ereshefsky L. Pharmacokinetics and drug interactions: update for new antipsychotics. J Clin Psychiatry. 1996; 57:Suppl 11. 12–25.23. Correll CU. Antipsychotic use in children and adolescents: minimizing adverse effects to maximize outcomes. J Am Acad Child Adolesc Psychiatry. 2008; 47:9–20.
Article24. Casey DE, Carson WH, Saha AR, Liebeskind A, Ali MW, Jody D, et al. Switching patients to aripiprazole from other antipsychotic agents: a multicenter randomized study. Psychopharmacology (Berl). 2003; 166:391–399.
Article25. Royal College of Nursing (Great Britain). National Collaborating Centre for Nursing and Supportive Care (Great Britain). Violence: The Short-term Management of Disturbed/violent Behaviour in Inpatient Psychiatric Settings and Emergency Departments. London: Royal College of Nursing;2005.26. Milbrandt EB, Kersten A, Kong L, Weissfeld LA, Clermont G, Fink MP, et al. Haloperidol use is associated with lower hospital mortality in mechanically ventilated patients. Crit Care Med. 2005; 33:226–229. discussion 263-265
Article27. Dorey JM, Beauchet O, Thomas Antérion C, Rouch I, Krolak-Salmon P, Gaucher J, et al. Behavioral and psychological symptoms of dementia and bipolar spectrum disorders: review of the evidence of a relationship and treatment implications. CNS Spectr. 2008; 13:796–803.
Article28. Ballard CG, Gauthier S, Cummings JL, Brodaty H, Grossberg GT, Robert P, et al. Management of agitation and aggression associated with Alzheimer disease. Nat Rev Neurol. 2009; 5:245–255.
Article29. Gareri P, Cortoneo A, Marchisio U, Curcio M, De Sarro G. Risperidone in the treatment of behavioral disorders in elderly patients with dementia. Arch Gerontol Geriatr Suppl. 2001; 7:173–182.
Article30. Gareri P, Cotroneo A, Lacava R, Seminara G, Marigliano N, Loiacono A, et al. Comparison of the efficacy of new and conventional antipsychotic drugs in the treatment of behavioral and psychological symptoms of dementia (BPSD). Arch Gerontol Geriatr Suppl. 2004; (9):207–215.
Article31. De Deyn PP, Rabheru K, Rasmussen A, Bocksberger JP, Dautzenberg PL, Eriksson S, et al. A randomized trial of risperidone, placebo, and haloperidol for behavioral symptoms of dementia. Neurology. 1999; 53:946–955.
Article32. Teri L, Logsdon RG, Peskind E, Raskind M, Weiner MF, Tractenberg RE, et al. Treatment of agitation in AD: a randomized, placebo-controlled clinical trial. Neurology. 2000; 55:1271–1278.
Article33. Lonergan E, Luxenberg J, Colford J. Haloperidol for agitation in dementia. Cochrane Database Syst Rev. 2002; (2):CD002852.
Article34. Ballard C, Howard R. Neuroleptic drugs in dementia: benefits and harm. Nat Rev Neurosci. 2006; 7:492–500.
Article35. Schneider LS, Dagerman K, Insel PS. Efficacy and adverse effects of atypical antipsychotics for dementia: meta-analysis of randomized, placebo-controlled trials. Am J Geriatr Psychiatry. 2006; 14:191–210.
Article36. Schneider LS, Dagerman KS, Insel P. Risk of death with atypical antipsychotic drug treatment for dementia: meta-analysis of randomized placebo-controlled trials. JAMA. 2005; 294:1934–1943.
Article37. Ballard C, Lana MM, Theodoulou M, Douglas S, McShane R, Jacoby R, et al. A randomised, blinded, placebo-controlled trial in dementia patients continuing or stopping neuroleptics (the DART-AD trial). PLoS Med. 2008; 5:e76.
Article38. Schneider LS, Tariot PN, Dagerman KS, Davis SM, Hsiao JK, Ismail MS, et al. Effectiveness of atypical antipsychotic drugs in patients with Alzheimer's disease. N Engl J Med. 2006; 355:1525–1538.
Article39. Sultzer DL, Davis SM, Tariot PN, Dagerman KS, Lebowitz BD, Lyketsos CG, et al. Clinical symptom responses to atypical antipsychotic medications in Alzheimer's disease: phase 1 outcomes from the CATIE-AD effectiveness trial. Am J Psychiatry. 2008; 165:844–854.
Article40. Vigen CL, Mack WJ, Keefe RS, Sano M, Sultzer DL, Stroup TS, et al. Cognitive effects of atypical antipsychotic medications in patients with Alzheimer's disease: outcomes from CATIE-AD. Am J Psychiatry. 2011; 168:831–839.
Article41. Ballard C, Waite J. The effectiveness of atypical antipsychotics for the treatment of aggression and psychosis in Alzheimer's disease. Cochrane Database Syst Rev. 2006; (1):CD003476.42. Mowat D, Fowlie D, MacEwan T. CSM warning on atypical psychotics and stroke may be detrimental for dementia. BMJ. 2004; 328:1262.
Article43. Lee PE, Gill SS, Freedman M, Bronskill SE, Hillmer MP, Rochon PA. Atypical antipsychotic drugs in the treatment of behavioural and psychological symptoms of dementia: systematic review. BMJ. 2004; 329:75.
Article44. Liperoti R, Onder G, Landi F, Lapane KL, Mor V, Bernabei R, et al. All-cause mortality associated with atypical and conventional antipsychotics among nursing home residents with dementia: a retrospective cohort study. J Clin Psychiatry. 2009; 70:1340–1347.
Article45. Huybrechts KF, Gerhard T, Crystal S, Olfson M, Avorn J, Levin R, et al. Differential risk of death in older residents in nursing homes prescribed specific antipsychotic drugs: population based cohort study. BMJ. 2012; 344:e977.
Article46. Sacchetti E, Trifirò G, Caputi A, Turrina C, Spina E, Cricelli C, et al. Risk of stroke with typical and atypical anti-psychotics: a retrospective cohort study including unexposed subjects. J Psychopharmacol. 2008; 22:39–46.
Article47. Trifirò G, Verhamme KM, Ziere G, Caputi AP, Ch Stricker BH, Sturkenboom MC. All-cause mortality associated with atypical and typical antipsychotics in demented outpatients. Pharmacoepidemiol Drug Saf. 2007; 16:538–544.
Article48. Trifirò G, Spina E, Gambassi G. Use of antipsychotics in elderly patients with dementia: do atypical and conventional agents have a similar safety profile? Pharmacol Res. 2009; 59:1–12.
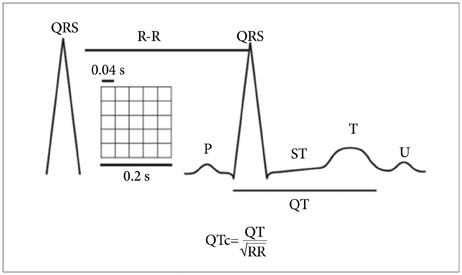
Article49. Haddad PM, Anderson IM. Antipsychotic-related QTc prolongation, torsade de pointes and sudden death. Drugs. 2002; 62:1649–1671.
Article50. Titier K, Girodet PO, Verdoux H, Molimard M, Bégaud B, Haverkamp W, et al. Atypical antipsychotics: from potassium channels to torsade de pointes and sudden death. Drug Saf. 2005; 28:35–51.51. Taylor DM. Antipsychotics and QT prolongation. Acta Psychiatr Scand. 2003; 107:85–95.
Article52. Reilly JG, Ayis SA, Ferrier IN, Jones SJ, Thomas SH. QTc-interval abnormalities and psychotropic drug therapy in psychiatric patients. Lancet. 2000; 355:1048–1052.
Article53. Thomas SH. Drugs, QT interval abnormalities and ventricular arrhythmias. Adverse Drug React Toxicol Rev. 1994; 13:77–102.54. De Ponti F, Poluzzi E, Montanaro N. QT-interval prolongation by non-cardiac drugs: lessons to be learned from recent experience. Eur J Clin Pharmacol. 2000; 56:1–18.
Article55. Ray WA, Meredith S, Thapa PB, Meador KG, Hall K, Murray KT. Antipsychotics and the risk of sudden cardiac death. Arch Gen Psychiatry. 2001; 58:1161–1167.
Article56. Alvarez PA, Pahissa J. QT alterations in psychopharmacology: proven candidates and suspects. Curr Drug Saf. 2010; 5:97–104.
Article57. Glassman AH, Bigger JT Jr. Antipsychotic drugs: prolonged QTc interval, torsade de pointes, and sudden death. Am J Psychiatry. 2001; 158:1774–1782.
Article58. Chung AK, Chua SE. Effects on prolongation of Bazett's corrected QT interval of seven second-generation antipsychotics in the treatment of schizophrenia: a meta-analysis. J Psychopharmacol. 2011; 25:646–666.
Article59. Zareba W, Lin DA. Antipsychotic drugs and QT interval prolongation. Psychiatr Q. 2003; 74:291–306.60. Liperoti R, Gambassi G, Lapane KL, Chiang C, Pedone C, Mor V, et al. Conventional and atypical antipsychotics and the risk of hospitalization for ventricular arrhythmias or cardiac arrest. Arch Intern Med. 2005; 165:696–701.
Article61. Pariente A, Fourrier-Réglat A, Ducruet T, Farrington P, Béland SG, Dartigues JF, et al. Antipsychotic use and myocardial infarction in older patients with treated dementia. Arch Intern Med. 2012; 172:648–653. discussion 654-655
Article62. Alexopoulos GS, Streim J, Carpenter D, Docherty JP. Expert Consensus Panel for Using Antipsychotic Drugs in Older Patients. Using antipsychotic agents in older patients. J Clin Psychiatry. 2004; 65:Suppl 2. 5–99. discussion 100-102; quiz 103-10463. Gill SS, Rochon PA, Herrmann N, Lee PE, Sykora K, Gunraj N, et al. Atypical antipsychotic drugs and risk of ischaemic stroke: population based retrospective cohort study. BMJ. 2005; 330:445.
Article64. Liperoti R, Gambassi G, Lapane KL, Chiang C, Pedone C, Mor V, et al. Cerebrovascular events among elderly nursing home patients treated with conventional or atypical antipsychotics. J Clin Psychiatry. 2005; 66:1090–1096.
Article65. Douglas IJ, Smeeth L. Exposure to antipsychotics and risk of stroke: self controlled case series study. BMJ. 2008; 337:a1227.
Article66. Herrmann N, Lanctôt KL. Do atypical antipsychotics cause stroke? CNS Drugs. 2005; 19:91–103.
Article67. Tarsy D, Baldessarini RJ, Tarazi FI. Effects of newer antipsychotics on extrapyramidal function. CNS Drugs. 2002; 16:23–45.
Article68. Weiden PJ. EPS profiles: the atypical antipsychotics are not all the same. J Psychiatr Pract. 2007; 13:13–24.69. Wirshing WC. Movement disorders associated with neuroleptic treatment. J Clin Psychiatry. 2001; 62:Suppl 21. 15–18.70. Orr MW, Knox JM, Allen R, Gelder MG, Grahame-Smith DG. The effects of neuroleptic drugs on 5-hydroxytryptamine induced platelet aggregation in schizophrenic patients. Br J Clin Pharmacol. 1981; 11:255–259.
Article71. Mulsant BH, Gharabawi GM, Bossie CA, Mao L, Martinez RA, Tune LE, et al. Correlates of anticholinergic activity in patients with dementia and psychosis treated with risperidone or olanzapine. J Clin Psychiatry. 2004; 65:1708–1714.
Article72. Wetterling T. Bodyweight gain with atypical antipsychotics. A comparative review. Drug Saf. 2001; 24:59–73.73. Allison DB, Mentore JL, Heo M, Chandler LP, Cappelleri JC, Infante MC, et al. Antipsychotic-induced weight gain: a comprehensive research synthesis. Am J Psychiatry. 1999; 156:1686–1696.74. Ananth J, Venkatesh R, Burgoyne K, Gadasalli R, Binford R, Gunatilake S. Atypical antipsychotic induced weight gain: pathophysiology and management. Ann Clin Psychiatry. 2004; 16:75–85.
Article75. Buse JB, Cavazzoni P, Hornbuckle K, Hutchins D, Breier A, Jovanovic L. A retrospective cohort study of diabetes mellitus and antipsychotic treatment in the United States. J Clin Epidemiol. 2003; 56:164–170.
Article76. Cohen D. Atypical antipsychotics and new onset diabetes mellitus. An overview of the literature. Pharmacopsychiatry. 2004; 37:1–11.77. Wirshing DA, Spellberg BJ, Erhart SM, Marder SR, Wirshing WC. Novel antipsychotics and new onset diabetes. Biol Psychiatry. 1998; 44:778–783.
Article78. Mukherjee S, Decina P, Bocola V, Saraceni F, Scapicchio PL. Diabetes mellitus in schizophrenic patients. Compr Psychiatry. 1996; 37:68–73.
Article79. Gaulin BD, Markowitz JS, Caley CF, Nesbitt LA, Dufresne RL. Clozapine-associated elevation in serum triglycerides. Am J Psychiatry. 1999; 156:1270–1272.80. Wirshing DA, Boyd JA, Meng LR, Ballon JS, Marder SR, Wirshing WC. The effects of novel antipsychotics on glucose and lipid levels. J Clin Psychiatry. 2002; 63:856–865.
Article81. Wu RR, Zhao JP, Liu ZN, Zhai JG, Guo XF, Guo WB, et al. Effects of typical and atypical antipsychotics on glucose-insulin homeostasis and lipid metabolism in first-episode schizophrenia. Psychopharmacology (Berl). 2006; 186:572–578.
Article82. Koro CE, Fedder DO, L'Italien GJ, Weiss S, Magder LS, Kreyenbuhl J, et al. An assessment of the independent effects of olanzapine and risperidone exposure on the risk of hyperlipidemia in schizophrenic patients. Arch Gen Psychiatry. 2002; 59:1021–1026.
Article83. Rondanelli M, Sarra S, Antoniello N, Mansi V, Govoni S, Falvo F, et al. No effect of atypical antipsychotic drugs on weight gain and risk of developing type II diabetes or lipid abnormalities among nursing home elderly patients with Alzheimer's disease. Minerva Med. 2006; 97:147–151.84. Sicras-Mainar A, Blanca-Tamayo M, Rejas-Gutiérrez J, Navarro-Artieda R. Metabolic syndrome in outpatients receiving antipsychotic therapy in routine clinical practice: a cross-sectional assessment of a primary health care database. Eur Psychiatry. 2008; 23:100–108.
Article85. Rettenbacher MA, Hofer A, Kemmler G, Fleischhacker WW. Neutropenia induced by second generation antipsychotics: a prospective investigation. Pharmacopsychiatry. 2010; 43:41–44.
Article86. Croarkin P, Rayner T. Acute neutropenia in a patient treated with quetiapine. Psychosomatics. 2001; 42:368.
Article87. Li X, Cameron MD. Potential role of a quetiapine metabolite in quetiapine-induced neutropenia and agranulocytosis. Chem Res Toxicol. 2012; 25:1004–1011.
Article88. Trifirò G, Gambassi G, Sen EF, Caputi AP, Bagnardi V, Brea J, et al. Association of community-acquired pneumonia with antipsychotic drug use in elderly patients: a nested case-control study. Ann Intern Med. 2010; 152:418–425. W139–W140.
Article89. Parker C, Coupland C, Hippisley-Cox J. Antipsychotic drugs and risk of venous thromboembolism: nested case-control study. BMJ. 2010; 341:c4245.
Article90. Allenet B, Schmidlin S, Genty C, Bosson JL. Antipsychotic drugs and risk of pulmonary embolism. Pharmacoepidemiol Drug Saf. 2012; 21:42–48.
Article91. Kleijer BC, Heerdink ER, Egberts TC, Jansen PA, van Marum RJ. Antipsychotic drug use and the risk of venous thromboembolism in elderly patients. J Clin Psychopharmacol. 2010; 30:526–530.
Article92. Axelsson S, Hägg S, Eriksson AC, Lindahl TL, Whiss PA. In vitro effects of antipsychotics on human platelet adhesion and aggregation and plasma coagulation. Clin Exp Pharmacol Physiol. 2007; 34:775–780.
Article93. Haddad PM, Wieck A. Antipsychotic-induced hyperprolactinaemia: mechanisms, clinical features and management. Drugs. 2004; 64:2291–2314.94. Kinon BJ, Gilmore JA, Liu H, Halbreich UM. Hyperprolactinemia in response to antipsychotic drugs: characterization across comparative clinical trials. Psychoneuroendocrinology. 2003; 28:Suppl 2. 69–82.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Prescribing Patterns of Antipsychotic Drugs and Antiparkinsonian Drugs in Elderly Patients with Dementia
- Late-life Schizophrenia
- Using Atypical Antipsychotics in Patients with Dementia
- Brain Neurologic Disorder and Depression in Elderly
- Repetitive and Stereotypic Vocalization in Dementia after Using Antipsychotics