Anat Cell Biol.
2019 Mar;52(1):100-101. 10.5115/acb.2019.52.1.100.
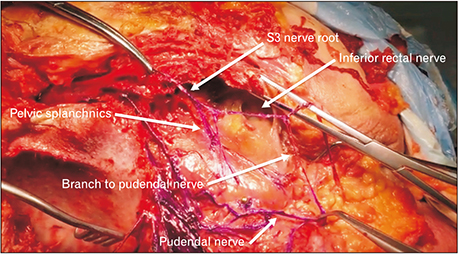
Report of an inferior rectal nerve variant arising from the S3 ventral ramus
- Affiliations
-
- 1Seattle Science Foundation, Seattle, WA, USA. joei@seattlesciencefoundation.org
- 2Swedish Neuroscience Institute, Swedish Medical Center, Seattle, WA, USA.
- 3Department of Anatomical Sciences, St. George's Univerisity, St. George's, Grenada, West Indies.
- KMID: 2442339
- DOI: http://doi.org/10.5115/acb.2019.52.1.100
Abstract
- In surgical approaches to the perineum in general and anal region specifically, considering the possible variations of the inferior rectal nerve is important for the surgeon. Normally, the inferior rectal nerve originates as a branch of the pudendal nerve. However, during routine dissection, a variant of the inferior rectal nerve was found where it arose directly from the third sacral nerve ventral ramus (S3). Many cases have described the inferior rectal nerve arising independently from the sacral plexus, most commonly from the fourth sacral nerve root (S4); however, few cases have reported the inferior rectal nerve arising from S3. Herein, we describe a variant of the inferior rectal nerve in which the nerve arises independently from the sacral plexus.
Figure
Reference
-
1. Schraffordt SE, Tjandra JJ, Eizenberg N, Dwyer PL. Anatomy of the pudendal nerve and its terminal branches: a cadaver study. ANZ J Surg. 2004; 74:23–26.
Article2. Mahakkanukrauh P, Surin P, Vaidhayakarn P. Anatomical study of the pudendal nerve adjacent to the sacrospinous ligament. Clin Anat. 2005; 18:200–205.
Article3. Roberts WH, Taylor WH. Inferior rectal nerve variations as it relates to pudendal block. Anat Rec. 1973; 177:461–463.
Article4. Henry BM, Vikse J, Pekala P, Loukas M, Tubbs RS, Walocha JA, Jones DG, Tomaszewski KA. Consensus guidelines for the uniform reporting of study ethics in anatomical research within the framework of the anatomical quality assurance (AQUA) checklist. Clin Anat. 2018; 31:521–524.
Article5. Tomaszewski KA, Henry BM, Kumar Ramakrishnan P, Roy J, Vikse J, Loukas M, Tubbs RS, Walocha JA. Development of the Anatomical Quality Assurance (AQUA) checklist: Guidelines for reporting original anatomical studies. Clin Anat. 2017; 30:14–20.
Article6. Achtari C, McKenzie BJ, Hiscock R, Rosamilia A, Schierlitz L, Briggs CA, Dwyer PL. Anatomical study of the obturator foramen and dorsal nerve of the clitoris and their relationship to minimally invasive slings. Int Urogynecol J Pelvic Floor Dysfunct. 2006; 17:330–334.
Article7. Shafik A, el-Sherif M, Youssef A, Olfat ES. Surgical anatomy of the pudendal nerve and its clinical implications. Clin Anat. 1995; 8:110–115.
Article8. Leclair F, Robert R, Faure A, Armstrong O, Rogez JM, Lardoux MC, Leborgne J. The inferior rectal nerve: anatomical bases of perineal pain. Morphologie. 2001; 85:21–24.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Variations of the ventral rami of the brachial plexus
- Study On The Relationship Of The Inferior Alveolar Nerve Position Between Buccal And Lingual Side Using Ct And Orthpantomogram
- Uncommon branching pattern with a prominent articular ramus of the inferior gluteal artery in a Korean male cadaver
- Stress Fractures in Pubic Bone: Report of 3 Cases
- Avoidance of Injury to the Inferior Alveolar Nerve in Mandibular Angle Contouring; Maneuver of One Inch