Korean J Radiol.
2019 May;20(5):739-748. 10.3348/kjr.2018.0809.
Current Opinion on Endovascular Therapy for Emergent Large Vessel Occlusion Due to Underlying Intracranial Atherosclerotic Stenosis
- Affiliations
-
- 1Department of Neurosurgery, School of Medicine, Kyungpook National University, Daegu, Korea.
- 2Department of Radiology, School of Medicine, Kyungpook National University, Daegu, Korea.
- 3Department of Radiology, Chonnam National University Medical School, Gwangju, Korea. radyoon@jnu.ac.kr
- KMID: 2442708
- DOI: http://doi.org/10.3348/kjr.2018.0809
Abstract
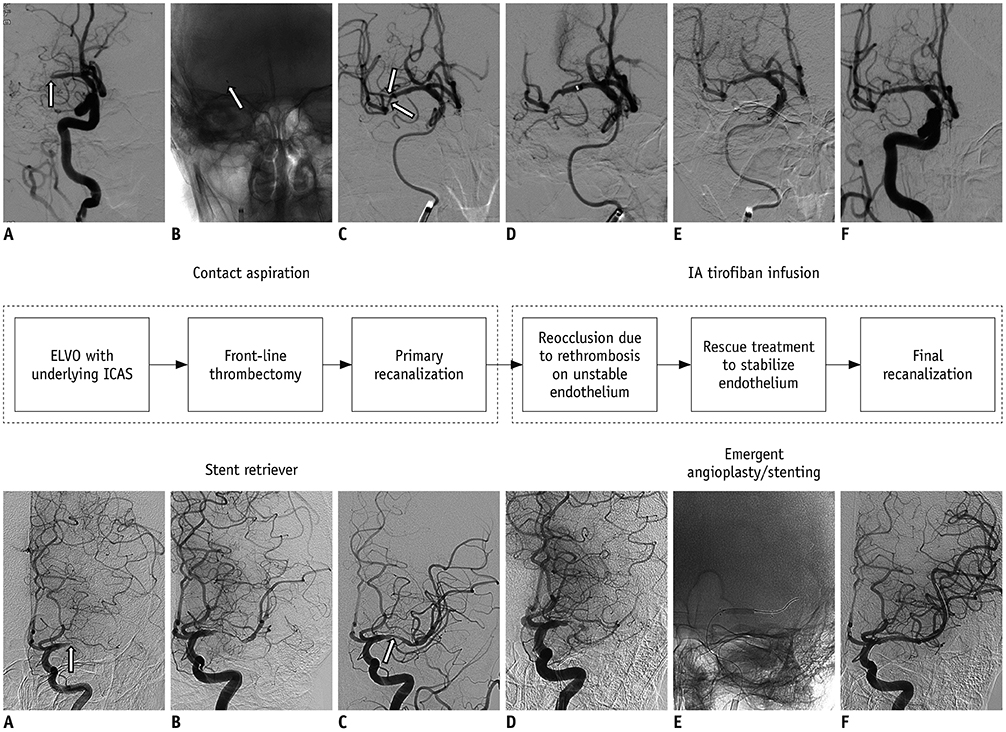
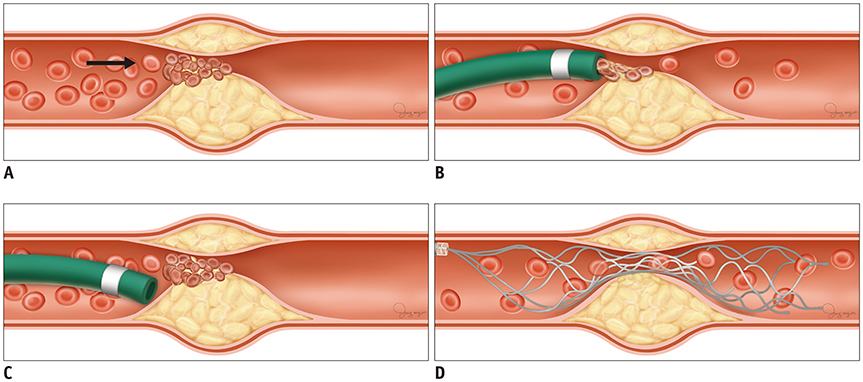
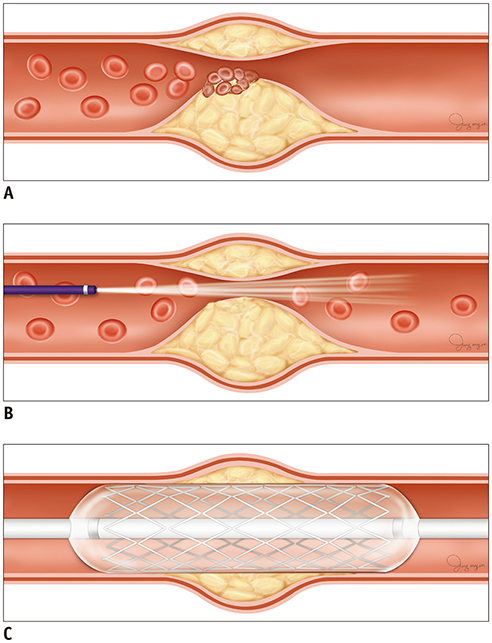
- For recanalization of emergent large vessel occlusions (ELVOs), endovascular therapy (EVT) using newer devices, such as a stent retriever and large-bore catheter, has shown better patient outcomes compared with intravenous recombinant tissue plasminogen activator only. Intracranial atherosclerotic stenosis (ICAS) is a major cause of acute ischemic stroke, the incidence of which is rising worldwide. Thus, it is not rare to encounter underlying ICAS during EVT procedures, particularly in Asian countries. ELVO due to underlying ICAS is often related to EVT procedure failure or complications, which can lead to poor functional recovery. However, information regarding EVT for this type of stroke is lacking because large clinical trials have been largely based on Western populations. In this review, we discuss the unique pathologic basis of ELVO with underlying ICAS, which may complicate EVT procedures. Moreover, we review EVT data for patients with ELVO due to underlying ICAS and suggest an optimal endovascular recanalization strategy based on the existing literature. Finally, we present future perspectives on this subject.
Keyword
MeSH Terms
Figure
Reference
-
1. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995; 333:1581–1588.2. Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et al. ECASS Investigators. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008; 359:1317–1329.
Article3. Bhatia R, Hill MD, Shobha N, Menon B, Bal S, Kochar P, et al. Low rates of acute recanalization with intravenous recombinant tissue plasminogen activator in ischemic stroke: real-world experience and a call for action. Stroke. 2010; 41:2254–2258.4. del Zoppo GJ, Poeck K, Pessin MS, Wolpert SM, Furlan AJ, Ferbert A, et al. Recombinant tissue plasminogen activator in acute thrombotic and embolic stroke. Ann Neurol. 1992; 32:78–86.
Article5. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. MR CLEAN Investigators. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015; 372:11–20.6. Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. EXTEND-IA Investigators. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015; 372:1009–1018.7. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. ESCAPE Trial Investigators. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; 372:1019–1030.8. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. REVASCAT Trial Investigators. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015; 372:2296–2306.
Article9. Kim YD, Cha MJ, Kim J, Lee DH, Lee HS, Nam CM, et al. Increases in cerebral atherosclerosis according to CHADS2 scores in patients with stroke with nonvalvular atrial fibrillation. Stroke. 2011; 42:930–934.10. Bang OY. Intracranial atherosclerosis: current understanding and perspectives. J Stroke. 2014; 16:27–35.
Article11. Gorelick PB, Wong KS, Bae HJ, Pandey DK. Large artery intracranial occlusive disease: a large worldwide burden but a relatively neglected frontier. Stroke. 2008; 39:2396–2399.12. Libby P. Inflammation in atherosclerosis. Nature. 2002; 420:868–874.
Article13. Kim JS, Bonovich D. Research on intracranial atherosclerosis from the East and West: why are the results different? J Stroke. 2014; 16:105–113.
Article14. Kim BM. Causes and solutions of endovascular treatment failure. J Stroke. 2017; 19:131–142.
Article15. Hwang YH, Kim YW, Kang DH, Kim YS, Liebeskind DS. Impact of target arterial residual stenosis on outcome after endovascular revascularization. Stroke. 2016; 47:1850–1857.
Article16. Leung SY, Ng TH, Yuen ST, Lauder IJ, Ho FC. Pattern of cerebral atherosclerosis in Hong Kong Chinese. Severity in intracranial and extracranial vessels. Stroke. 1993; 24:779–786.
Article17. Wang Y, Zhao X, Liu L, Soo YO, Pu Y, Pan Y, et al. CICAS Study Group. Prevalence and outcomes of symptomatic intracranial large artery stenoses and occlusions in China: the Chinese Intracranial Atherosclerosis (CICAS) study. Stroke. 2014; 45:663–669.18. White H, Boden-Albala B, Wang C, Elkind MS, Rundek T, Wright CB, et al. Ischemic stroke subtype incidence among Whites, Blacks, and Hispanics: the Northern Manhattan Study. Circulation. 2005; 111:1327–1331.19. Lee JS, Hong JM, Lee KS, Suh HI, Demchuk AM, Hwang YH, et al. Endovascular therapy of cerebral arterial occlusions: intracranial atherosclerosis versus embolism. J Stroke Cerebrovasc Dis. 2015; 24:2074–2080.
Article20. Yoon W, Kim SK, Park MS, Kim BC, Kang HK. Endovascular treatment and the outcomes of atherosclerotic intracranial stenosis in patients with hyperacute stroke. Neurosurgery. 2015; 76:680–686. discussion 686.
Article21. Kang DH, Kim YW, Hwang YH, Park SP, Kim YS, Baik SK. Instant reocclusion following mechanical thrombectomy of in situ thromboocclusion and the role of low-dose intra-arterial tirofiban. Cerebrovasc Dis. 2014; 37:350–355.
Article22. Kim YW, Hong JM, Park DG, Choi JW, Kang DH, Kim YS, et al. Effect of intracranial atherosclerotic disease on endovascular treatment for patients with acute vertebrobasilar occlusion. AJNR Am J Neuroradiol. 2016; 37:2072–2078.
Article23. Kim SJ, Ryoo S, Kim GM, Chung CS, Lee KH, Bang OY. Clinical and radiological outcomes after intracranial atherosclerotic stroke: a comprehensive approach comparing stroke subtypes. Cerebrovasc Dis. 2011; 31:427–434.
Article24. Kim SJ, Seok JM, Bang OY, Kim GM, Kim KH, Jeon P, et al. MR mismatch profiles in patients with intracranial atherosclerotic stroke: a comprehensive approach comparing stroke subtypes. J Cereb Blood Flow Metab. 2009; 29:1138–1145.
Article25. Turan TN, Cotsonis G, Lynn MJ, Chaturvedi S, Chimowitz M. Warfarin-Aspirin Symptomatic Intracranial Disease (WASID) Trial Investigators. Relationship between blood pressure and stroke recurrence in patients with intracranial arterial stenosis. Circulation. 2007; 115:2969–2975.
Article26. Ross R. Cell biology of atherosclerosis. Annu Rev Physiol. 1995; 57:791–804.
Article27. Velican C, Velican D. Atherosclerotic involvement of human intracranial arteries with special reference to intimal necrosis. Atherosclerosis. 1982; 43:59–69.
Article28. Velican C, Anghelescu M, Velican D. Preliminary study on the natural history of cerebral atherosclerosis. Med Interne. 1981; 19:137–145.29. Chimowitz MI, Lynn MJ, Howlett-Smith H, Stern BJ, Hertzberg VS, Frankel MR, et al. Warfarin-Aspirin Symptomatic Intracranial Disease Trial Investigators. Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med. 2005; 352:1305–1316.
Article30. Chimowitz MI, Lynn MJ, Derdeyn CP, Turan TN, Fiorella D, Lane BF, et al. SAMMPRIS Trial Investigators. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011; 365:993–1003.31. Lee JS, Hong JM, Kim JS. Diagnostic and therapeutic strategies for acute intracranial atherosclerosis-related occlusions. J Stroke. 2017; 19:143–151.
Article32. Kim SK, Yoon W, Kim TS, Kim HS, Heo TW, Park MS. Histologic analysis of retrieved clots in acute ischemic stroke: correlation with stroke etiology and gradient-echo MRI. AJNR Am J Neuroradiol. 2015; 36:1756–1762.
Article33. Chen XY, Wong KS, Lam WW, Zhao HL, Ng HK. Middle cerebral artery atherosclerosis: histological comparison between plaques associated with and not associated with infarct in a postmortem study. Cerebrovasc Dis. 2008; 25:74–80.
Article34. Suh HI, Hong JM, Lee KS, Han M, Choi JW, Kim JS, et al. Imaging predictors for atherosclerosis-related intracranial large artery occlusions in acute anterior circulation stroke. J Stroke. 2016; 18:352–354.
Article35. Cho KH, Kim JS, Kwon SU, Cho AH, Kang DW. Significance of susceptibility vessel sign on T2*-weighted gradient echo imaging for identification of stroke subtypes. Stroke. 2005; 36:2379–2383.
Article36. Cho KH, Yoon Y, Sohn SI, Kim JS. Susceptibility vessel signs on T2*-weighted gradient echo images in patients with cerebral atherosclerosis. Int J Stroke. 2014; 9:E32.
Article37. Lee JS, Hong JM, Lee KS, Suh HI, Choi JW, Kim SY. Primary stent retrieval for acute intracranial large artery occlusion due to atherosclerotic disease. J Stroke. 2016; 18:96–101.
Article38. Baek JH, Kim BM, Kim DJ, Heo JH, Nam HS, Song D, et al. Importance of truncal-type occlusion in stentriever-based thrombectomy for acute stroke. Neurology. 2016; 87:1542–1550.
Article39. Manning NW, Chapot R, Meyers PM. Endovascular stroke management: key elements of success. Cerebrovasc Dis. 2016; 42:170–177.
Article40. Yoon W, Kim SK, Park MS, Baek BH, Lee YY. Predictive factors for good outcome and mortality after stent-retriever thrombectomy in patients with acute anterior circulation stroke. J Stroke. 2017; 19:97–103.
Article41. Lapergue B, Blanc R, Gory B, Labreuche J, Duhamel A, Marnat G, et al. ASTER Trial Investigators. Effect of endovascular contact aspiration vs stent retriever on revascularization in patients with acute ischemic stroke and large vessel occlusion: the ASTER randomized clinical trial. JAMA. 2017; 318:443–452.
Article42. Kang DH, Park J. Endovascular stroke therapy focused on stent retriever thrombectomy and direct clot aspiration: historical review and modern application. J Korean Neurosurg Soc. 2017; 60:335–347.43. Gory B, Mazighi M, Blanc R, Labreuche J, Piotin M, Turjman F, et al. Mechanical thrombectomy in basilar artery occlusion: influence of reperfusion on clinical outcome and impact of the first-line strategy (ADAPT vs stent retriever). J Neurosurg. 2018; 129:1482–1491.
Article44. Stapleton CJ, Leslie-Mazwi TM, Torok CM, Hakimelahi R, Hirsch JA, Yoo AJ, et al. A direct aspiration first-pass technique vs stentriever thrombectomy in emergent large vessel intracranial occlusions. J Neurosurg. 2018; 128:567–574.
Article45. Al Kasab S, Almadidy Z, Spiotta AM, Turk AS, Chaudry MI, Hungerford JP, et al. Endovascular treatment for AIS with underlying ICAD. J Neurointerv Surg. 2017; 9:948–951.
Article46. Lee YY, Yoon W, Kim SK, Baek BH, Kim GS, Kim JT, et al. Acute basilar artery occlusion: differences in characteristics and outcomes after endovascular therapy between patients with and without underlying severe atherosclerotic stenosis. AJNR Am J Neuroradiol. 2017; 38:1600–1604.
Article47. Baik SK, Oh SJ, Park KP, Lee JH. Intra-arterial tirofiban infusion for partial recanalization with stagnant flow in hyperacute cerebral ischemic stroke. Interv Neuroradiol. 2011; 17:442–451.
Article48. Fiorella D, Derdeyn CP, Lynn MJ, Barnwell SL, Hoh BL, Levy EI, et al. SAMMPRIS Trial Investigators. Detailed analysis of periprocedural strokes in patients undergoing intracranial stenting in Stenting and Aggressive Medical Management for Preventing Recurrent Stroke in Intracranial Stenosis (SAMMPRIS). Stroke. 2012; 43:2682–2688.
Article49. Kang DH, Yoon W, Kim SK, Baek BH, Lee YY, Kim YW, et al. Endovascular treatment for emergent large vessel occlusion due to severe intracranial atherosclerotic stenosis. J Neurosurg. 2018; 06. 01. DOI: 10.3171/2018.1.JNS172350. [Epub ahead of print].
Article50. Baek JH, Kim BM, Kim DJ, Heo JH, Nam HS, Yoo J. Stenting as a rescue treatment after failure of mechanical thrombectomy for anterior circulation large artery occlusion. Stroke. 2016; 47:2360–2363.
Article51. Chang Y, Kim BM, Bang OY, Baek JH, Heo JH, Nam HS, et al. Rescue stenting for failed mechanical thrombectomy in acute ischemic stroke: a multicenter experience. Stroke. 2018; 49:958–964.52. Leung TW, Wang L, Soo YOY, Ip VHL, Chan AYY, Au LWC, et al. Evolution of intracranial atherosclerotic disease under modern medical therapy. Ann Neurol. 2015; 77:478–486.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Angioplasty, Stenting and Other Potential Treatments of Atherosclerotic Stenosis of the Intracranial Arteries: Past, Present and Future
- Endovascular Treatment of Large Vessel Occlusion Strokes Due to Intracranial Atherosclerotic Disease
- Proximal basilar artery hemorrhage after submaximal angioplasty for intracranial atherosclerotic disease presenting as a large vessel occlusion treated with pipeline embolization device
- Endovascular Therapy for Acute Basilar Artery Occlusion: Comparison between Patients with and without Underlying Intracranial Atherosclerotic Stenosis
- Guideline for Intracranial Stenting of Symptomatic Intracranial Artery Stenosis: Preliminary Report