Dement Neurocogn Disord.
2016 Dec;15(4):170-173. 10.12779/dnd.2016.15.4.170.
Neurosyphilis Mimicking Creutzfeldt-Jakob Disease
- Affiliations
-
- 1Department of Neurology, Kangwon National University Hospital, Chuncheon, Korea.
- 2Department of Neurology, Seoul National University College of Medicine, Clinical Neuroscience Center, Seoul National University Bundang Hospital, Seongnam, Korea. neuroksy@snu.ac.kr
- KMID: 2442845
- DOI: http://doi.org/10.12779/dnd.2016.15.4.170
Abstract
- BACKGROUND
As rapidly progressive dementia (RPD), general paresis and Creutzfeldt-Jakob disease (CJD) may have overlapping clinical presentation due to a wide variety of clinical manifestations.
CASE REPORT
A 57-year-old man presented with rapid progressive cognitive decline, behavioral change, ataxic gait, tremor and pyramidal signs for 3 months. In addition to these multiple systemic involvements, positive result for the cerebrospinal fluid (CSF) 14-3-3 protein tentatively diagnosed him as probable CJD. However, due to increased serum rapid plasma reagin, venereal disease research laboratory, and fluorescent treponemal antibody-absorption reactivity in CSF, the final diagnosis was changed to general paresis.
CONCLUSIONS
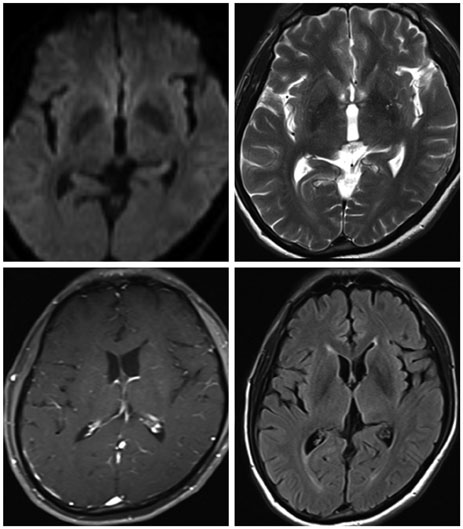
A patient with RPD needs to be carefully considered for differential diagnosis, among a long list of diseases. It is important to rule out CJD, which is the most frequent in RPD and is a fatal disease with no cure. Diagnostic criteria or marker of CJD, such as 14-3-3 protein, may be inconclusive, and a typical pattern in diffusion-weighted imaging is important to rule out other reversible diseases.
MeSH Terms
Figure
Reference
-
1. Ghanem KG. REVIEW: neurosyphilis: a historical perspective and review. CNS Neurosci Ther. 2010; 16:e157–e168.
Article2. Bradley WG. Neurology in clinical practice: principles of diagnosis and management. 4th ed. Philadelphia: Taylor & Francis;2004.
Article3. Brown P, Gibbs CJ Jr, Rodgers-Johnson P, Asher DM, Sulima MP, Bacote A, et al. Human spongiform encephalopathy: the National Institutes of Health series of 300 cases of experimentally transmitted disease. Ann Neurol. 1994; 35:513–529.
Article4. Stefani A, Riello M, Rossini F, Mariotto S, Fenzi F, Gambina G, et al. Neurosyphilis manifesting with rapidly progressive dementia: report of three cases. Neurol Sci. 2013; 34:2027–2030.
Article5. Jantzen SU, Ferrea S, Langebner T, Gaebel W, Griese M, Arendt G, et al. Late-stage neurosyphilis presenting with severe neuropsychiatric deficits: diagnosis, therapy, and course of three patients. J Neurol. 2012; 259:720–728.
Article6. Zheng D, Zhou D, Zhao Z, Liu Z, Xiao S, Xing Y, et al. The clinical presentation and imaging manifestation of psychosis and dementia in general paresis: a retrospective study of 116 cases. J Neuropsychiatry Clin Neurosci. 2011; 23:300–307.
Article7. The National CJD Research & Surveillance Unit (NCJDRSU, formerly NCJDSU). National Creutzfeldt-Jakob disease Surveillance Diagnositic Criteria. cited 2016 Nov 15. Available from: http://www.cjd.ed.ac.uk/documents/criteria.pdf.
Article8. Zerr I, Pocchiari M, Collins S, Brandel JP, de Pedro Cuesta J, Knight RS, et al. Analysis of EEG and CSF 14-3-3 proteins as aids to the diagnosis of Creutzfeldt-Jakob disease. Neurology. 2000; 55:811–815.
Article9. Sanchez-Juan P, Green A, Ladogana A, Cuadrado-Corrales N, Saanchez-Valle R, Mitrovaa E, et al. CSF tests in the differential diagnosis of Creutzfeldt-Jakob disease. Neurology. 2006; 67:637–643.
Article10. Satoh J, Kurohara K, Yukitake M, Kuroda Y. The 14-3-3 protein detectable in the cerebrospinal fluid of patients with prion-unrelated neurological diseases is expressed constitutively in neurons and glial cells in culture. Eur Neurol. 1999; 41:216–225.
Article11. Jang JW, Park YH, Lim JS, Park SC, Cheong HK, Kim JE, et al. Neurologists' awareness and preparedness on prion diseases in Korea. Dement Neurocognitive Disord. 2013; 12:9–20.
Article12. Nagappa M, Sinha S, Taly AB, Rao SL, Nagarathna S, Bindu PS, et al. Neurosyphilis: MRI features and their phenotypic correlation in a cohort of 35 patients from a tertiary care university hospital. Neuroradiology. 2013; 55:379–388.
Article13. Park SY, Wang MJ, Jang JW, Park YH, Lim JS, Youn YC, et al. The clinical stages of sporadic Creutzfeldt-Jakob disease with Met/Met genotype in Korean patients. Eur Neurol. 2016; 75:213–222.
Article14. Vitali P, Maccagnano E, Caverzasi E, Henry RG, Haman A, Torres-Chae C, et al. Diffusion-weighted MRI hyperintensity patterns differentiate CJD from other rapid dementias. Neurology. 2011; 76:1711–1719.
Article15. Zerr I, Kallenberg K, Summers DM, Romero C, Taratuto A, Heinemann U, et al. Updated clinical diagnostic criteria for sporadic Creutzfeldt-Jakob disease. Brain. 2009; 132(Pt 10):2659–2668.
Article16. Wang J, Guo Q, Zhou P, Zhang J, Zhao Q, Hong Z. Cognitive impairment in mild general paresis of the insane: AD-like pattern. Dement Geriatr Cogn Disord. 2011; 31:284–290.
Article17. Hama K, Ishiguchi H, Tuji T, Miwa H, Kondo T. Neurosyphilis with mesiotemporal magnetic resonance imaging abnormalities. Intern Med. 2008; 47:1813–1817.
Article18. Choe HS, Lee DS, Lee SJ, Lee CB, Lee WC, Cho YH. Prevalence of sexually transmitted infections and sexual behavior of young adults and middle-aged people presenting to health examination centers in Korea. J Infect Chemother. 2012; 18:207–212.
Article19. Marra CM. Update on neurosyphilis. Curr Infect Dis Rep. 2009; 11:127–134.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Neurosyphilis Mimicking Limbic Encephalitis and Creutzfeldt-Jakob Disease
- A case of Creutzfeldt-Jakob disease
- Creutzfeldt-Jakob Disease Mimicking a Stroke as Initial Manifestation
- New Variant Creutzfeldt-Jakob Disease
- A Case of Probable Creutzfeldt-Jakob Disease with Coexistence of the Features of Hashimoto Encephalopathy