Kosin Med J.
2018 Dec;33(3):454-462. 10.7180/kmj.2018.33.3.454.
A Case Of Cavernous Sinus Syndrome and Mutifocal Cerebral Infarction Related To Mucormycosis Of Sphenoid Sinus
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and neck surgery, College of Medicine, Kosin University, Busan, Korea. entkwon@hanmail.net
- KMID: 2442559
- DOI: http://doi.org/10.7180/kmj.2018.33.3.454
Abstract
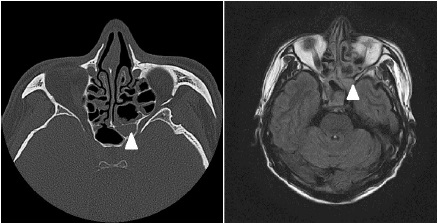
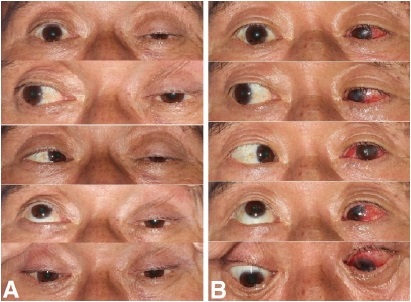
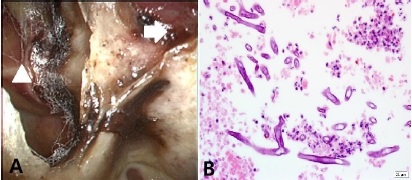
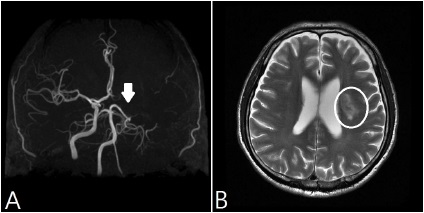
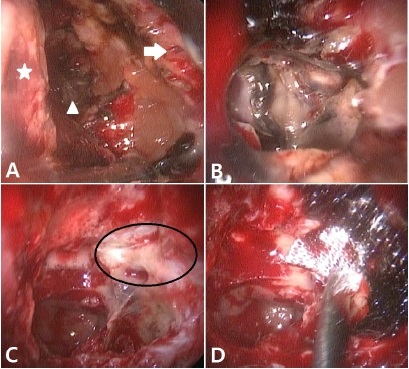
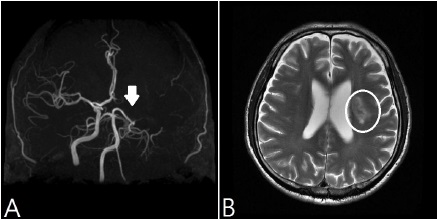
- A 54-year-old man, suffering from severe headache and ophthalmoplegia after undergoing endoscopic sinus surgery was referred to a tertiary hospital. Computed tomography (CT) revealed soft tissue density lesions in the left sphenoid sinus. The internal carotid artery was shown to be occluded in brain magnetic resonance imaging (MRI) scans without any other cerebral lesion. Endoscopic view of left nasal cavity shows whitish hyphae in the ethmoid and the sphenoid sinuses. We diagnosed him with cavernous sinus syndrome caused by mucormycosis and conducted endoscopic sinus surgery to remove remaining lesions and decompress orbit and optic nerves. After the revision surgery the patient's headache and ophthalmoplegia were improved. However, multifocal cerebral infarctions were newly discovered in a postoperative CT scan. We experienced a case of mucormycosis of sphenoid sinus resulting in occlusion of internal carotid artery and multifocal cerebral infarction, and report it with a brief review of these disease entities.
Keyword
MeSH Terms
Figure
Reference
-
1. Thajeb P, Thajeb T, Dai D. Fatal strokes in patients with rhino-orbito-cerebral mucormycosis and associated vasculopathy. Scand J Infect Dis. 2004; 36:643.
Article2. Blitzer A, Lawson W, Meyers BR, Biller HF. Patient survivalfactors in paranasal sinus mucormycosis. Laryngoscope. 1980; 90:635–638.3. Patterson TF, Kirkpatrick WR, White M, Hiemenz JW, Wingard JR, Dupont B, et al. Invasive aspergillosis. Diseases pectrum, treatment practices, and outcomes. I3 Aspergillus Study Group. Medicine. 2000; 79:250.
Article4. Vessely MB, Zitsch RP 3rd, Estrem SA, Renner G. Atypical presentations of mucormycosis in the head and neck. Otolaryngol Head Neck Surg. 1996; 115:573–577.
Article5. Bendet E, Talmi YP, Kronenberg J. Rhinoorbito-cerebral mycormycosis. Otolaryngol Head Neck Surg. 1996; 114:830–832.6. Keane JR. Cavernous sinus syndrome.Analysis of 151 cases. Arch Neurol. 1996; 53:967–971.7. Onerci M, Gursel B, Hosal S, Gulekon N, Gokoz A. Rhinocerebral mucormycosis with extension to the cavernous sinus. Rhinology. 1991; 29:321–324.8. Jin YW, Cho JS, Kim KH, Cha CI. Rhinocerebralmucormycosis with selective cranial nerve palsy. Korean J Otolaryngol-Head Neck Surg. 2001; 44:674–677.9. Bendet E, Talmi YP, Kronenberg J. Rhino-orbitocerebral mycormycosis. Otolaryngol Head Neck Surg. 1996; 114:830–832.10. Talmi YP, Goldschmied-Reouven A, Bakon M, Barshack I, Wolf M, Horowitz Z, et al. Rhino-orbital and rhino-orbito-cerebral mucormycosis. Otolaryngol Head Neck Surg. 2002; 127:22.
Article11. Baumann A, Zimmerli S, Hausler R, Caversaccio M. Invasive sphe¬noidalaspergillosis: successful treatment with sphenoidotomy and voriconazole. ORL J Otorhinolaryngol Relat Spec. 2007; 69:121–126.
Article12. Sugar AM. Mucormycosis. Clin Infect Dis. 1992; 14:s126–s129.
Article13. Viterbo S, Fasolis M, Garzino-Demo P, Griffa A, Boffano P, Iaquinta C, et al. Management and outcomes of three cases of rhinocerebralmucormycosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011; 112:e69–e74.14. Mohamed MS, Abdel-Motaleb HY, Mobarak FA. Management of rhino-orbital mucormycosis. Saudi Med J. 2015; 36:865–868.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Cavernous Sinus Thrombophlebitis Secondary toAcute Isolated Sphenoid Sinusitis
- A Case of Bilateral Cavernous Sinus Mucormycosis
- Cavernous Sinus Syndrome Complicating Occlusion of the Internal Carotid Artery by Necrotizing Sinusitis
- Lateral Sinus Thrombophlebitis Caused by Isolated Sphenoid Sinusitis
- Cerebral Infarction due to Mucormycosis in the Cavernous Sinus