J Korean Soc Radiol.
2019 Mar;80(2):213-225. 10.3348/jksr.2019.80.2.213.
A Review of Three-Dimensional Printing Technology for Medical Applications
- Affiliations
-
- 1Department of Convergence Medicine, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea. namkugkim@gmail.com
- 2Department of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- 3Department of Urology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- 4Department of Health Screening and Promotion Center, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- 5Division of Breast Surgery, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- 6Department of Thoracic and Cardiovascular Surgery, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- 7Department of Ophthalmology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- KMID: 2442514
- DOI: http://doi.org/10.3348/jksr.2019.80.2.213
Abstract
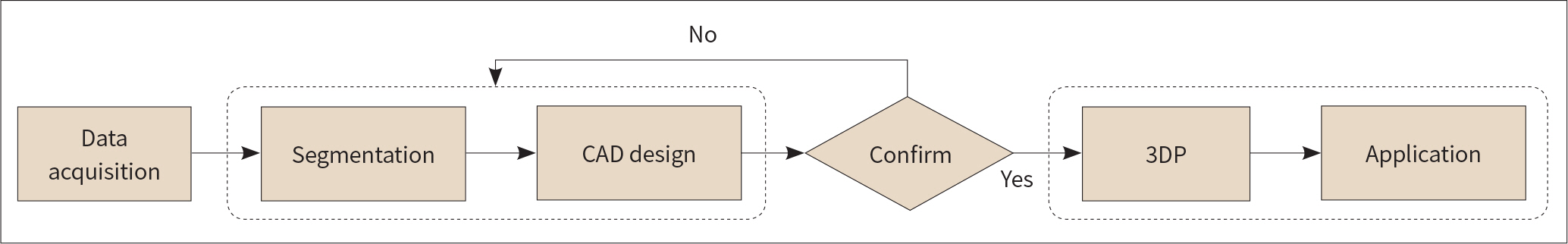
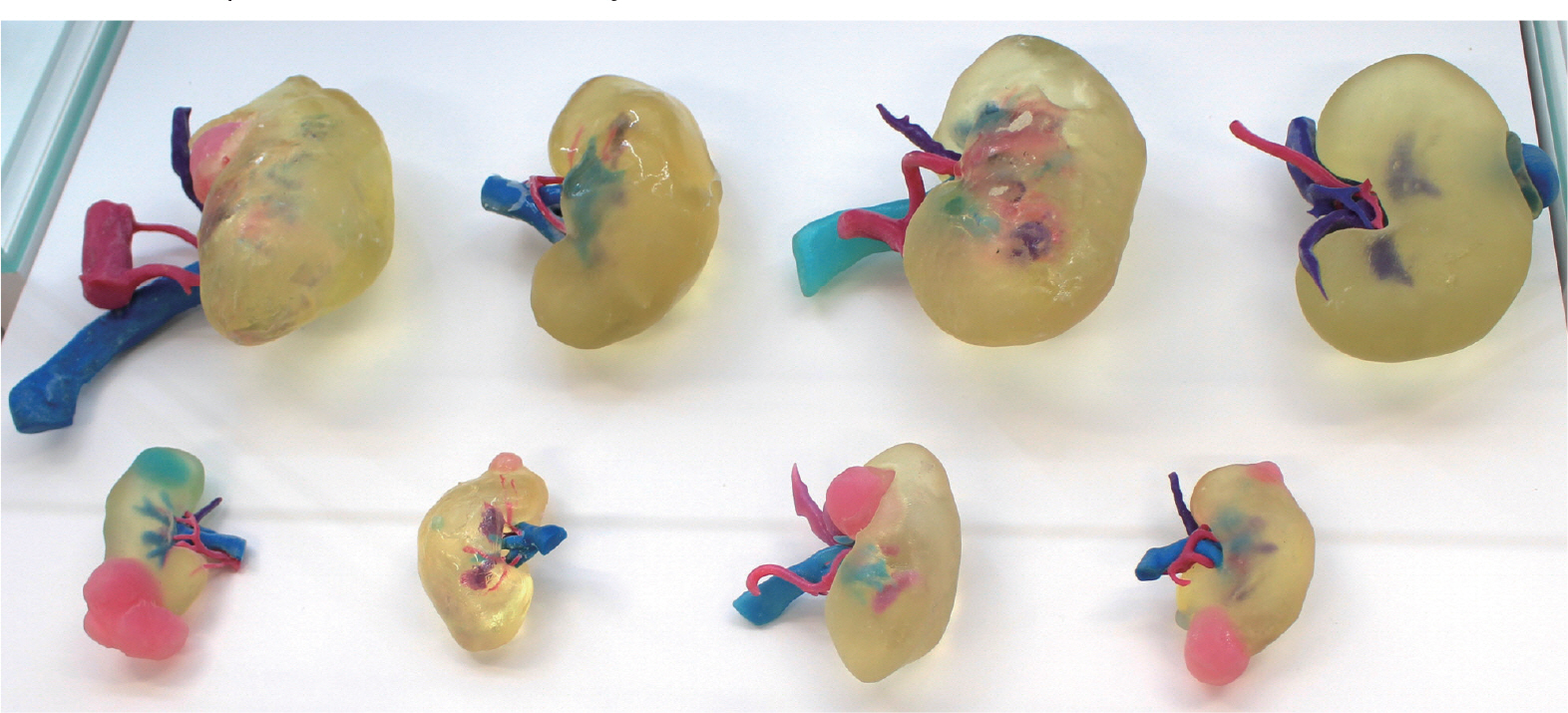
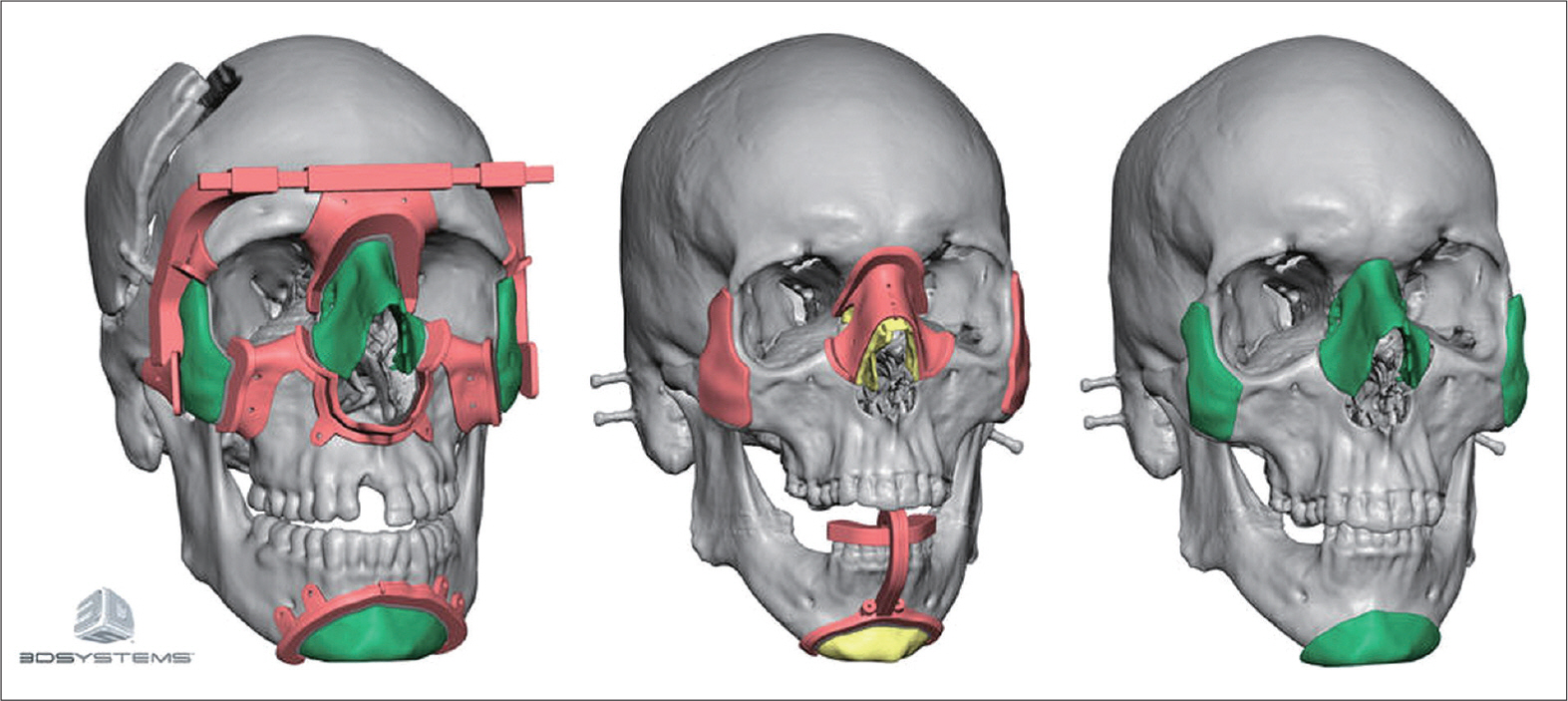
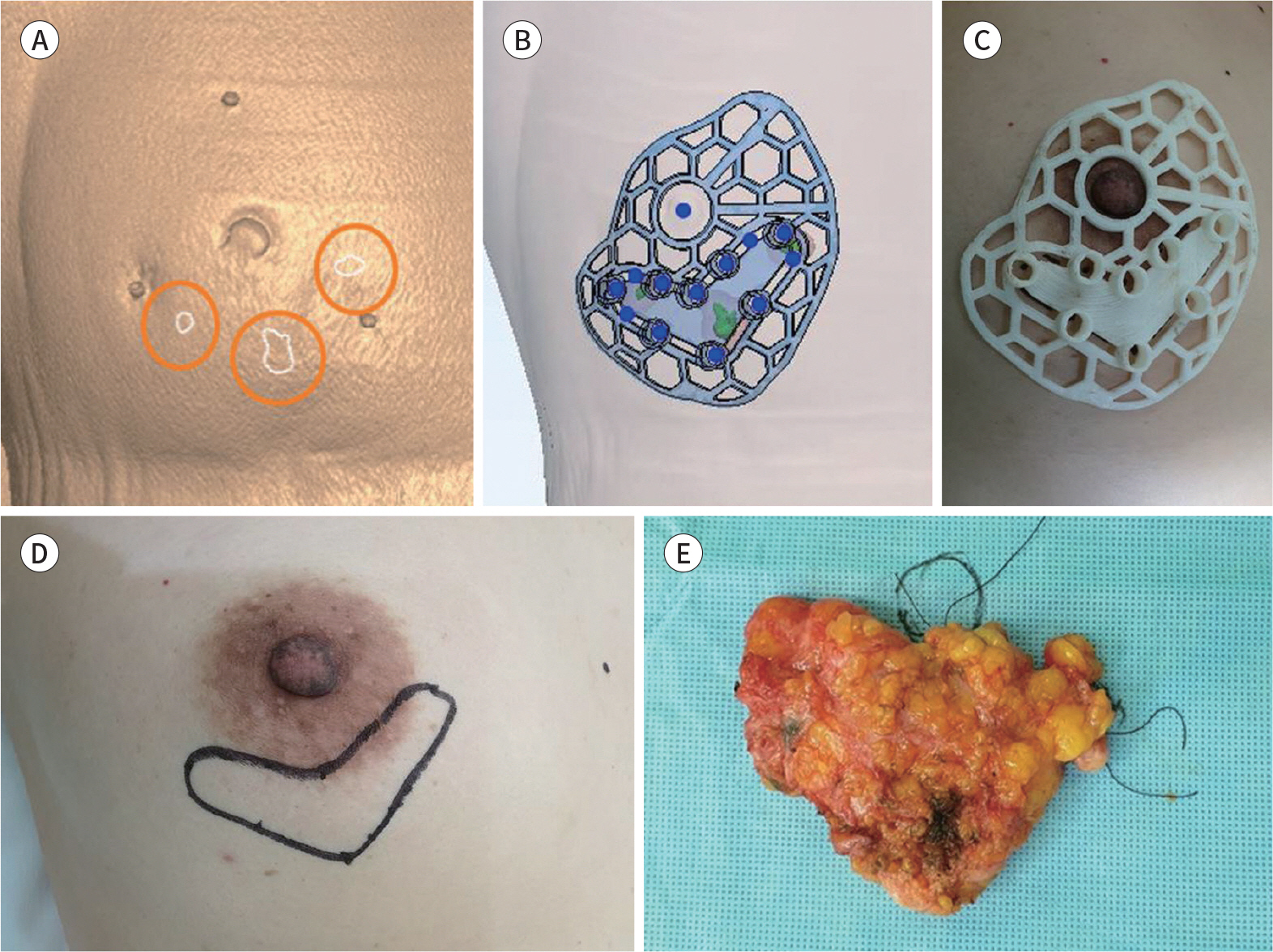
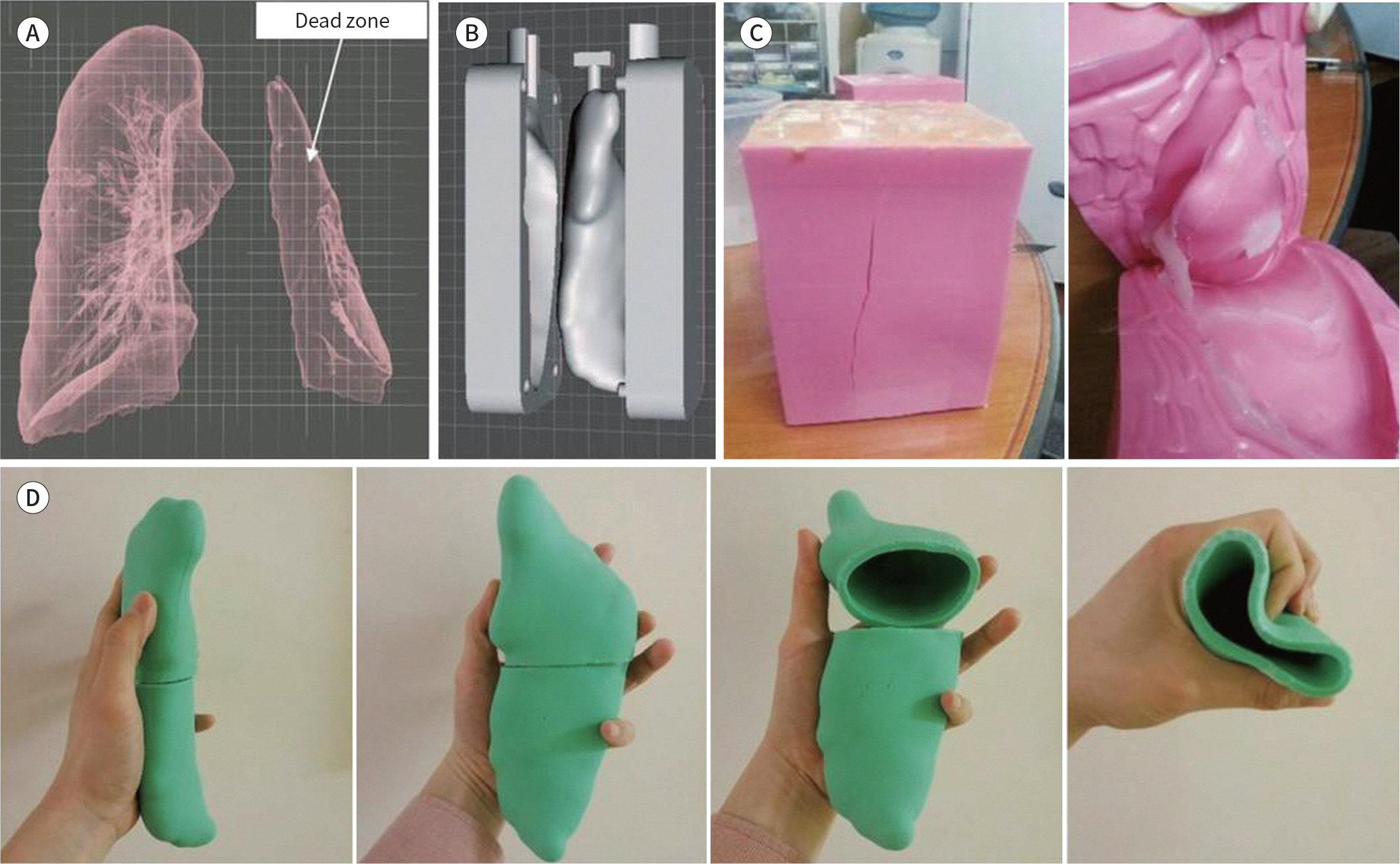
- Three-dimensional (3D) printing technology, with additive manufacturing, can aid in the production of various kinds of patient-specific medical devices and implants in medical fields, which cannot be covered by mass production systems for producing conventional devices/implants. The simulator-based medical image demonstrates the anatomical structure of the disease, which can be used for education, diagnosis, preparation of treatment plan and preoperative surgical guide, etc. The surgical guide is used as a patient-specific medical device for guiding incision, resection, insertion, and marking. As 3D printers can output materials that can be inserted into the human body, the patient-specific implant device that reflects the patient's anatomy and surgical plan could be of relevance. In addition, patient-specific aids, including gibs, splints, prostheses, and epitheses, could be used for a better outcome. Finally, bio-printing is also used to cultivate cells to produce functional artificial tissues.
MeSH Terms
Figure
Cited by 1 articles
-
Advanced Sectioned Images of a Cadaver Head with Voxel Size of 0.04 mm
Beom Sun Chung, Miran Han, Donghwan Har, Jin Seo Park
J Korean Med Sci. 2019;34(34):. doi: 10.3346/jkms.2019.34.e218.
Reference
-
References
1. Huang SH, Liu P, Mokasdar A, Hou L. Additive manufacturing and its societal impact: a literature review.Int J Adv Manuf Technol. 2013; 67:1191–1203.2. Gross BC, Erkal JL, Lockwood SY, Chen C, Spence DM. Evaluation of 3D printing and its potential impact on biotechnology and the chemical sciences. Anal Chem. 2014; 86:3240–3253.
Article3. Rengier F, Mehndiratta A, Von Tengg-Kobligk H, Zechmann CM, Unterhinninghofen R, Kauczor HU, et al. 3D printing based on imaging data: review of medical applications.Int J Comput Assist Radiol Surg. 2010; 5:335–341.4. Mitsouras D, Liacouras P, Imanzadeh A, Giannopoulos AA, Cai TR, Kumamaru KK, et al. Medical 3D printing for the radiologist.Radiographics. 2015; 35:1965–1988.5. McGurk M, Amis AA, Potamianos P, Goodger NM. Rapid prototyping techniques for anatomial modelling in medicine.Ann R Coll Surg Engl. 1997; 79:169–174.6. Kim GB, Lee S, Kim H, Yang DH, Kim YH, Kyung YS, et al. Three-dimensional printing: basic principles and applications in medicine and radiology.Korean J Radiol. 2016; 17:182–197.7. Ventola CL. Medical applications for 3D printing: current and projected uses. P T. 2014; 39:704–711.8. Michalski MH, Ross JS. The shape of things to come: 3D printing in medicine.JAMA. 2014; 312:2213–2214.9. Dodziuk H. Applications of 3D printing in healthcare. Kard/iiochir Torakoch/iirurgia Pol. 2016; 13:283–293.
Article10. Wong KV, Hernandez A. A review of additive manufacturing. ISRN Mech Eng. 2012; 2012:1–10.
Article11. Levy GN, Schindel R, Kruth JP. Rapid manufacturing and rapid tooling with layer manufacturing (LM) technologies, state of the art and future perspectives. CIRP Ann Manuf Technol. 2003; 52:589–609.
Article12. Chepelev L, Giannopoulos A, Tang A, Mitsouras D, Rybicki FJ. Medical 3D printing: methods to standardize terminology and report trends.3D Print Med. 2017; 3:4.13. Gupta BM, Dhawan SM. Three dimensional (3D) printing: a scientometric assessment of global publications output during 2007–16.DESIDOC Journal of Library & Information Technology. 2018; 38:238–245.14. Ayoub AF, Rehab M, O'Neil M, Khambay B, Ju X, Barbenel J, et al. A novel approach for planning orthognathic surgery: the integration of dental casts into three-dimensional printed mandibular models.Int J Oral Maxillofac Surg. 2014; 43:454–459.15. Li B, Zhang L, Sun H, Yuan J, Shen SG, Wang X. A novel method of computer aided orthognathic surgery using individual CAD/CAM templates: a combination of osteotomy and repositioning guides.Br J Oral Maxillo-fac Surg. 2013; 51:E239–E244.16. Canstein C, Cachot P, Faust A, Stalder AF, Bock J, Frydrychowicz A, et al. 3D MR flow analysis in realistic rapid-prototyping model systems of the thoracic aorta: comparison with in vivo data and computational fluid dynamics in identical vessel geometries. Magn Reson Med. 2008; 59:535–546.
Article17. Anderson JR, Thompson WL, Alkattan AK, Diaz O, Klucznik R, Zhang YJ, et al. Three-dimensional printing of anatomically accurate, patient specific intracranial aneurysm models.J Neurointerv Surg. 2016; 8:517–520.18. Jacobo OM, Giachero VE, Hartwig DK, Mantrana GA. Three-dimensional printing modeling: application in maxillofacial and hand fractures and resident training. Eur J Plast Surg. 2018; 41:137–146.
Article19. Giannopoulos AA, Mitsouras D, Yoo SJ, Liu PP, Chatzizisis YS, Rybicki FJ. Applications of 3D printing in cardiovascular diseases. Nat Rev Cardiol. 2016; 13:701–718.
Article20. Wood BC, Sher SR, Mitchell BJ, Oh AK, Rogers GF, Boyajian MJ. Conjoined twin separation: integration of three-dimensional modeling for optimization of surgical planning.J Craniofac Surg. 2017; 28:4–10.21. Jabero M, Sarment DP. Advanced surgical guidance technology: a review. Implant Dent. 2006; 15:135–142.
Article22. Barth RJ Jr, Krishnaswamy V, Paulsen KD, Rooney TB, Wells WA, Rizzo E, et al. A patient-specific 3D-printed form accurately transfers supine MRI-derived tumor localization information to guide breast-conserving surgery.Ann Surg Oncol. 2017; 24:2950–2956.23. Ciocca L, De Crescenzio F, Fantini M, Scotti R. CAD/CAM and rapid prototyped scaffold construction for bone regenerative medicine and surgical transfer of virtual planning: a pilot study. Comput Med Imaging Graph. 2009; 33:58–62.24. Suojanen J, Leikola J, Stoor P. The use of patient-specific implants in orthognathic surgery: a series of 32 maxillary osteotomy patients. J Craniomaxillofac Surg. 2016; 44:1913–1916.
Article25. Flügge TV, Nelson K, Schmelzeisen R, Metzger MC. Three-dimensional plotting and printing of an implant drilling guide: simplifying guided implant surgery.J Oral Max/iillofac Surg. 2013; 71:1340–1346.26. Sarment DP, Sukovic P, Clinthorne N. Accuracy of implant placement with a stereolithographic surgical guide.Int J Oral Max/iillofac Implants. 2003; 18:571–577.27. Ersoy AE, Turkyilmaz I, Ozan O, McGlumphy EA. Reliability of implant placement with stereolithographic surgical guides generated from computed tomography: clinical data from 94 implants. J Periodontol. 2008; 79:1339–1345.
Article28. Oka K, Moritomo H, Goto A, Sugamoto K, Yoshikawa H, Murase T. Corrective osteotomy for malunited intraarticular fracture of the distal radius using a custom-made surgical guide based on three-dimensional computer simulation: case report. J Hand Surg Am. 2008; 33:835–840.
Article29. Kang S, Kwon J, Ahn CJ, Esmaeli B, Kim GB, Kim N, et al. Generation of customized orbital implant templates using 3-dimensional printing for orbital wall reconstruction.Eye (Lond). 2018; 32:1864–1870.30. Tabakovic´ SZ, Konstantinovic´ VS, Radosavljevic´ R, Movrin D, Hadz istevic ´ M, Hatab N. Application of computer-aided designing and rapid prototyping technologies in reconstruction of blowout fractures of the orbital floor. J Cran/iiofac Surg. 2015; 26:1558–1563.31. Morrison RJ, Hollister SJ, Niedner MF, Mahani MG, Park AH, Mehta DK, et al. Mitigation of tracheobroncho-malacia with 3D-printed personalized medical devices in pediatric patients.Sci Transl Med. 2015; 7:285ra64.32. Zopf DA, Hollister SJ, Nelson ME, Ohye RG, Green GE. Bioresorbable airway splint created with a three-dimensional printer.N Engl J Med. 2013; 368:2043–2045.33. Choi JW, Kim N. Clinical application of three-dimensional printing technology in craniofacial plastic surgery. Arch Plast Surg. 2015; 42:267–277.
Article34. Aranda JL, Jiménez MF, Rodríguez M, Varela G. Tridimensional titanium-printed custom-made prosthesis for sternocostal reconstruction. Eur J Cardiothorac Surg. 2015; 48:e92–e94.
Article35. Aragón J, Pérez Méndez I. Dynamic 3D printed titanium copy prosthesis: a novel design for large chest wall resection and reconstruction. J Thorac D/iis. 2016; 8:E385–E389.
Article36. Chen Y, Lin H, Zhang X, Huang W, Shi L, Wang D. Application of 3D-printed and patient-specific cast for the treatment of distal radius fractures: initial experience.3D Print Med. 2017; 3:11.37. Fitzpatrick AP, Mohanned MI, Collins PK, Gibson I. Design of a patient specific, 3D printed arm cast.KnE Eng ineering. 2017; 2:135–142.38. Menneking H, Klein M, Locke HG, Gonschior S. Postoperative management of bone-anchored facial epithe-ses. HNO. 1998; 46:579–582.39. Su S, Moran K, Robar JL. Design and production of 3D printed bolus for electron radiation therapy. J Appl Clin Med Phys. 2014; 15:194–211.
Article40. Solomon J, Samei E. Quantum noise properties of CT images with anatomical textured backgrounds across reconstruction algorithms: FBP and SAFIRE. Med Phys. 2014; 41:091908.
Article41. Murphy SV, Atala A. 3D bioprinting of tissues and organs. Nat Biotechnol. 2014; 32:773–785.
Article42. Das S, Pati F, Choi YJ, Rijal G, Shim JH, Kim SW, et al. Bioprintable, cell-laden silk fibroin-gelatin hydrogel supporting multilineage differentiation of stem cells for fabrication of three-dimensional tissue constructs.Acta Biomater. 2015; 11:233–246.43. Khalyfa A, Vogt S, Weisser J, Grimm G, Rechtenbach A, Meyer W, et al. Development of a new calcium phosphate powder-binder system for the 3D printing of patient specific implants.J Mater Sci Mater Med. 2007; 18:909–916.44. Park SH, Kim TG, Kim HC, Yang DY, Park TG. Development of dual scale scaffolds via direct polymer melt deposition and electrospinning for applications in tissue regeneration.Acta Biomater. 2008; 4:1198–1207.45. Derby B. Printing and prototyping of tissues and scaffolds.Science. 2012; 338:921–926.46. Pati F, Jang J, Ha DH, Kim SW, Rhie JW, Shim JH, et al. Printing three-dimensional tissue analogues with de-cellularized extracellular matrix bioink. Nat Commun. 2014; 5:3935.
Article47. Nguyen DG, Funk J, Robbins JB, Crogan-Grundy C, Presnell SC, Singer T, et al. Bioprinted 3D primary liver tissues allow assessment of organ-level response to clinical drug induced toxicity in vitro.PLos One. 2016; 11:e0158674.48. Chia HN, Wu BM. Recent advances in 3D printing of biomaterials.J Biol Eng. 2015; 9:4.49. Ho CM, Ng SH, Li KH, Yoon YJ. 3D printed microfluidics for biological applications.Lab Chip. 2015; 15:3627–3637.50. Yazdi AA, Popma A, Wong W, Nguyen T, Pan YY, Xu J. 3D printing: an emerging tool for novel microfluidics and lab-on-a-chip applications.Microfluid Nanofluidics. 2016; 20:50.51. Zhang DQ, Chen SC. A novel kernelized fuzzy C-means algorithm with application in medical image segmentation. Artif Intell Med. 2004; 32:37–50.
Article52. 3D Systems. Virtual Surgical Planning Assists with Full Face Transplant. Available at.https://ko.3dsystems.com/blog/2015/11/virtual-surgical-planning-assists-full-face-transplant. Published 2015. Accessed Mar 20,. 2019.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Application of Three-Dimensional Printing in the Fracture Management
- A Review of Current Clinical Applications of Three-Dimensional Printing in Spine Surgery
- Medical Applications of 3D Printing and Standardization Issues
- Clinical Applications of Three-Dimensional Printing in Cardiovascular Disease
- Three-Dimensional Printing Technology in Orthopedic Surgery