J Breast Cancer.
2018 Mar;21(1):62-69. 10.4048/jbc.2018.21.1.62.
Clinical Characteristics and Prognosis Associated with Multiple Primary Cancers in Breast Cancer Patients
- Affiliations
-
- 1Department of Surgery, Daejeon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Daejeon, Korea. sun2729@catholic.ac.kr
- 2Department of Surgery, Incheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea.
- 3Department of Surgery, Kyung Hee University Hospital at Gangdong, Kyung Hee University School of Medicine, Seoul, Korea.
- 4Department of Surgery, Seoul National University College of Medicine, Seoul, Korea.
- 5Department of Surgery, Chonnam National University Medical School, Gwangju, Korea.
- 6Department of Surgery, Ajou University School of Medicine, Suwon, Korea.
- 7Department of Surgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- KMID: 2441869
- DOI: http://doi.org/10.4048/jbc.2018.21.1.62
Abstract
- PURPOSE
Breast cancer is one of the most common malignancies worldwide and the second most common cancer among Korean women. The prognosis of breast cancer is poor in patients with other primary cancers. However, there have been few clinical studies regarding this issue. Therefore, we analyzed the characteristics and prognosis of patients with breast cancer with multiple primary cancers (MPCs).
METHODS
Data from the Korean Breast Cancer Society Registry were analyzed. Data from enrolled patients who underwent surgery for breast cancer were analyzed for differences in prognosis dependent on the presence of MPCs, and which MPC characteristics affected their prognosis.
RESULTS
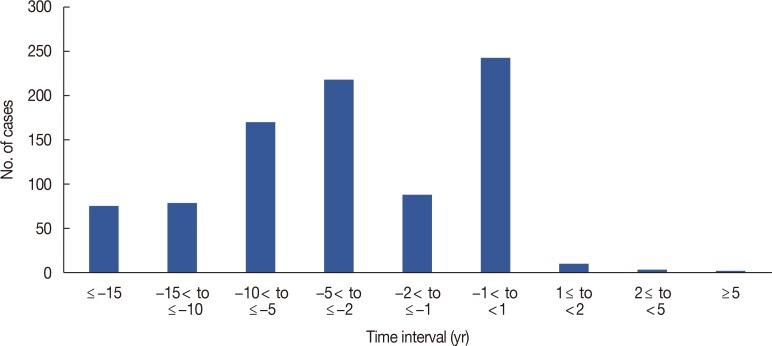
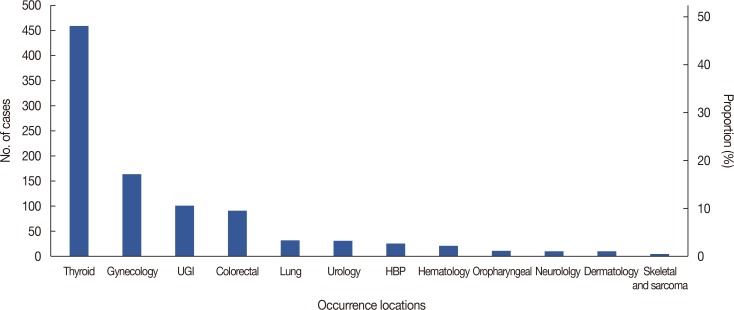
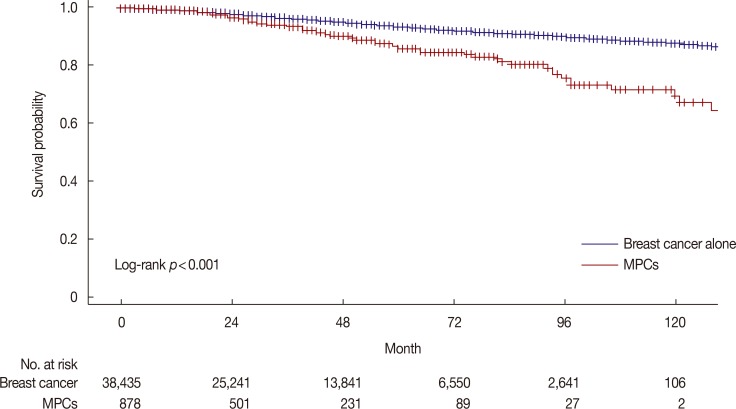
Among the 41,841 patients analyzed, 913 patients were found to have MPCs, accounting for 950 total MPCs. There was a significant difference in survival rates between the breast cancer only group and the MPC group. The 5-year survival rates were 93.6% and 86.7% and the 10-year survival rates were 87.5% and 70.4%, respectively. Among the 913 patients with MPCs, patients with two or more MPCs had significantly worse prognoses than patients with a single MPC. With respect to the time interval between breast cancer and MPC occurrence, patients with a 5-year or greater interval had significantly better prognoses than patients with less than 1 year between occurrences. Among MPCs, thyroid cancer was the most common primary cancer. However, this type was not related to the prognosis of breast cancer. Gynecologic cancer, colorectal cancer, upper gastrointestinal cancer, and lung cancer were related to breast cancer prognosis.
CONCLUSION
MPCs were a poor prognostic factor for patients with breast cancer. Two or more MPCs and a shorter time interval between occurrences were worse prognostic factors. Although MPCs were a poor prognostic factor, thyroid cancer did not affect the prognosis of patients with breast cancer.
MeSH Terms
Figure
Reference
-
1. Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015; 65:87–108. PMID: 25651787.
Article2. Min SY, Kim Z, Hur MH, Yoon CS, Park EH, Jung KW, et al. The basic facts of Korean breast cancer in 2013: results of a nationwide survey and breast cancer registry database. J Breast Cancer. 2016; 19:1–7. PMID: 27066090.
Article3. DeSantis CE, Ma J, Goding Sauer A, Newman LA, Jemal A. Breast cancer statistics, 2017, racial disparity in mortality by state. CA Cancer J Clin. 2017; 67:439–448. PMID: 28972651.
Article4. Berry DA, Cronin KA, Plevritis SK, Fryback DG, Clarke L, Zelen M, et al. Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med. 2005; 353:1784–1792. PMID: 16251534.
Article5. Munoz D, Near AM, van Ravesteyn NT, Lee SJ, Schechter CB, Alagoz O, et al. Effects of screening and systemic adjuvant therapy on ER-specific US breast cancer mortality. J Natl Cancer Inst. 2014; 106:dju289. PMID: 25255803.
Article6. Mariotto AB, Rowland JH, Ries LA, Scoppa S, Feuer EJ. Multiple cancer prevalence: a growing challenge in long-term survivorship. Cancer Epidemiol Biomarkers Prev. 2007; 16:566–571. PMID: 17372253.
Article7. Kim JY, Song HS. Metachronous double primary cancer after treatment of breast cancer. Cancer Res Treat. 2015; 47:64–71. PMID: 25544582.
Article8. Eliyatkin N, Zengel B, Yagci A, Comut E, Postaci H, Uslu A, et al. Properties of synchronous versus metachronous bilateral breast carcinoma with long time follow up. Asian Pac J Cancer Prev. 2015; 16:4921–4926. PMID: 26163616.
Article9. Shan S, She J, Xue ZQ, Su CX, Ren SX, Wu FY. Clinical characteristics and survival of lung cancer patients associated with multiple primary malignancies. PLoS One. 2017; 12:e0185485. PMID: 28957405.
Article10. Bu-Ali H, Solh M, Kapur A, Mittal V. Receptor characteristics of the second tumor in synchronous versus metachronous breast cancer. Am Surg. 2008; 74:702–705. PMID: 18705570.
Article11. Romaniuk А, Lyndin M, Smiyanov V, Sikora V, Rieznik A, Kuzenko Y, et al. Primary multiple tumor with affection of the thyroid gland, uterus, urinary bladder, mammary gland and other organs. Pathol Res Pract. 2017; 213:574–579. PMID: 28214212.
Article12. Arjunan R, Kumar D, Kumar KV, Premlatha CS. Breast cancer with synchronous renal cell carcinoma: a rare presentation. J Clin Diagn Res. 2016; 10:XD03–XD05.13. Castro M, Vierkoetter K, Prager D, Montgomery S, Sedgwick K. Synchronous onset of breast and pancreatic cancers: results of germline and somatic genetic analysis. Case Rep Oncol. 2016; 9:387–394. PMID: 27721756.
Article14. Park EH, Min SY, Kim Z, Yoon CS, Jung KW, Nam SJ, et al. Basic facts of breast cancer in Korea in 2014: the 10-year overall survival progress. J Breast Cancer. 2017; 20:1–11. PMID: 28382089.
Article15. Choi MY, Lee SK, Lee JE, Park HS, Lim ST, Jung Y, et al. Characterization of Korean male breast cancer using an online nationwide breast-cancer database: matched-pair analysis of patients with female breast cancer. Medicine (Baltimore). 2016; 95:e3299. PMID: 27100414.16. Albright F, Teerlink C, Werner TL, Cannon-Albright LA. Significant evidence for a heritable contribution to cancer predisposition: a review of cancer familiality by site. BMC Cancer. 2012; 12:138. PMID: 22471249.
Article17. Soerjomataram I, Coebergh JW. Epidemiology of multiple primary cancers. Methods Mol Biol. 2009; 471:85–105. PMID: 19109776.
Article18. Koubková L, Hrstka R, Dobes P, Vojtesek B, Vyzula R. Second primary cancers: causes, incidence and the future. Klin Onkol. 2014; 27:11–17. PMID: 24635432.19. Gursel B, Meydan D, Özbek N, Ozdemir O, Odabas E. Multiple primary malignant neoplasms from the black sea region of Turkey. J Int Med Res. 2011; 39:667–674. PMID: 21672373.
Article20. Lee J, Park S, Kim S, Kim J, Ryu J, Park HS, et al. Characteristics and survival of breast cancer patients with multiple synchronous or meta-chronous primary cancers. Yonsei Med J. 2015; 56:1213–1220. PMID: 26256962.
Article21. Tabuchi T, Ito Y, Ioka A, Miyashiro I, Tsukuma H. Incidence of meta-chronous second primary cancers in Osaka, Japan: update of analyses using population-based cancer registry data. Cancer Sci. 2012; 103:1111–1120. PMID: 22364479.
Article22. Yoshimoto M, Kasumi F, Fukami A, Nishi M, Kajitani T, Sakamoto G. The influence of family history of cancer, irradiation and anticancer medication (mitomycin C), on the occurrence of multiple primary neoplasms with breast cancer: statistical analysis by the person-year method. Jpn J Clin Oncol. 1985; 15(Suppl 1):191–199. PMID: 3925198.23. Park KJ, Choi HJ, Suh SP, Ki CS, Kim JW. Germline TP53 mutation and clinical characteristics of Korean patients with Li-Fraumeni syndrome. Ann Lab Med. 2016; 36:463–468. PMID: 27374712.
Article24. Mai PL, Best AF, Peters JA, DeCastro RM, Khincha PP, Loud JT, et al. Risks of first and subsequent cancers among TP53 mutation carriers in the National Cancer Institute Li-Fraumeni syndrome cohort. Cancer. 2016; 122:3673–3681. PMID: 27496084.25. Kikuchi S, Nishimura R, Osako T, Okumura Y, Nishiyama Y, Toyozumi Y, et al. Definition of p53 overexpression and its association with the clinicopathological features in luminal/HER2-negative breast cancer. Anticancer Res. 2013; 33:3891–3897. PMID: 24023325.26. Berrington de, Curtis RE, Kry SF, Gilbert E, Lamart S, Berg CD, et al. Proportion of second cancers attributable to radiotherapy treatment in adults: a cohort study in the US SEER cancer registries. Lancet Oncol. 2011; 12:353–360. PMID: 21454129.27. Nielsen SM, White MG, Hong S, Aschebrook-Kilfoy B, Kaplan EL, Angelos P, et al. The breast-thyroid cancer link: a systematic review and meta-analysis. Cancer Epidemiol Biomarkers Prev. 2016; 25:231–238. PMID: 26908594.
Article28. Silva-Vieira M, Carrilho Vaz S, Esteves S, Ferreira TC, Limbert E, Salgado L, et al. Second primary cancer in patients with differentiated thyroid cancer: does radioiodine play a role? Thyroid. 2017; 27:1068–1076. PMID: 28614983.
Article