Tuberc Respir Dis.
2019 Jan;82(1):35-41. 10.4046/trd.2018.0050.
Factors Associated with Indacaterol Response in Tuberculosis-Destroyed Lung with Airflow Limitation
- Affiliations
-
- 1Department of Pulmonary and Critical Care Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. ymoh55@amc.seoul.kr
- 2Department of Internal Medicine, CHA Bundang Medical Center, CHA University, Seongnam, Korea.
- 3Division of Pulmonary, Allergy and Critical Care Medicine, Department of Internal Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- KMID: 2441728
- DOI: http://doi.org/10.4046/trd.2018.0050
Abstract
- BACKGROUND
Pulmonary tuberculosis can result in anatomical sequelae, and cause airflow limitation. However, there are no treatment guidelines for patients with a tuberculosis-destroyed lung. Recently, indacaterol effectiveness in chronic obstructive pulmonary disease (COPD) patients with Tuberculosis history (INFINITY) study revealed indacaterol provided bronchodilation and symptom improvement in COPD patients with a tuberculosis-destroyed lung.
METHODS
We conducted a post-hoc subgroup analysis of the randomized controlled trial, the INFINITY study, to determine factors associated with indacaterol response in a tuberculosis-destroyed lung with airflow limitation. Data from 68 patients treated with inhaled indacaterol, were extracted and analyzed. Factors associated with the response of forced expiratory volume in one second (FEV1) to indacaterol treatment, were determined using linear regression analysis.
RESULTS
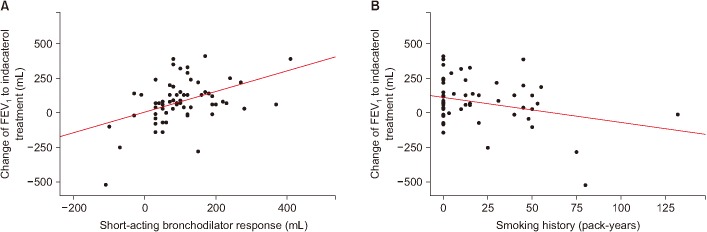
Of 62 patients included, 68% were male, and 52% had history of cigarette smoking. Patients revealed mean FEV1 of 50.5% of predicted value with mean improvement of 81.3 mL in FEV1 after indacaterol treatment for 8 weeks. Linear regression analysis revealed factors associated with response of FEV1 to indacaterol included a short duration of smoking history, and high short-acting bronchodilator response. When patients with history of smoking were excluded, factors associated with response of FEV1 to indacaterol included high short-acting bronchodilator response, and poor healthrelated quality of life score as measured by St. George's Respiratory Questionnaire for COPD.
CONCLUSION
In a tuberculosis-destroyed lung with airflow limitation, short-acting bronchodilator response and smoking history can play a critical role in predicting outcomes of indacaterol treatment.
MeSH Terms
Figure
Reference
-
1. World Health Organization Global tuberculosis report, 2017 [Internet]. Geneva: World Health Organization;2017. cited 2018 Apr 1. Available from: http://appswhoint/iris/bitstream/handle/10665/259366/9789241565516-engpdf?sequence=1.2. Harries AD, Ade S, Burney P, Hoa NB, Schluger NW, Castro JL. Successfully treated but not fit for purpose: paying attention to chronic lung impairment after TB treatment. Int J Tuberc Lung Dis. 2016; 20:1010–1014. PMID: 27393532.
Article3. Jung JW, Choi JC, Shin JW, Kim JY, Choi BW, Park IW. Pulmonary impairment in tuberculosis survivors: the Korean National Health and Nutrition Examination Survey 2008-2012. PLoS One. 2015; 10:e0141230. PMID: 26496500.
Article4. Menezes AM, Hallal PC, Perez-Padilla R, Jardim JR, Muino A, Lopez MV, et al. Tuberculosis and airflow obstruction: evidence from the PLATINO study in Latin America. Eur Respir J. 2007; 30:1180–1185. PMID: 17804445.
Article5. Pasipanodya JG, Miller TL, Vecino M, Munguia G, Garmon R, Bae S, et al. Pulmonary impairment after tuberculosis. Chest. 2007; 131:1817–1824. PMID: 17400690.
Article6. Byrne AL, Marais BJ, Mitnick CD, Lecca L, Marks GB. Tuberculosis and chronic respiratory disease: a systematic review. Int J Infect Dis. 2015; 32:138–146. PMID: 25809770.
Article7. Yum HK, Park IN. Effect of inhaled tiotropium on spirometric parameters in patients with tuberculous destroyed lung. Tuberc Respir Dis. 2014; 77:167–171.
Article8. Kim CJ, Yoon HK, Park MJ, Yoo KH, Jung KS, Park JW, et al. Inhaled indacaterol for the treatment of COPD patients with destroyed lung by tuberculosis and moderate-to-severe airflow limitation: results from the randomized INFINITY study. Int J Chron Obstruct Pulmon Dis. 2017; 12:1589–1596. PMID: 28615931.9. Chakrabarti B, Calverley PM, Davies PD. Tuberculosis and its incidence, special nature, and relationship with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2007; 2:263–272. PMID: 18229564.10. Hanania NA, Celli BR, Donohue JF, Martin UJ. Bronchodilator reversibility in COPD. Chest. 2011; 140:1055–1063. PMID: 21972384.
Article11. Bleecker ER, Emmett A, Crater G, Knobil K, Kalberg C. Lung function and symptom improvement with fluticasone propionate/ salmeterol and ipratropium bromide/albuterol in COPD: response by beta-agonist reversibility. Pulm Pharmacol Ther. 2008; 21:682–688. PMID: 18541448.12. Tashkin D, Kesten S. Long-term treatment benefits with tiotropium in COPD patients with and without short-term bronchodilator responses. Chest. 2003; 123:1441–1449. PMID: 12740259.
Article13. Hanania NA, Sharafkhaneh A, Celli B, Decramer M, Lystig T, Kesten S, et al. Acute bronchodilator responsiveness and health outcomes in COPD patients in the UPLIFT trial. Respir Res. 2011; 12:6. PMID: 21219660.
Article14. Burgel PR, Le Gros V, Decuypere L, Bourdeix I, Perez T, Deslee G. Immediate salbutamol responsiveness does not predict long-term benefits of indacaterol in patients with chronic obstructive pulmonary disease. BMC Pulm Med. 2017; 17:25. PMID: 28143447.
Article15. Rhee CK, Yoo KH, Lee JH, Park MJ, Kim WJ, Park YB, et al. Clinical characteristics of patients with tuberculosis-destroyed lung. Int J Tuberc Lung Dis. 2013; 17:67–75. PMID: 23232006.
Article16. Forey BA, Thornton AJ, Lee PN. Systematic review with metaanalysis of the epidemiological evidence relating smoking to COPD, chronic bronchitis and emphysema. BMC Pulm Med. 2011; 11:36. PMID: 21672193.
Article17. Kohansal R, Martinez-Camblor P, Agusti A, Buist AS, Mannino DM, Soriano JB. The natural history of chronic airflow obstruction revisited: an analysis of the Framingham offspring cohort. Am J Respir Crit Care Med. 2009; 180:3–10. PMID: 19342411.18. Ji W, Lim MN, Bak SH, Hong SH, Han SS, Lee SJ, et al. Differences in chronic obstructive pulmonary disease phenotypes between non-smokers and smokers. Clin Respir J. 2018; 12:666–673. PMID: 27805311.
Article19. Lamprecht B, McBurnie MA, Vollmer WM, Gudmundsson G, Welte T, Nizankowska-Mogilnicka E, et al. COPD in never smokers: results from the population-based burden of obstructive lung disease study. Chest. 2011; 139:752–763. PMID: 20884729.20. Zhou Y, Wang C, Yao W, Chen P, Kang J, Huang S, et al. COPD in Chinese nonsmokers. Eur Respir J. 2009; 33:509–518. PMID: 19251797.
Article21. Ramirez-Venegas A, Sansores RH, Perez-Padilla R, Regalado J, Velazquez A, Sanchez C, et al. Survival of patients with chronic obstructive pulmonary disease due to biomass smoke and tobacco. Am J Respir Crit Care Med. 2006; 173:393–397. PMID: 16322646.
Article22. Rezende Goncalves J, Corso Pereira M, Figueiras Pedreira De Cerqueira EM, Oliveira Magro D, Mello Moreira M, Paschoal IA. Severe obstructive disease: similarities and differences between smoker and non-smoker patients with COPD and/or bronchiectasis. Rev Port Pneumol. 2013; 19:13–18. PMID: 23017504.23. Leung CC, Yew WW, Chan CK, Tam CM, Lam CW, Chang KC, et al. Smoking and tuberculosis in Hong Kong. Int J Tuberc Lung Dis. 2003; 7:980–986. PMID: 14552569.24. Zhang J, Lin XF, Bai CX. Comparison of clinical features between non-smokers with COPD and smokers with COPD: a retrospective observational study. Int J Chron Obstruct Pulmon Dis. 2014; 9:57–63. PMID: 24426780.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Airflow Limitation on Acute Exacerbations in Patients with Destroyed Lungs by Tuberculosis
- Risk Factors for Unawareness of Obstructive Airflow Limitation among Adults with Chronic Obstructive Pulmonary Disease
- Pathophysiology of Chronic Obstructive Pulmonary Disease
- Change of Lung Volumes in Chronic Obstructive Pulmonary Disease Patients with Improvement of Airflow Limitation after Treatment
- Pathophysiology of Chronic Obstructive Pulmonary Disease