Infect Chemother.
2019 Mar;51(1):1-9. 10.3947/ic.2019.51.1.1.
Clinical Characteristics and Antimicrobial Susceptibility Trends in Citrobacter Bacteremia: An 11-Year Single-Center Experience
- Affiliations
-
- 1Division of Infectious Diseases, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea. sumichoi@catholic.ac.kr
- 2Department of Laboratory Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 3Vaccine Bio Research Institute, Seoul, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 4Emergency care center, Konyang University Hospital, Daejeon, Korea.
- KMID: 2442216
- DOI: http://doi.org/10.3947/ic.2019.51.1.1
Abstract
- BACKGROUND
Recently, Citrobacter freundii bacteremia outbreak in a neonatal intensive care unit has attracted public attention in Korea. However, Citrobacter bacteremia is uncommon and usually occurs in patients with underlying diseases such as malignancy and hepatobiliary diseases. Increase in resistance and emerging of multidrug resistance among Citrobacter species have gradually been reported. The aim of this study was to investigate the clinical characteristics and outcome of C. freundii and non-freundii bacteremia and antimicrobial susceptibility trends.
MATERIALS AND METHODS
We reviewed the medical records of patients with Citrobacter bacteremia at St. Mary's Hospital, from 2007 to 2017.
RESULTS
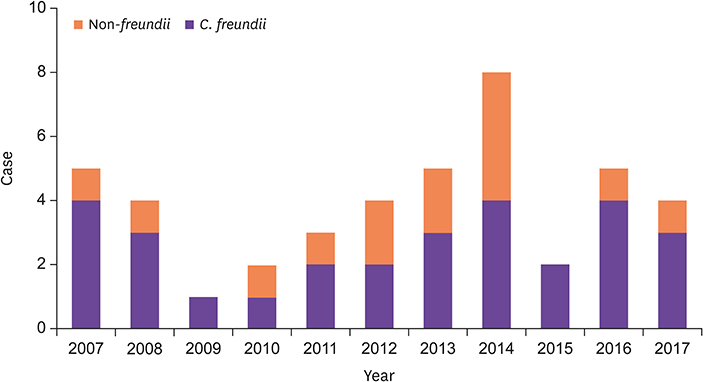
A total of 43 patients with a median age of 72 (24-93) years was identified and 90.7% of them had comorbidities. Twenty-nine (67.4%) patients had C. freundii bacteremia while 14 had non-freundii bacteremia (six of C. braakii, five of C. koseri, two of C. amalonaticus and one of C. youngae). A total of 26 (51.2%) patients had community-acquired infection and intra-abdominal infection including hepatobiliary tract was the most common portal of entry (24/43, 55.8%). Moreover, hepatobiliary tract was the leading primary site of nosocomial infection (9/17, 52.9%). Polymicrobial bacteremia was observed in 21 (48.8%) patients. The percentages of Citrobacter species susceptible to ampicillin, amikacin, aztreonam, cefazolin, cefoxitin, cefotaxime, cefepime, piperacillin-tazobactam, ciprofloxacin, and imipenem were 9.5%, 97.6%, 73.8%, 9.5%, 14.3%, 71.4%, 92.9%, 83.3%, 83.3% and 100%, respectively. The resistance rate did not increase during the study period. Of 39 patients treated with antibiotics, 36 (92.3%) received appropriate empirical antibiotics. Overall mortality was 18.6%. High Charlson comorbidity index and Pitt bacteremia score were significant risk factors for death in univariate analysis and showed trends in the multivariate analysis. No significant difference in clinical features and antimicrobial susceptibility rate was observed between C. freundii and non-freundii bacteremia.
CONCLUSION
Citrobacter bacteremia was predominant in the elderly with comorbidities, while no pediatric case was observed. Hepatobiliary tract is the leading primary focus of bacteremia both in community-acquired and nosocomial infection. The rate of susceptibility to antibiotics has not changed in the last 11 years.
Keyword
MeSH Terms
-
Aged
Amikacin
Ampicillin
Anti-Bacterial Agents
Aztreonam
Bacteremia*
Cefazolin
Cefotaxime
Cefoxitin
Ciprofloxacin
Citrobacter freundii
Citrobacter*
Community-Acquired Infections
Comorbidity
Cross Infection
Drug Resistance
Drug Resistance, Multiple
Humans
Imipenem
Infant, Newborn
Intensive Care, Neonatal
Intraabdominal Infections
Korea
Medical Records
Mortality
Multivariate Analysis
Prognosis
Risk Factors
Amikacin
Ampicillin
Anti-Bacterial Agents
Aztreonam
Cefazolin
Cefotaxime
Cefoxitin
Ciprofloxacin
Imipenem
Figure
Reference
-
1. Lavigne JP, Defez C, Bouziges N, Mahamat A, Sotto A. Clinical and molecular epidemiology of multidrug-resistant Citrobacter spp. infections in a French university hospital. Eur J Clin Microbiol Infect Dis. 2007; 26:439–441.
Article2. Lipsky BA, Hook EW 3rd, Smith AA, Plorde JJ. Citrobacter infections in humans: experience at the Seattle Veterans Administration Medical Center and a review of the literature. Rev Infect Dis. 1980; 2:746–760.
Article3. Jones RN, Jenkins SG, Hoban DJ, Pfaller MA, Ramphal R. In vitro efficacy of six cephalosporins tested against Enterobacteriaceae isolated at 38 North American medical centres participating in the SENTRY Antimicrobial Surveillance Program, 1997-1998. Int J Antimicrob Agents. 2000; 15:111–118.
Article4. Samonis G, Karageorgopoulos DE, Kofteridis DP, Matthaiou DK, Sidiropoulou V, Maraki S, Falagas ME. Citrobacter infections in a general hospital: characteristics and outcomes. Eur J Clin Microbiol Infect Dis. 2009; 28:61–68.
Article5. Kim BN, Woo JH, Ryu J, Kim YS. Resistance to extended-spectrum cephalosporins and mortality in patients with Citrobacter freundii bacteremia. Infection. 2003; 31:202–207.
Article6. Shih CC, Chen YC, Chang SC, Luh KT, Hsieh WC. Bacteremia due to Citrobacter species: significance of primary intraabdominal infection. Clin Infect Dis. 1996; 23:543–549.
Article7. Drelichman V, Band JD. Bacteremias due to Citrobacter diversus and Citrobacter freundii. Incidence, risk factors, and clinical outcome. Arch Intern Med. 1985; 145:1808–1810.
Article8. Doran TI. The role of Citrobacter in clinical disease of children: review. Clin Infect Dis. 1999; 28:384–394.
Article9. Hawkley T, Chang D, Pollard W, Ferraro D. Ecthyma gangrenosum caused by Citrobacter freundii. BMJ Case Rep. 2017; 2017:pii: bcr-2017-220996.10. Lai CC, Tan CK, Lin SH, Liu WL, Liao CH, Huang YT, Hsueh PR. Bacteraemia caused by non-freundii, non-koseri Citrobacter species in Taiwan. J Hosp Infect. 2010; 76:332–335.
Article11. Pepperell C, Kus JV, Gardam MA, Humar A, Burrows LL. Low-virulence Citrobacter species encode resistance to multiple antimicrobials. Antimicrob Agents Chemother. 2002; 46:3555–3560.
Article12. Korea Centers for Disease Control and Prevention (KCDC). Update on epidemiological investigation of infant deaths at Ewha Womans University Mokdong Hospital NICU. Accessed 7 July 2018. Available at: http://www.cdc.go.kr/CDC/eng/info/CdcKPress.jsp?menuIds=HOME002-MNU0576MNU0586&fid=8652&q_type=&q_value=&cid=77357&pageNum.13. Clinical and Laboratory Standards Institute (CLSI). Performance standards for antimicrobial susceptibility testing; 27th ed. CLSI document M100. Wayne, PA: CLSI;2017.14. Clinical and Laboratory Standards Institute (CLSI). Performance standards for antimicrobial susceptibility testing; Twenty-fourth informational supplement. CLSI document M100-S24. Wayne, PA: CLSI;2014.15. Clinical and Laboratory Standards Institute (CLSI). Performance standards for antimicrobial susceptibility testing; twentieth informational supplement. CLSI document M100-S20. Wayne, PA: CLSI;2010.16. Sutter D, Stagliano D, Braun L, Williams F, Arnold J, Ottolini M, Epstein J. Polymicrobial bloodstream infection in pediatric patients: risk factors, microbiology, and antimicrobial management. Pediatr Infect Dis J. 2008; 27:400–405.17. Lenz R, Leal JR, Church DL, Gregson DB, Ross T, Laupland KB. The distinct category of healthcare associated bloodstream infections. BMC Infect Dis. 2012; 12:85.
Article18. Mohanty S, Singhal R, Sood S, Dhawan B, Kapil A, Das BK. Citrobacter infections in a tertiary care hospital in Northern India. J Infect. 2007; 54:58–64.19. Brenner DJ, O'Hara CM, Grimont PA, Janda JM, Falsen E, Aldova E, Ageron E, Schindler J, Abbott SL, Steigerwalt AG. Biochemical identification of Citrobacter species defined by DNA hybridization and description of Citrobacter gillenii sp. nov. (formerly Citrobacter genomospecies 10) and Citrobacter murliniae sp. nov. (formerly Citrobacter genomospecies 11). J Clin Microbiol. 1999; 37:2619–2624.
Article20. Samonis G, Anaissie E, Elting L, Bodey GP. Review of Citrobacter bacteremia in cancer patients over a sixteen-year period. Eur J Clin Microbiol Infect Dis. 1991; 10:479–485.
Article21. Liu LH, Wang NY, Wu AY, Lin CC, Lee CM, Liu CP. Citrobacter freundii bacteremia: Risk factors of mortality and prevalence of resistance genes. J Microbiol Immunol Infect. 2018; 51:565–572.
Article22. Lew PD, Baker AS, Kunz LJ, Moellering RC Jr. Intra-abdominal Citrobacter infections: association with biliary or upper gastrointestinal source. Surgery. 1984; 95:398–403.23. Jones SR, Ragsdale AR, Kutscher E, Sanford JP. Clinical and bacteriologic observations on a recently recognized species of enterobacteriaceae, Citrobacter diversus. J Infect Dis. 1973; 128:563–565.
Article24. McKenzie FE. Case mortality in polymicrobial bloodstream infections. J Clin Epidemiol. 2006; 59:760–761.
Article25. Liu LH, Wang NY, Wu AY, Lin CC, Lee CM, Liu CP. Citrobacter freundii bacteremia: Risk factors of mortality and prevalence of resistance genes. J Microbiol Immunol Infect. 2018; 51:565–572.
Article26. Kanamori H, Yano H, Hirakata Y, Endo S, Arai K, Ogawa M, Shimojima M, Aoyagi T, Hatta M, Yamada M, Nishimaki K, Kitagawa M, Kunishima H, Kaku M. High prevalence of extended-spectrum β-lactamases and qnr determinants in Citrobacter species from Japan: dissemination of CTX-M-2. J Antimicrob Chemother. 2011; 66:2255–2262.
Article27. Zhang R, Yang L, Cai JC, Zhou HW, Chen GX. High-level carbapenem resistance in a Citrobacter freundii clinical isolate is due to a combination of KPC-2 production and decreased porin expression. J Med Microbiol. 2008; 57:332–337.
Article28. Orrett FA, Shurland SM. Prevalence of bacterial pathogens and susceptibility patterns from clinical sources in Trinidad. West Indian Med J. 2000; 49:205–209.29. Wang JT, Chang SC, Chen YC, Luh KT. Comparison of antimicrobial susceptibility of Citrobacter freundii isolates in two different time periods. J Microbiol Immunol Infect. 2000; 33:258–262.30. Venditti C, Fortini D, Villa L, Vulcano A, D'Arezzo S, Capone A, Petrosillo N, Nisii C, Carattoli A, Di Caro A. Circulation of blaKPC-3-Carrying IncX3 Plasmids among Citrobacter freundii Isolates in an Italian Hospital. Antimicrob Agents Chemother. 2017; 61:pii:e0050-17.
Article31. Park JW, Lee E, Lee SJ. HM L. Status of carbapenemase producing Enterobacteriaceae incidence in Korea, 2015-2016. Public Health Wkly Rep. 2017; 10:1243–1247.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antimicrobial drug susceptibility of enterobacter and citrobacter islated from clinical specimens
- Trends in Five-year Blood Cultures of Patients at a University Hospital (2003~2007)
- The Trends of the Species and Antimicrobial Susceptibility of Bacteria and Fungi Isolated from Blood Cultures (1986-1996)
- Antimicrobial Susceptibility Trends and Risk Factors for Antimicrobial Resistance in Pseudomonas aeruginosa Bacteremia: 12-Year Experience in a Tertiary Hospital in Korea
- Analysis for Group B Streptococci Isolated from Bacteremic Patients