Endocrinol Metab.
2019 Mar;34(1):63-69. 10.3803/EnM.2019.34.1.63.
(99m)Tc-Pertechnetate Scintigraphy Predicts Successful Postoperative Ablation in Differentiated Thyroid Carcinoma Patients Treated with Low Radioiodine Activities
- Affiliations
-
- 1Clinic for Nuclear Medicine and Competence Center for Thyroid Diseases, Oncology Institute of Southern Switzerland, Bellinzona, Switzerland. pierpaolo.trimboli@eoc.ch
- KMID: 2441680
- DOI: http://doi.org/10.3803/EnM.2019.34.1.63
Abstract
- BACKGROUND
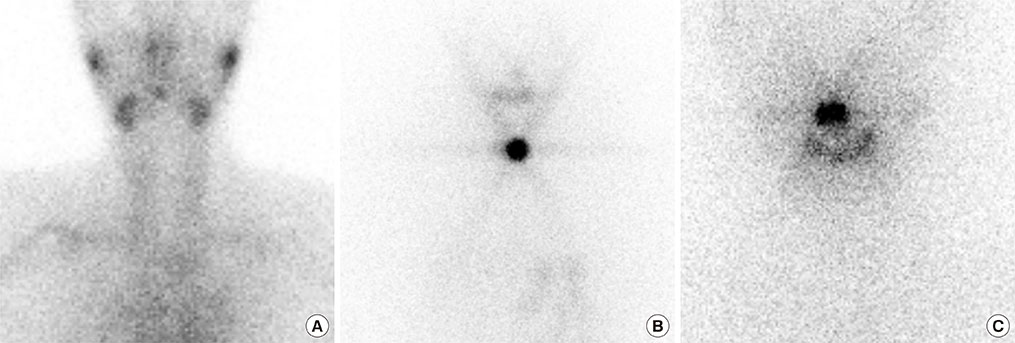
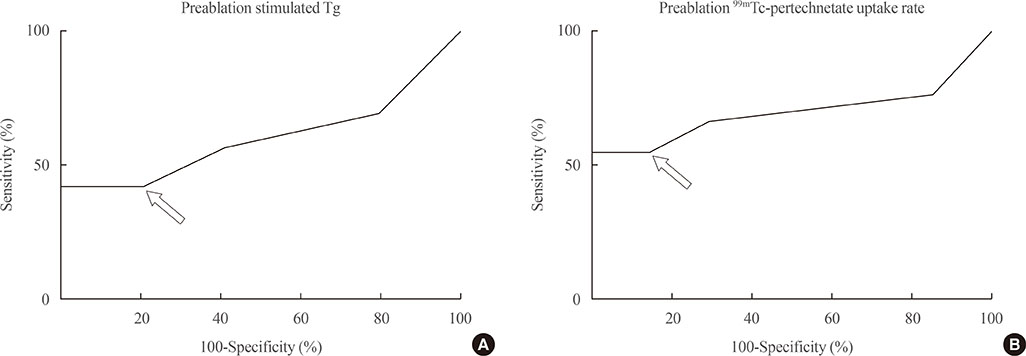
Postoperative routine radioiodine (RAI) treatment is currently debated for patients with low-risk differentiated thyroid carcinoma (DTC) patients. If performed, a low 131I activity (i.e., 1 to 2 GBq) is recommended with the aim to ablate thyroid remnant and facilitate subsequent follow-up by thyroglobulin measurement. The purpose of this study was to evaluate the relationship between postsurgical technetium-99m (99mTc)-pertechnetate scintigraphy and the rate of successful remnant ablation after low activity radioiodine ablation in patients with DTC.
METHODS
Enrolled were 193 patients with low risk DTC who underwent total thyroidectomy and RAI ablation with a fixed 1.1 GBq activity of 131I. 99mTc-pertechnetate scans were done and thyrotropin stimulated thyroglobulin (sTg) levels measured just before ablation. Ablation effectiveness was assessed 6 to 12 months later by sTg measurement, neck ultrasound and diagnostic whole body scan.
RESULTS
A negative 99mTc-perthecnetate scans was the best predictor of successful ablation (P<0.001) followed by preablative sTg levels <0.8 ng/mL (P=0.008) and 99mTc-pertechnetate uptake rate values <0.9% (P=0.065). Neither sex nor age of the patient at the time of ablation or tumor histology and size showed a significant association with the rate of successful ablation.
CONCLUSION
The 99mTc-pertechnetate scintigraphy is a simple and feasible tool to predict effectiveness of low activity 131I thyroid to ablate thyroid remnants in patients with DTC.
Keyword
MeSH Terms
Figure
Reference
-
1. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016; 26:1–133.2. Mallick U, Harmer C, Yap B, Wadsley J, Clarke S, Moss L, et al. Ablation with low-dose radioiodine and thyrotropin alfa in thyroid cancer. N Engl J Med. 2012; 366:1674–1685.
Article3. Luster M, Clarke SE, Dietlein M, Lassmann M, Lind P, Oyen WJ, et al. Guidelines for radioiodine therapy of differentiated thyroid cancer. Eur J Nucl Med Mol Imaging. 2008; 35:1941–1959.
Article4. Giovanella L, Suriano S, Ricci R, Ceriani L, Verburg FA. Postsurgical thyroid remnant estimation by 99mTc-pertechnetate scintigraphy predicts radioiodine ablation effectiveness in patients with differentiated thyroid carcinoma. Head Neck. 2011; 33:552–556.
Article5. Jung JS, Lee SM, Kim SJ, Choi J, Han SW. Prediction of the success of thyroid remnant ablation using preablative 99mTc pertechnetate scintigraphy and postablative dual 131I scintigraphy. Nucl Med Commun. 2015; 36:38–44.
Article6. Ozdemir D, Cuhaci FN, Ozdemir E, Aydin C, Ersoy R, Turkolmez S, et al. The role of postoperative Tc-99m pertechnetate scintigraphy in estimation of remnant mass and prediction of successful ablation in patients with differentiated thyroid cancer. Nucl Med Commun. 2016; 37:640–645.
Article7. Giovanella L, Suriano S, Ceriani L, Verburg FA. Undetectable thyroglobulin in patients with differentiated thyroid carcinoma and residual radioiodine uptake on a postablation whole-body scan. Clin Nucl Med. 2011; 36:109–112.
Article8. Trimboli P, Zilioli V, Imperiali M, Ceriani L, Giovanella L. High-sensitive basal serum thyroglobulin 6-12 months after thyroid ablation is strongly associated with early response to therapy and event-free survival in patients with low-to-intermediate risk differentiated thyroid carcinomas. Eur J Endocrinol. 2017; 176:497–504.
Article9. Piccardo A, Puntoni M, Bottoni G, Treglia G, Foppiani L, Bertoli M, et al. Differentiated thyroid cancer lymph-node relapse. Role of adjuvant radioactive iodine therapy after lymphadenectomy. Eur J Nucl Med Mol Imaging. 2017; 44:926–934.
Article10. Giovanella L, Toffalori E, Ceriani L, Caputo M, Verburg FA. Thyroglobulin and thyroglobulin autoantibodies measurement using the automated KRYPTOR® platform in patients with differentiated thyroid carcinoma. Horm Metab Res. 2011; 43:728–730.
Article11. Verburg FA, Luster M, Cupini C, Chiovato L, Duntas L, Elisei R, et al. Implications of thyroglobulin antibody positivity in patients with differentiated thyroid cancer: a clinical position statement. Thyroid. 2013; 23:1211–1225.
Article12. Lee CH, Jung JH, Son SH, Hong CM, Jeong JH, Jeong SY, et al. Risk factors for radioactive iodine-avid metastatic lymph nodes on post I-131 ablation SPECT/CT in low- or intermediate-risk groups of papillary thyroid cancer. PLoS One. 2018; 13:e0202644.
Article13. Gourin CG, Tufano RP, Forastiere AA, Koch WM, Pawlik TM, Bristow RE. Volume-based trends in thyroid surgery. Arch Otolaryngol Head Neck Surg. 2010; 136:1191–1198.
Article14. Schneider DF, Ojomo KA, Chen H, Sippel RS. Remnant uptake as a postoperative oncologic quality indicator. Thyroid. 2013; 23:1269–1276.
Article15. Giovanella L, Ceriani L, Trimboli P. Letter to the editor: “postoperative thyroglobulin and neck ultrasound in the risk restratification and decision to perform 131i ablation”. J Clin Endocrinol Metab. 2017; 102:1783–1784.
Article16. Giovanella L, Avram AM, Clerc J, Hindie E, Taieb D, Verburg FA. Postoperative serum thyroglobulin and neck ultrasound to drive decisions about iodine-131 therapy in patients with differentiated thyroid carcinoma: an evidence-based strategy? Eur J Nucl Med Mol Imaging. 2018; 45:2155–2158.
Article17. Campenni A, Giovanella L, Pignata SA, Vento A, Alibrandi A, Sturiale L, et al. Undetectable or low (<1 ng/ml) postsurgical thyroglobulin values do not rule out metastases in early stage differentiated thyroid cancer patients. Oncotarget. 2018; 9:17491–17500.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Usefulness of Diagnostic Scan Using Technetium-99m Pertechnetate Scintigraphy prior to the First Ablative Radioiodine Treatment in Patients with Well Differentiated Thyroid Carcinoma: A Comparative Study with Iodine-131
- Thyroid carcinoma presenting as hot nodule on technetium-99m pertechnetate thyroid scintigraphy
- Detection for Residual Thyroid Tissue and Metastatic Lesion after Total Thyroidectomy in Patients with Differentiated Thyroid Cancer: Comparison between Tc-99m Pertechnetate Scan and High Dose I-131 Therapy Scan
- Simultaneous Visualization of the Sublingual Thyroid and Lactating Breasts with Tc-99m Pertechnetate Scintigraphy
- Bowel Activity Caused by Free Tc-99m Pertechnetate Mimicking Urine Leaks during Tc-99m MAG3 Renal Scintigraphy