J Cardiovasc Imaging.
2019 Apr;27(2):105-118. 10.4250/jcvi.2019.27.e19.
Mid-term Clinical Outcomes in a Cohort of Asymptomatic or Mildly Symptomatic Korean Patients with Bicuspid Aortic Valve in a Tertiary Referral Hospital
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Chungnam National University Hospital, Chungnam National University School of Medicine, Daejeon, Korea.
- 2Valvular Heart Disease Center, Asan Medical Center Heart Institute, University of Ulsan College of Medicine, Seoul, Korea. jksong@amc.seoul.kr
- 3Research Institute for Valvular Heart Disease, University of Ulsan College of Medicine, Seoul, Korea.
- 4Division of Cardiology, Department of Internal Medicine, Gyeongsang National University School of Medicine, Gyeongsang National University Changwon Hospital, Changwon, Korea.
- KMID: 2442744
- DOI: http://doi.org/10.4250/jcvi.2019.27.e19
Abstract
- BACKGROUND
Although bicuspid aortic valve (BAV) is one of the most common congenital heart diseases, clinical outcome data regarding BAV are still limited. We evaluated clinical characteristics and mid-term clinical outcomes of asymptomatic Korean patients with bicuspid aortic valve.
METHODS
We initiated a prospective registry in 2014 at a tertiary referral hospital. To develop a cohort of asymptomatic patients, we excluded patients who previously underwent open heart surgery (OHS) or who had OHS within 6 months of referral.
RESULTS
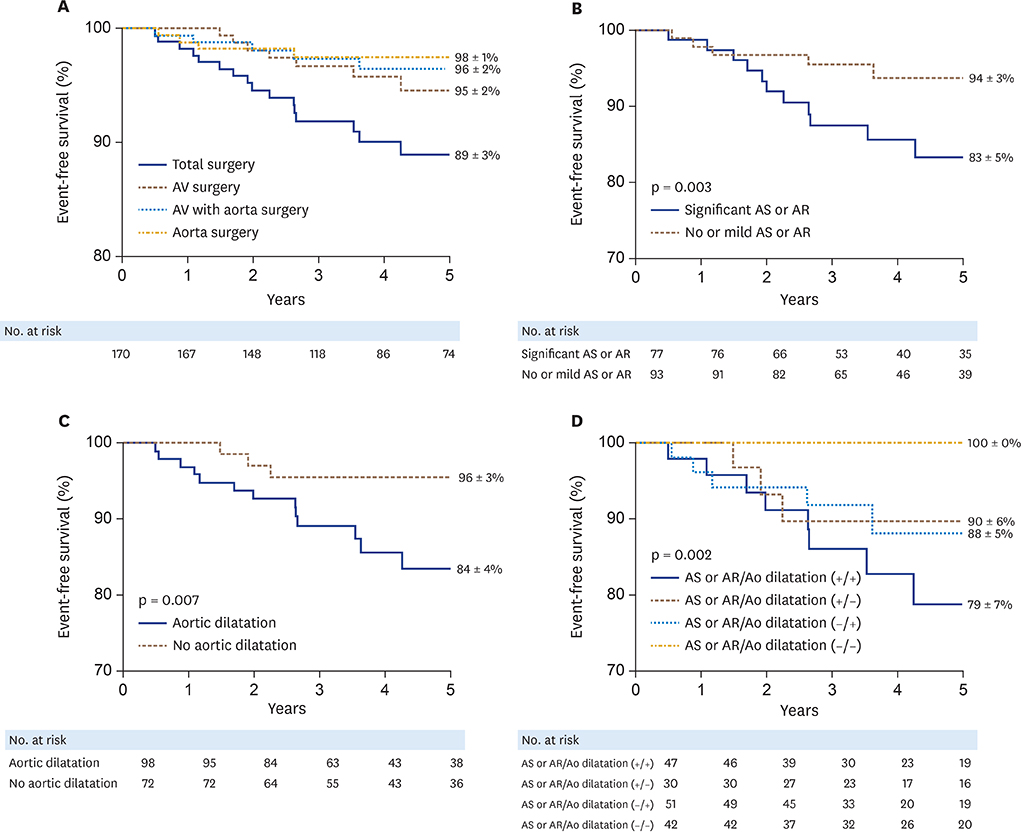
A total of 170 patients (117 male [69%], age 50 ± 13 years) were enrolled. More than 70% (n = 124, 73%) were incidentally diagnosed with BAV during routine health examinations or preoperative screening for non-cardiac surgery. At the time of enrollment, moderate to severe aortic stenosis (AS) or regurgitation (AR) was present in 77 patients (45%) and 98 (58%) showed aortic dilation: 42 (25%) had non-significant valvular dysfunction without aortic dilation. During a median follow-up of 4 years, AS severity increased significantly (p < 0.001), while there was no significant change in AR severity (p = 0.361). A total of 27 patients (16%) underwent OHS, including isolated aortic valve (AV) surgery (n = 11, 41%), AV with combined aortic surgery (n = 12, 44%), and isolated aortic surgery (n = 4, 15%): no patient developed aortic dissection. Moderate to severe AS (hazard ratio [HR] 4.61; 95% confidence interval [CI] 1.83-11.62; p = 0.001), NYHA class ≥ 2 (HR 2.53; 95% CI 1.01-6.35; p = 0.048) and aortic dilation (HR 2.13; 95% CI 0.87-5.21; p = 0.099) were associated with surgical events.
CONCLUSIONS
Progression patterns of valvular dysfunction and impacts of BAV phenotype on OHS should be explored in future studies with longer follow-up durations.
MeSH Terms
Figure
Cited by 1 articles
-
Understanding the Natural History of Bicuspid Aortic Valve: Are We Close to Understanding It?
Seung-Pyo Lee
J Cardiovasc Imaging. 2019;27(2):119-121. doi: 10.4250/jcvi.2019.27.e21.
Reference
-
1. Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics--2011 update: a report from the American Heart Association. Circulation. 2011; 123:e18–e209.2. Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol. 2002; 39:1890–1900.
Article3. Song JK. Bicuspid aortic valve: unresolved issues and role of imaging specialists. J Cardiovasc Ultrasound. 2015; 23:1–7.
Article4. Verma S, Siu SC. Aortic dilatation in patients with bicuspid aortic valve. N Engl J Med. 2014; 370:1920–1929.
Article5. Michelena HI, Prakash SK, Della Corte A, et al. Bicuspid aortic valve: identifying knowledge gaps and rising to the challenge from the International Bicuspid Aortic Valve Consortium (BAVCon). Circulation. 2014; 129:2691–2704.6. Michelena HI, Khanna AD, Mahoney D, et al. Incidence of aortic complications in patients with bicuspid aortic valves. JAMA. 2011; 306:1104–1112.
Article7. Tzemos N, Therrien J, Yip J, et al. Outcomes in adults with bicuspid aortic valves. JAMA. 2008; 300:1317–1325.
Article8. Michelena HI, Desjardins VA, Avierinos JF, et al. Natural history of asymptomatic patients with normally functioning or minimally dysfunctional bicuspid aortic valve in the community. Circulation. 2008; 117:2776–2784.
Article9. Prakash SK, Bossé Y, Muehlschlegel JD, et al. A roadmap to investigate the genetic basis of bicuspid aortic valve and its complications: insights from the International BAVCon (Bicuspid Aortic Valve Consortium). J Am Coll Cardiol. 2014; 64:832–839.10. Sun BJ, Lee S, Jang JY, et al. Performance of a simplified dichotomous phenotypic classification of bicuspid aortic valve to predict type of valvulopathy and combined aortopathy. J Am Soc Echocardiogr. 2017; 30:1152–1161.
Article11. Jilaihawi H, Chen M, Webb J, et al. A bicuspid aortic valve imaging classification for the TAVR era. JACC Cardiovasc Imaging. 2016; 9:1145–1158.12. Sievers HH, Schmidtke C. A classification system for the bicuspid aortic valve from 304 surgical specimens. J Thorac Cardiovasc Surg. 2007; 133:1226–1233.
Article13. Sun BJ, Jin X, Song JK, et al. Clinical characteristics of Korean patients with bicuspid aortic valve who underwent aortic valve surgery. Korean Circ J. 2018; 48:48–58.
Article14. Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014; 129:e521–e643.
Article15. National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002; 39:S1–266.16. Baumgartner H, Hung J, Bermejo J, et al. Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice. Eur J Echocardiogr. 2009; 10:1–25.
Article17. Zoghbi WA, Enriquez-Sarano M, Foster E, et al. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr. 2003; 16:777–802.
Article18. Borger MA, Fedak PWM, Stephens EH, et al. The American Association for Thoracic Surgery consensus guidelines on bicuspid aortic valve-related aortopathy: Full online-only version. J Thorac Cardiovasc Surg. 2018; 156:e41–74.
Article19. Gharibeh L, Komati H, Bossé Y, et al. GATA6 regulates aortic valve remodeling, and its haploinsufficiency leads to right-left type bicuspid aortic valve. Circulation. 2018; 138:1025–1038.
Article20. Michelena HI, Suri RM, Katan O, et al. Sex differences and survival in adults with bicuspid aortic valves: verification in 3 contemporary echocardiographic cohorts. J Am Heart Assoc. 2016; 5:e004211.
Article21. Pepe G, De Cario R, Sticchi E, et al. Bicuspid aortic valve syndrome and fibrillinopathies: potential impact on clinical approach. Int Cardiovasc Forum J. 2015; 1:167–174.
Article22. Galian-Gay L, Carro Hevia A, Teixido-Turà G, et al. Familial clustering of bicuspid aortic valve and its relationship with aortic dilation in first-degree relatives. Heart. 2018; 10. 15. [E-pub ahead of print], https://doi.org/10.1136/heartjnl-2018-313802.
Article23. Niaz T, Poterucha JT, Johnson JN, et al. Incidence, morphology, and progression of bicuspid aortic valve in pediatric and young adult subjects with coexisting congenital heart defects. Congenit Heart Dis. 2017; 12:261–269.
Article24. Kong WKF, Regeer MV, Poh KK, et al. Inter-ethnic differences in valve morphology, valvular dysfunction, and aortopathy between Asian and European patients with bicuspid aortic valve. Eur Heart J. 2018; 39:1308–1313.
Article25. Kong WK, Delgado V, Poh KK, et al. Prognostic implications of raphe in bicuspid aortic valve anatomy. JAMA Cardiol. 2017; 2:285–292.
Article26. Kang JW, Song HG, Yang DH, et al. Association between bicuspid aortic valve phenotype and patterns of valvular dysfunction and bicuspid aortopathy: comprehensive evaluation using MDCT and echocardiography. JACC Cardiovasc Imaging. 2013; 6:150–161.27. Schaefer BM, Lewin MB, Stout KK, et al. The bicuspid aortic valve: an integrated phenotypic classification of leaflet morphology and aortic root shape. Heart. 2008; 94:1634–1638.
Article28. Fernandes SM, Sanders SP, Khairy P, et al. Morphology of bicuspid aortic valve in children and adolescents. J Am Coll Cardiol. 2004; 44:1648–1651.
Article29. Kinoshita T, Naito S, Suzuki T, Asai T. Valve phenotype and risk factors of aortic dilatation after aortic valve replacement in Japanese patients with bicuspid aortic valve. Circ J. 2016; 80:1356–1361.
Article30. Fernández B, Durán AC, Fernández-Gallego T, et al. Bicuspid aortic valves with different spatial orientations of the leaflets are distinct etiological entities. J Am Coll Cardiol. 2009; 54:2312–2318.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Ascending Aortic Aneurysm Associated with Congenital Bicuspid Aortic Valve
- Comparable Outcomes of Bicuspid Aortic Valves for RapidDeployment Aortic Valve Replacement
- Exercise Echocardiography in Asymptomatic Patients with Severe Aortic Stenosis and Preserved Left Ventricular Ejection Fraction
- Bicuspid Aortic Valve: Unresolved Issues and Role of Imaging Specialists
- A Case of Double Orifice Mitral Valve in a Patient with Bicuspid Aortic Valve: Coincidental or a Missed Finding?