J Breast Cancer.
2018 Mar;21(1):80-86. 10.4048/jbc.2018.21.1.80.
Benign Intraductal Papilloma without Atypia on Core Needle Biopsy Has a Low Rate of Upgrading to Malignancy after Excision
- Affiliations
-
- 1Department of Pathology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. sypmd@snu.ac.kr
- 2Department of Pathology, Konyang University Hospital, Daejeon, Korea.
- 3Department of Radiology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- 4Department of Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- KMID: 2441871
- DOI: http://doi.org/10.4048/jbc.2018.21.1.80
Abstract
- PURPOSE
The management of benign intraductal papilloma (IDP) without atypia diagnosed on core needle biopsy (CNB) remains controversial. This study was performed to evaluate the rate of upgrading to malignancy or high-risk lesions after excision and to identify factors associated with upgrading using a large series of benign IDP cases without atypia.
METHODS
We included patients who were diagnosed as having benign IDP without atypia on CNB and underwent surgical or vacuum-assisted excision between 2010 and 2015. We analyzed the clinical, radiologic, and histopathologic features of IDPs that were upgraded to malignancy or high-risk lesions after excision.
RESULTS
A total of 511 benign IDPs without atypia diagnosed via CNB were identified, of which 398 cases were treated with excision. After reviewing these cases, four cases of high-risk lesions in adjacent tissue on CNB, two cases which were revealed as papilloma with atypia, and nine cases of malignancy in the same breast were excluded. In the remaining 383 cases, the rate of upgrading to malignancy and high-risk lesions after excision was 0.8% and 4.4%, respectively. The presence of concurrent contralateral breast cancer, the presence of symptoms, and multifocality were factors significantly associated with upgrading to malignancy on subsequent excision. Surgical excision rather than vacuum-assisted excision was significantly associated with upgrading to high-risk lesions or malignancy.
CONCLUSION
The rate of upgrading to malignancy for benign IDP without atypia was very low, suggesting that close clinical and radiologic observation may be sufficient for patients with benign IDP without atypia on CNB under proper settings.
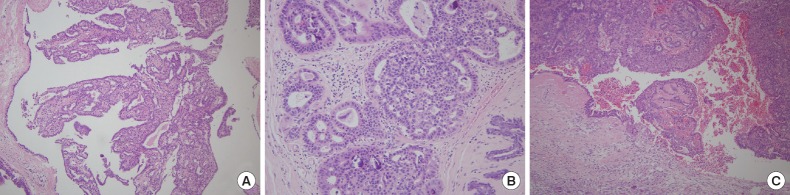
Figure
Reference
-
1. Cyr AE, Novack D, Trinkaus K, Margenthaler JA, Gillanders WE, Eberlein TJ, et al. Are we overtreating papillomas diagnosed on core needle biopsy? Ann Surg Oncol. 2011; 18:946–951. PMID: 21046266.
Article2. Gendler LS, Feldman SM, Balassanian R, Riker MA, Frencher SK, Whelan DB, et al. Association of breast cancer with papillary lesions identified at percutaneous image-guided breast biopsy. Am J Surg. 2004; 188:365–370. PMID: 15474427.
Article3. Renshaw AA, Derhagopian RP, Tizol-Blanco DM, Gould EW. Papillomas and atypical papillomas in breast core needle biopsy specimens: risk of carcinoma in subsequent excision. Am J Clin Pathol. 2004; 122:217–221. PMID: 15323138.4. Rizzo M, Lund MJ, Oprea G, Schniederjan M, Wood WC, Mosunjac M. Surgical follow-up and clinical presentation of 142 breast papillary lesions diagnosed by ultrasound-guided core-needle biopsy. Ann Surg Oncol. 2008; 15:1040–1047. PMID: 18204989.
Article5. McGhan LJ, Pockaj BA, Wasif N, Giurescu ME, McCullough AE, Gray RJ. Atypical ductal hyperplasia on core biopsy: an automatic trigger for excisional biopsy? Ann Surg Oncol. 2012; 19:3264–3269. PMID: 22878619.
Article6. Shiino S, Tsuda H, Yoshida M, Jimbo K, Asaga S, Hojo T, et al. Intraductal papillomas on core biopsy can be upgraded to malignancy on subsequent excisional biopsy regardless of the presence of atypical features. Pathol Int. 2015; 65:293–300. PMID: 25801805.
Article7. Ahmadiyeh N, Stoleru MA, Raza S, Lester SC, Golshan M. Management of intraductal papillomas of the breast: an analysis of 129 cases and their outcome. Ann Surg Oncol. 2009; 16:2264–2269. PMID: 19484312.
Article8. Bennett LE, Ghate SV, Bentley R, Baker JA. Is surgical excision of core biopsy proven benign papillomas of the breast necessary? Acad Radiol. 2010; 17:553–557. PMID: 20223685.
Article9. Ko D, Kang E, Park SY, Kim SM, Jang M, Yun B, et al. The management strategy of benign solitary intraductal papilloma on breast core biopsy. Clin Breast Cancer. 2017; 17:367–372. PMID: 28438672.
Article10. Nakhlis F, Ahmadiyeh N, Lester S, Raza S, Lotfi P, Golshan M. Papilloma on core biopsy: excision vs. observation. Ann Surg Oncol. 2015; 22:1479–1482. PMID: 25361885.
Article11. Pareja F, Corben AD, Brennan SB, Murray MP, Bowser ZL, Jakate K, et al. Breast intraductal papillomas without atypia in radiologic-pathologic concordant core-needle biopsies: rate of upgrade to carcinoma at excision. Cancer. 2016; 122:2819–2827. PMID: 27315013.
Article12. Carder PJ, Garvican J, Haigh I, Liston JC. Needle core biopsy can reliably distinguish between benign and malignant papillary lesions of the breast. Histopathology. 2005; 46:320–327. PMID: 15720418.
Article13. Liberman L, Bracero N, Vuolo MA, Dershaw DD, Morris EA, Abramson AF, et al. Percutaneous large-core biopsy of papillary breast lesions. AJR Am J Roentgenol. 1999; 172:331–337. PMID: 9930777.
Article14. Liberman L, Drotman M, Morris EA, LaTrenta LR, Abramson AF, Zakowski MF, et al. Imaging-histologic discordance at percutaneous breast biopsy. Cancer. 2000; 89:2538–2546. PMID: 11135213.
Article15. Mercado CL, Hamele-Bena D, Singer C, Koenigsberg T, Pile-Spellman E, Higgins H, et al. Papillary lesions of the breast: evaluation with stereotactic directional vacuum-assisted biopsy. Radiology. 2001; 221:650–655. PMID: 11719659.
Article16. Jakate K, De Brot M, Goldberg F, Muradali D, O'Malley FP, Mulligan AM. Papillary lesions of the breast: impact of breast pathology subspecialization on core biopsy and excision diagnoses. Am J Surg Pathol. 2012; 36:544–551. PMID: 22314186.17. Chang JM, Moon WK, Cho N, Han W, Noh DY, Park IA, et al. Risk of carcinoma after subsequent excision of benign papilloma initially diagnosed with an ultrasound (US)-guided 14-gauge core needle biopsy: a prospective observational study. Eur Radiol. 2010; 20:1093–1100. PMID: 19890638.
Article18. Kil WH, Cho EY, Kim JH, Nam SJ, Yang JH. Is surgical excision necessary in benign papillary lesions initially diagnosed at core biopsy? Breast. 2008; 17:258–262. PMID: 18054232.
Article19. Holley SO, Appleton CM, Farria DM, Reichert VC, Warrick J, Allred DC, et al. Pathologic outcomes of nonmalignant papillary breast lesions diagnosed at imaging-guided core needle biopsy. Radiology. 2012; 265:379–384. PMID: 22952379.
Article20. Youk JH, Kim EK, Kwak JY, Son EJ, Park BW, Kim SI. Benign papilloma without atypia diagnosed at US-guided 14-gauge core-needle biopsy: clinical and US features predictive of upgrade to malignancy. Radiology. 2011; 258:81–88. PMID: 20971773.
Article21. Puglisi F, Zuiani C, Bazzocchi M, Valent F, Aprile G, Pertoldi B, et al. Role of mammography, ultrasound and large core biopsy in the diagnostic evaluation of papillary breast lesions. Oncology. 2003; 65:311–315. PMID: 14707450.
Article22. Hong YR, Song BJ, Jung SS, Kang BJ, Kim SH, Chae BJ. Predictive factors for upgrading patients with benign breast papillary lesions using a core needle biopsy. J Breast Cancer. 2016; 19:410–416. PMID: 28053629.
Article23. Schacht DV, Yamaguchi K, Lai J, Kulkarni K, Sennett CA, Abe H. Importance of a personal history of breast cancer as a risk factor for the development of subsequent breast cancer: results from screening breast MRI. AJR Am J Roentgenol. 2014; 202:289–292. PMID: 24450667.
Article24. Harjit K, Willsher PC, Bennett M, Jackson LR, Metcalf C, Saunders CM. Multiple papillomas of the breast: is current management adequate? Breast. 2006; 15:777–781. PMID: 16839765.
Article25. Lewis JT, Hartmann LC, Vierkant RA, Maloney SD, Shane Pankratz V, Allers TM, et al. An analysis of breast cancer risk in women with single, multiple, and atypical papilloma. Am J Surg Pathol. 2006; 30:665–672. PMID: 16723843.
Article26. Rizzo M, Linebarger J, Lowe MC, Pan L, Gabram SG, Vasquez L, et al. Management of papillary breast lesions diagnosed on core-needle biopsy: clinical pathologic and radiologic analysis of 276 cases with surgical follow-up. J Am Coll Surg. 2012; 214:280–287. PMID: 22244207.
Article27. Shin HJ, Kim HH, Kim SM, Yang HR, Sohn JH, Kwon GY, et al. Papillary lesions of the breast diagnosed at percutaneous sonographically guided biopsy: comparison of sonographic features and biopsy methods. AJR Am J Roentgenol. 2008; 190:630–636. PMID: 18287432.
Article28. Mercado CL, Hamele-Bena D, Oken SM, Singer CI, Cangiarella J. Papillary lesions of the breast at percutaneous core-needle biopsy. Radiology. 2006; 238:801–808. PMID: 16424237.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Predictive Factors for Upgrading Patients with Benign Breast Papillary Lesions Using a Core Needle Biopsy
- Clinicopathologic Features of the Papillary Breast Lesions Diagnosed on Ultrasonography-guided Core Needle Biopsy
- Excision Can Be Delayed until Size Grows in Small Papillary Lesions of the Breast
- A Study Regarding Predictive Factors for Malignancy of Papillary Lesions on Core Needle Biopsy of the Breast
- Is US-guided 14-gauge Core Needle Biopsy Valid for Papillary Neoplasm of the Breast?