Allergy Asthma Immunol Res.
2018 Nov;10(6):628-647. 10.4168/aair.2018.10.6.628.
Obesity-Associated Metabolic Signatures Correlate to Clinical and Inflammatory Profiles of Asthma: A Pilot Study
- Affiliations
-
- 1Pneumology Group, Department of Integrated Traditional Chinese and Western Medicine, State Key Laboratory of Biotherapy, West China Hospital, Sichuan University, and Collaborative Innovation Center for Biotherapy, Chengdu, China.
- 2Pneumology Group, Department of Integrated Traditional Chinese and Western Medicine, West China Hospital, Sichuan University, Chengdu, China.
- 3Department of Integrated Traditional Chinese and Western Medicine, Xinqiao Hospital, Third Military University, Chongqing, China.
- 4Center for Asthma and Respiratory Diseases, Department of Respiratory and Sleep Medicine, John Hunter Hospital, Hunter Medical Research Institute, University of Newcastle, New Lambton, NSW, Australia.
- 5Department of Respiratory and Critical Care Medicine, Clinical Research Center for Respiratory Disease, West China Hospital, Sichuan University, Chengdu, China. wcums-respiration@hotmail.com
- KMID: 2441813
- DOI: http://doi.org/10.4168/aair.2018.10.6.628
Abstract
- PURPOSE
Obesity is associated with metabolic dysregulation, but the underlying metabolic signatures involving clinical and inflammatory profiles of obese asthma are largely unexplored. We aimed at identifying the metabolic signatures of obese asthma.
METHODS
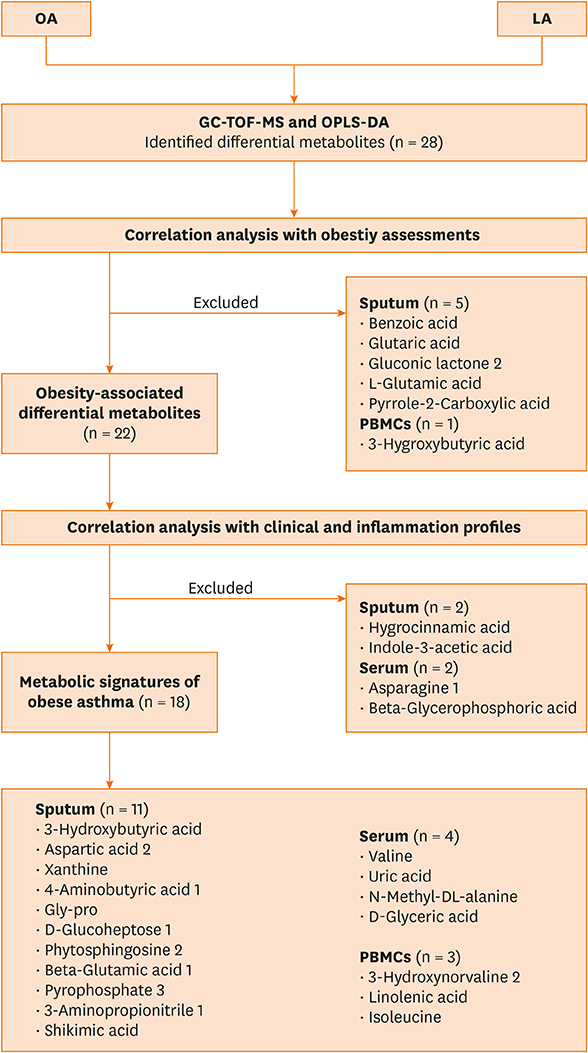
Eligible subjects with obese (n = 11) and lean (n = 22) asthma underwent body composition and clinical assessment, sputum induction, and blood sampling. Sputum supernatant was assessed for interleukin (IL)-1β, -4, -5, -6, -13, and tumor necrosis factor (TNF)-α, and serum was detected for leptin, adiponectin and C-reactive protein. Untargeted gas chromatography time-of-flight mass spectrometry (GC-TOF-MS)-based metabolic profiles in sputum, serum and peripheral blood monocular cells (PBMCs) were analyzed by orthogonal projections to latent structures-discriminate analysis (OPLS-DA) and pathway topology enrichment analysis. The differential metabolites were further validated by correlation analysis with body composition, and clinical and inflammatory profiles.
RESULTS
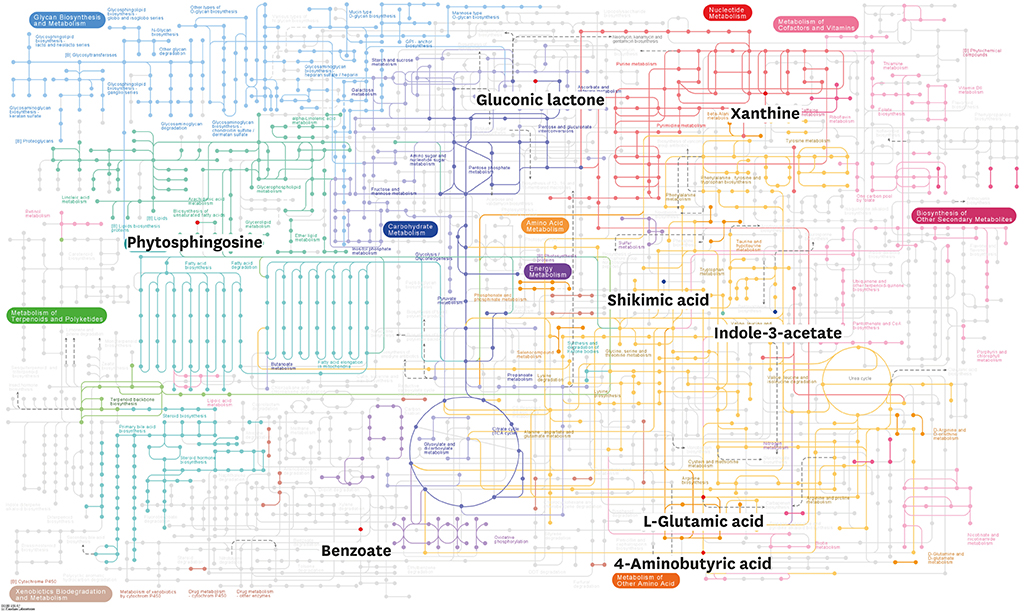
Body composition, asthma control, and the levels of IL-1β, -4, -13, leptin and adiponectin in obese asthmatics were significantly different from those in lean asthmatics. OPLS-DA analysis revealed 28 differential metabolites that distinguished obese from lean asthmatic subjects. The validation analysis identified 18 potential metabolic signatures (11 in sputum, 4 in serum and 2 in PBMCs) of obese asthmatics. Pathway topology enrichment analysis revealed that cyanoamino acid metabolism, caffeine metabolism, alanine, aspartate and glutamate metabolism, phenylalanine, tyrosine and tryptophan biosynthesis, pentose phosphate pathway in sputum, and glyoxylate and dicarboxylate metabolism, glycerolipid metabolism and pentose phosphate pathway in serum are suggested to be significant pathways related to obese asthma.
CONCLUSIONS
GC-TOF-MS-based metabolomics indicates obese asthma is characterized by a metabolic profile different from lean asthma. The potential metabolic signatures indicated novel immune-metabolic mechanisms in obese asthma with providing more phenotypic and therapeutic implications, which needs further replication and validation.
Keyword
MeSH Terms
-
Adiponectin
Alanine
Aspartic Acid
Asthma*
Body Composition
C-Reactive Protein
Caffeine
Chromatography, Gas
Glutamic Acid
Interleukins
Leptin
Mass Spectrometry
Metabolism
Metabolome
Metabolomics
Obesity
Pentose Phosphate Pathway
Phenylalanine
Pilot Projects*
Sputum
Tryptophan
Tumor Necrosis Factor-alpha
Tyrosine
Adiponectin
Alanine
Aspartic Acid
C-Reactive Protein
Caffeine
Glutamic Acid
Interleukins
Leptin
Phenylalanine
Tryptophan
Tumor Necrosis Factor-alpha
Tyrosine
Figure
Reference
-
1. Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention [Internet]. [place unknown]: Global Initiative for Asthma;2014. cited 2015 Aug 1. Available from: http://www.ginasthma.org.2. Wenzel SE. Asthma phenotypes: the evolution from clinical to molecular approaches. Nat Med. 2012; 18:716–725.
Article3. Ye WJ, Xu WG, Guo XJ, Han FF, Peng J, Li XM, et al. Differences in airway remodeling and airway inflammation among moderate-severe asthma clinical phenotypes. J Thorac Dis. 2017; 9:2904–2914.
Article4. Kim MA, Shin SW, Park JS, Uh ST, Chang HS, Bae DJ, et al. Clinical characteristics of exacerbation-prone adult asthmatics identified by cluster analysis. Allergy Asthma Immunol Res. 2017; 9:483–490.
Article5. Khaltaev N. GARD, a new way to battle with chronic respiratory diseases, from disease oriented programmes to global partnership. J Thorac Dis. 2017; 9:4676–4689.
Article6. Yoo KH, Ahn HR, Park JK, Kim JW, Nam GH, Hong SK, et al. Burden of respiratory disease in Korea: an observational study on allergic rhinitis, asthma, COPD, and rhinosinusitis. Allergy Asthma Immunol Res. 2016; 8:527–534.
Article7. Seidell JC, Halberstadt J. The global burden of obesity and the challenges of prevention. Ann Nutr Metab. 2015; 66:Suppl 2. 7–12.
Article8. Dixon AE, Holguin F, Sood A, Salome CM, Pratley RE, Beuther DA, et al. An official American Thoracic Society Workshop report: obesity and asthma. Proc Am Thorac Soc. 2010; 7:325–335.
Article9. Lee JH, Han KD, Jung HM, Youn YH, Lee JY, Park YG, et al. Association between obesity, abdominal obesity, and adiposity and the prevalence of atopic dermatitis in young Korean adults: the Korea National Health and Nutrition Examination Survey 2008–2010. Allergy Asthma Immunol Res. 2016; 8:107–114.
Article10. Sutherland ER, Goleva E, King TS, Lehman E, Stevens AD, Jackson LP, et al. Cluster analysis of obesity and asthma phenotypes. PLoS One. 2012; 7:e36631.
Article11. Heymsfield SB, Wadden TA. Mechanisms, pathophysiology, and management of obesity. N Engl J Med. 2017; 376:254–266.
Article12. Periyalil HA, Gibson PG, Wood LG. Immunometabolism in obese asthmatics: are we there yet? Nutrients. 2013; 5:3506–3530.
Article13. Rastogi D, Fraser S, Oh J, Huber AM, Schulman Y, Bhagtani RH, et al. Inflammation, metabolic dysregulation, and pulmonary function among obese urban adolescents with asthma. Am J Respir Crit Care Med. 2015; 191:149–160.
Article14. Shore SA, Cho Y. Obesity and asthma: microbiome-metabolome interactions. Am J Respir Cell Mol Biol. 2016; 54:609–617.
Article15. Nicholson JK, Lindon JC. Systems biology: metabonomics. Nature. 2008; 455:1054–1056.16. Maniscalco M, Paris D, Melck DJ, D’Amato M, Zedda A, Sofia M, et al. Coexistence of obesity and asthma determines a distinct respiratory metabolic phenotype. J Allergy Clin Immunol. 2017; 139:1536–1547.e5.
Article17. Kelly RS, Dahlin A, McGeachie MJ, Qiu W, Sordillo J, Wan ES, et al. Asthma metabolomics and the potential for integrative omics in research and the clinic. Chest. 2017; 151:262–277.
Article18. Villaseñor A, Rosace D, Obeso D, Pérez-Gordo M, Chivato T, Barbas C, et al. Allergic asthma: an overview of metabolomic strategies leading to the identification of biomarkers in the field. Clin Exp Allergy. 2017; 47:442–456.
Article19. Kim HY, Lee HJ, Chang YJ, Pichavant M, Shore SA, Fitzgerald KA, et al. Interleukin-17-producing innate lymphoid cells and the NLRP3 inflammasome facilitate obesity-associated airway hyperreactivity. Nat Med. 2014; 20:54–61.
Article20. Leiria LO, Martins MA, Saad MJ. Obesity and asthma: beyond T(H)2 inflammation. Metabolism. 2015; 64:172–181.
Article21. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000; 894:i–xii.22. Camargo CA Jr, Rachelefsky G, Schatz M. Managing asthma exacerbations in the emergency department: summary of the National Asthma Education and Prevention Program Expert Panel Report 3 guidelines for the management of asthma exacerbations. J Allergy Clin Immunol. 2009; 124:S5–S14.
Article23. Jia CE, Zhang HP, Lv Y, Liang R, Jiang YQ, Powell H, et al. The Asthma Control Test and Asthma Control Questionnaire for assessing asthma control: systematic review and meta-analysis. J Allergy Clin Immunol. 2013; 131:695–703.
Article24. Xu KF, Luo XC, Chen Y, Zhang YJ, Li Y, Hu B, et al. The use of Juniper’s asthma quality of life questionnaire in Chinese asthmatics. Zhonghua Nei Ke Za Zhi. 2003; 42:760–763.25. Zheng J, Zhang X, Zhang L, Zhang HP, Wang L, Wang G. Interactive effects between obesity and atopy on inflammation: a pilot study for asthma phenotypic overlap. [PubMed]. Ann Allergy Asthma Immunol. 2016; 117:716–717.26. Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005; 26:319–338.27. Wang G, Baines KJ, Fu JJ, Wood LG, Simpson JL, McDonald VM, et al. Sputum mast cell subtypes relate to eosinophilia and corticosteroid response in asthma. Eur Respir J. 2016; 47:1123–1133.
Article28. Manise M, Holtappels G, Van Crombruggen K, Schleich F, Bachert C, Louis R. Sputum IgE and cytokines in asthma: relationship with sputum cellular profile. PLoS One. 2013; 8:e58388.
Article29. Pedersen F, Holz O, Lauer G, Quintini G, Kiwull-Schöne H, Kirsten AM, et al. Multi-analyte profiling of inflammatory mediators in COPD sputum--the effects of processing. Cytokine. 2015; 71:401–404.30. Miao H, Ou J, Peng Y, Zhang X, Chen Y, Hao L, et al. Macrophage ABHD5 promotes colorectal cancer growth by suppressing spermidine production by SRM. Nat Commun. 2016; 7:11716.
Article31. Chang C, Guo ZG, He B, Yao WZ. Metabolic alterations in the sera of Chinese patients with mild persistent asthma: a GC-MS-based metabolomics analysis. Acta Pharmacol Sin. 2015; 36:1356–1366.
Article32. Xia J, Wishart DS. Using MetaboAnalyst 3.0 for comprehensive metabolomics data analysis. Curr Protoc Bioinformatics. 2016; 55:14.10.1–14.10.91.
Article33. Karlsson FH, Tremaroli V, Nookaew I, Bergström G, Behre CJ, Fagerberg B, et al. Gut metagenome in European women with normal, impaired and diabetic glucose control. Nature. 2013; 498:99–103.
Article34. Quinn KD, Schedel M, Nkrumah-Elie Y, Joetham A, Armstrong M, Cruickshank-Quinn C, et al. Dysregulation of metabolic pathways in a mouse model of allergic asthma. Allergy. 2017; 72:1327–1337.
Article35. Mosen DM, Schatz M, Magid DJ, Camargo CA Jr. The relationship between obesity and asthma severity and control in adults. J Allergy Clin Immunol. 2008; 122:507–511.e6.
Article36. Kim SH, Sutherland ER, Gelfand EW. Is there a link between obesity and asthma? Allergy Asthma Immunol Res. 2014; 6:189–195.
Article37. Sideleva O, Suratt BT, Black KE, Tharp WG, Pratley RE, Forgione P, et al. Obesity and asthma: an inflammatory disease of adipose tissue not the airway. Am J Respir Crit Care Med. 2012; 186:598–605.38. Peters MC, Fahy JV. Type 2 immune responses in obese individuals with asthma. Am J Respir Crit Care Med. 2013; 188:633–634.
Article39. Zhang X, Zheng J, Zhang L, Liu Y, Chen GP, Zhang HP, et al. Systemic inflammation mediates the detrimental effects of obesity on asthma control. Allergy Asthma Proc. 2018; 39:43–50.
Article40. Darkhal P, Gao M, Ma Y, Liu D. Blocking high-fat diet-induced obesity, insulin resistance and fatty liver by overexpression of Il-13 gene in mice. Int J Obes. 2015; 39:1292–1299.
Article41. Bo S, Gambino R, Durazzo M, Ghione F, Musso G, Gentile L, et al. Associations between serum uric acid and adipokines, markers of inflammation, and endothelial dysfunction. J Endocrinol Invest. 2008; 31:499–504.
Article42. Lyngdoh T, Marques-Vidal P, Paccaud F, Preisig M, Waeber G, Bochud M, et al. Elevated serum uric acid is associated with high circulating inflammatory cytokines in the population-based Colaus study. PLoS One. 2011; 6:e19901.
Article43. Kool M, Willart MA, van Nimwegen M, Bergen I, Pouliot P, Virchow JC, et al. An unexpected role for uric acid as an inducer of T helper 2 cell immunity to inhaled antigens and inflammatory mediator of allergic asthma. Immunity. 2011; 34:527–540.
Article44. Barros R, Moreira A, Fonseca J, Delgado L, Castel-Branco MG, Haahtela T, et al. Dietary intake of α-linolenic acid and low ratio of n-6:n-3 PUFA are associated with decreased exhaled NO and improved asthma control. Br J Nutr. 2011; 106:441–450.
Article45. Xu Y, O’Brien WG 3rd, Lee CC, Myers MG Jr, Tong Q. Role of GABA release from leptin receptor-expressing neurons in body weight regulation. Endocrinology. 2012; 153:2223–2233.
Article46. Yocum GT, Gallos G, Zhang Y, Jahan R, Stephen MR, Varagic Z, et al. Targeting the γ-aminobutyric acid A receptor α4 subunit in airway smooth muscle to alleviate bronchoconstriction. Am J Respir Cell Mol Biol. 2016; 54:546–553.
Article47. Yu M, Cui FX, Jia HM, Zhou C, Yang Y, Zhang HW, et al. Aberrant purine metabolism in allergic asthma revealed by plasma metabolomics. J Pharm Biomed Anal. 2016; 120:181–189.
Article48. Cano KE, Li L, Bhatia S, Bhatia R, Forman SJ, Chen Y. NMR-based metabolomic analysis of the molecular pathogenesis of therapy-related myelodysplasia/acute myeloid leukemia. J Proteome Res. 2011; 10:2873–2881.
Article49. Park J, Rho HK, Kim KH, Choe SS, Lee YS, Kim JB. Overexpression of glucose-6-phosphate dehydrogenase is associated with lipid dysregulation and insulin resistance in obesity. Mol Cell Biol. 2005; 25:5146–5157.
Article50. Turi KN, Romick-Rosendale L, Ryckman KK, Hartert TV. A review of metabolomics approaches and their application in identifying causal pathways of childhood asthma. J Allergy Clin Immunol. 2018; 141:1191–1201.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Asthma Phenotype with Metabolic Dysfunction
- Inflammatory Receptors/Ligands as a Novel Target Against Obesity-Induced Inflammation and Metabolic Diseases
- The Role of T Cells in Obesity-Associated Inflammation and Metabolic Disease
- Obesity and Asthma Risk
- Trends of vitamin D in asthma in the pediatric population for two decades: a systematic review