Endocrinol Metab.
2019 Mar;34(1):29-38. 10.3803/EnM.2019.34.1.29.
Graves' Disease: Can It Be Cured?
- Affiliations
-
- 1Department of Endocrinology and Metabolism, Academic Medical Center, University of Amsterdam, Amsterdam, The Netherlands. w.m.wiersinga@amc.uva.nl
- KMID: 2441676
- DOI: http://doi.org/10.3803/EnM.2019.34.1.29
Abstract
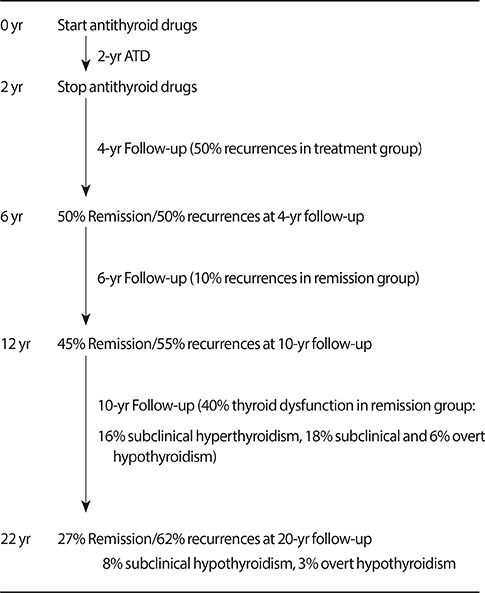
- Whether or not Graves' hyperthyroidism can be really cured, depends on the definition of "cure." If eradication of thyroid hormone excess suffices for the label "cure," then all patients can be cured because total thyroidectomy or high doses of 1¹³¹I will abolish hyperthyroidism albeit at the expense of creating another disease (hypothyroidism) requiring lifelong medication with levothyroxine. I would not call this a "cure," which I would like to define as a state with stable thyroid stimulating hormone (TSH), free thyroxine, and triiodothyronine serum concentrations in the normal range in the absence of any thyroid medication. Surgery and radioiodine are unlikely to result in so-defined cures, as their preferable aim as stated in guidelines is to cause permanent hypothyroidism. Discontinuation of antithyroid drugs is followed by 50% recurrences within 4 years; before starting therapy the risk of recurrences can be estimated with the Graves' Recurrent Events After Therapy (GREAT) score. At 20-year follow-up about 62% had developed recurrent hyperthyroidism, 8% had subclinical hypothyroidism, and 3% overt hypothyroidism related to TSH receptor blocking antibodies and thyroid peroxidase antibodies. Only 27% was in remission, and might be considered cured. If the definition of "cure" would also include the disappearance of thyroid antibodies in serum, the proportion of cured patients would become even lower.
Keyword
MeSH Terms
-
Antibodies
Antibodies, Blocking
Antithyroid Agents
Follow-Up Studies
Graves Disease*
Humans
Hyperthyroidism
Hypothyroidism
Iodide Peroxidase
Receptors, Thyrotropin
Recurrence
Reference Values
Thyroid Gland
Thyroidectomy
Thyrotropin
Thyroxine
Triiodothyronine
Antibodies
Antibodies, Blocking
Antithyroid Agents
Iodide Peroxidase
Receptors, Thyrotropin
Thyrotropin
Thyroxine
Triiodothyronine
Figure
Cited by 2 articles
-
Changes in Thyroid Peroxidase and Thyroglobulin Antibodies Might Be Associated with Graves' Disease Relapse after Antithyroid Drug Therapy
Yun Mi Choi, Mi Kyung Kwak, Sang Mo Hong, Eun-Gyoung Hong
Endocrinol Metab. 2019;34(3):268-274. doi: 10.3803/EnM.2019.34.3.268.Clinical Outcomes of Repeated Radioactive Iodine Therapy for Graves’ Disease
Min Joo Kim, Sun Wook Cho, Ye An Kim, Hoon Sung Choi, Young Joo Park, Do Joon Park, Bo Youn Cho
Endocrinol Metab. 2022;37(3):524-532. doi: 10.3803/EnM.2022.1418.
Reference
-
1. Smith TJ, Hegedus L. Graves' disease. N Engl J Med. 2016; 375:1552–1565.
Article2. Nystrom HF, Jansson S, Berg G. Incidence rate and clinical features of hyperthyroidism in a long-term iodine sufficient area of Sweden (Gothenburg) 2003-2005. Clin Endocrinol (Oxf). 2013; 78:768–776.3. Hussain YS, Hookham JC, Allahabadia A, Balasubramanian SP. Epidemiology, management and outcomes of Graves' disease-real life data. Endocrine. 2017; 56:568–578.
Article4. Wass JAH, Stewart PM. Chapter 3.3.6, Antithyroid drug treatment for thyrotoxicosis. Oxford textbook of endocrinology and diabetes. 2nd ed. Oxford: Oxford University Pres;2011. p. 476–480.5. Ross DS, Burch HB, Cooper DS, Greenlee MC, Laurberg P, Maia AL, et al. 2016 American Thyroid Association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid. 2016; 26:1343–1421.
Article6. Kahaly GJ, Bartalena L, Hegedus L, Leenhardt L, Poppe K, Pearce SH. 2018 European Thyroid Association guideline for the management of Graves' hyperthyroidism. Eur Thyroid J. 2018; 7:167–186.
Article7. Guo Z, Yu P, Liu Z, Si Y, Jin M. Total thyroidectomy vs bilateral subtotal thyroidectomy in patients with Graves' diseases: a meta-analysis of randomized clinical trials. Clin Endocrinol (Oxf). 2013; 79:739–746.8. Genovese BM, Noureldine SI, Gleeson EM, Tufano RP, Kandil E. What is the best definitive treatment for Graves' disease? A systematic review of the existing literature. Ann Surg Oncol. 2013; 20:660–667.
Article9. Liu ZW, Masterson L, Fish B, Jani P, Chatterjee K. Thyroid surgery for Graves' disease and Graves' ophthalmopathy. Cochrane Database Syst Rev. 2015; (11):CD010576.
Article10. Kautbally S, Alexopoulou O, Daumerie C, Jamar F, Mourad M, Maiter D. Greater efficacy of total thyroidectomy versus radioiodine therapy on hyperthyroidism and thyroid-stimulating immunoglobulin levels in patients with Graves' disease previously treated with antithyroid drugs. Eur Thyroid J. 2012; 1:122–128.
Article11. Lin YS, Lin JD, Hsu CC, Yu MC. The long-term outcomes of thyroid function after subtotal thyroidectomy for Graves' hyperthyroidism. J Surg Res. 2017; 220:112–118.
Article12. Huang CS, Wang M, Shun CT, Liaw KY. Factors affecting thyroid function after thyroidectomy for Graves' disease. J Formos Med Assoc. 1995; 94:423–427.13. Aung ET, Zammitt NN, Dover AR, Strachan MWJ, Seckl JR, Gibb FW. Predicting outcomes and complications following radioiodine therapy in Graves' thyrotoxicosis. Clin Endocrinol (Oxf). 2019; 90:192–199.
Article14. Laurberg P, Wallin G, Tallstedt L, Abraham-Nordling M, Lundell G, Torring O. TSH-receptor autoimmunity in Graves' disease after therapy with anti-thyroid drugs, surgery, or radioiodine: a 5-year prospective randomized study. Eur J Endocrinol. 2008; 158:69–75.
Article15. Ma C, Xie J, Wang H, Li J, Chen S. Radioiodine therapy versus antithyroid medications for Graves’ disease. Cochrane Database Syst Rev. 2016; 2:CD010094.
Article16. Fanning E, Inder WJ, Mackenzie E. Radioiodine treatment for Graves' disease: a 10-year Australian cohort study. BMC Endocr Disord. 2018; 18:94.
Article17. Hyer SL, Pratt B, Gray M, Chittenden S, Du Y, Harmer CL, et al. Dosimetry-based treatment for Graves' disease. Nucl Med Commun. 2018; 39:486–492.
Article18. Chen DY, Schneider PF, Zhang XS, He ZM, Jing J, Chen TH. Striving for euthyroidism in radioiodine therapy of Graves' disease: a 12-year prospective, randomized, open-label blinded end point study. Thyroid. 2011; 21:647–654.
Article19. Burch HB, Burman KD, Cooper DS. A 2011 survey of clinical practice patterns in the management of Graves' disease. J Clin Endocrinol Metab. 2012; 97:4549–4558.
Article20. Brito JP, Schilz S, Singh Ospina N, Rodriguez-Gutierrez R, Maraka S, Sangaralingham LR, et al. Antithyroid drugs-the most common treatment for Graves' disease in the United States: a nationwide population-based study. Thyroid. 2016; 26:1144–1145.
Article21. Burch HB, Cooper DS. Anniversary review: antithyroid drug therapy: 70 years later. Eur J Endocrinol. 2018; 179:R261–R274.22. Struja T, Fehlberg H, Kutz A, Guebelin L, Degen C, Mueller B, et al. Can we predict relapse in Graves' disease? Results from a systematic review and meta-analysis. Eur J Endocrinol. 2017; 176:87–97.
Article23. Vos XG, Endert E, Zwinderman AH, Tijssen JG, Wiersinga WM. Predicting the risk of recurrence before the start of antithyroid drug therapy in patients with Graves’ hyperthyroidism. J Clin Endocrinol Metab. 2016; 101:1381–1389.
Article24. Struja T, Kaeslin M, Boesiger F, Jutzi R, Imahorn N, Kutz A, et al. External validation of the GREAT score to predict relapse risk in Graves' disease: results from a multicenter, retrospective study with 741 patients. Eur J Endocrinol. 2017; 176:413–419.
Article25. Masiello E, Veronesi G, Gallo D, Premoli P, Bianconi E, Rosetti S, et al. Antithyroid drug treatment for Graves' disease: baseline predictive models of relapse after treatment for a patient-tailored management. J Endocrinol Invest. 2018; 41:1425–1432.
Article26. Giuliani C, Cerrone D, Harii N, Thornton M, Kohn LD, Dagia NM, et al. A TSHR-LH/CGR chimera that measures functional thyroid-stimulating autoantibodies (TSAb) can predict remission or recurrence in Graves' patients undergoing antithyroid drug (ATD) treatment. J Clin Endocrinol Metab. 2012; 97:E1080–E1087.
Article27. Kwon H, Kim WG, Jang EK, Kim M, Park S, Jeon MJ, et al. Usefulness of measuring thyroid stimulating antibody at the time of antithyroid drug withdrawal for predicting relapse of Graves disease. Endocrinol Metab (Seoul). 2016; 31:300–310.
Article28. Eliana F, Suwondo P, Asmarinah A, Harahap A, Djauzi S, Prihartono J, et al. The role of cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) gene, thyroid stimulating hormone receptor (TSHR) gene and regulatory t-cells as risk factors for relapse in patients with Graves disease. Acta Med Indones. 2017; 49:195–204.29. Garcia-Mayor RV, Alvarez-Vazquez P, Fluiters E, Valverde D, Andrade A. Long-term remission following antithyroid drug withdrawal in patients with Graves' hyperthyroidism: parameters with prognostic value. Endocrine. 2019; 63:316–322.
Article30. Mohlin E, Filipsson Nystrom H, Eliasson M. Long-term prognosis after medical treatment of Graves' disease in a northern Swedish population 2000-2010. Eur J Endocrinol. 2014; 170:419–427.
Article31. Abraham P, Avenell A, Park CM, Watson WA, Bevan JS. A systematic review of drug therapy for Graves' hyperthyroidism. Eur J Endocrinol. 2005; 153:489–498.
Article32. Razvi S, Vaidya B, Perros P, Pearce SH. What is the evidence behind the evidence-base? The premature death of block-replace antithyroid drug regimens for Graves' disease. Eur J Endocrinol. 2006; 154:783–786.
Article33. Park SM, Cho YY, Joung JY, Sohn SY, Kim SW, Chung JH. Excessive iodine intake does not increase the recurrence rate of Graves' disease after withdrawal of the antithyroid drug in an iodine-replete area. Eur Thyroid J. 2015; 4:36–42.
Article34. Volpe R. The immunomodulatory effects of anti-thyroid drugs are mediated via actions on thyroid cells, affecting thyrocyte-immunocyte signalling: a review. Curr Pharm Des. 2001; 7:451–460.
Article35. Laurberg P. Remission of Graves’ disease during anti-thyroid drug therapy. Time to reconsider the mechanism? Eur J Endocrinol. 2006; 155:783–786.
Article36. Hashizume K, Ichikawa K, Sakurai A, Suzuki S, Takeda T, Kobayashi M, et al. Administration of thyroxine in treated Graves' disease. Effects on the level of antibodies to thyroid-stimulating hormone receptors and on the risk of recurrence of hyperthyroidism. N Engl J Med. 1991; 324:947–953.37. Tamai H, Hayaki I, Kawai K, Komaki G, Matsubayashi S, Kuma K, et al. Lack of effect of thyroxine administration on elevated thyroid stimulating hormone receptor antibody levels in treated Graves' disease patients. J Clin Endocrinol Metab. 1995; 80:1481–1484.
Article38. Mori T, Sugawa H, Kosugi S, Ueda M, Hai N, Matsuda A. Recent trends in the management of Graves' hyperthyroidism in Japan: opinion survey results, especially on the combination therapy of antithyroid drug and thyroid hormone. Endocr J. 1997; 44:509–517.
Article39. Wang L, Wang B, Chen SR, Hou X, Wang XF, Zhao SH, et al. Effect of selenium supplementation on recurrent hyperthyroidism caused by Graves' disease: a prospective pilot study. Horm Metab Res. 2016; 48:559–564.
Article40. Kahaly GJ, Riedl M, Konig J, Diana T, Schomburg L. Double-blind, placebo-controlled, randomized trial of selenium in Graves hyperthyroidism. J Clin Endocrinol Metab. 2017; 102:4333–4341.
Article41. Liu X, Qiang W, Liu X, Liu L, Liu S, Gao A, et al. A second course of antithyroid drug therapy for recurrent Graves' disease: an experience in endocrine practice. Eur J Endocrinol. 2015; 172:321–326.
Article42. Kim YA, Cho SW, Choi HS, Moon S, Moon JH, Kim KW, et al. The second antithyroid drug treatment is effective in relapsed Graves' disease patients: a median 11-year follow-up study. Thyroid. 2017; 27:491–496.
Article43. Elbers L, Mourits M, Wiersinga W. Outcome of very long-term treatment with antithyroid drugs in Graves' hyperthyroidism associated with Graves' orbitopathy. Thyroid. 2011; 21:279–283.
Article44. Laurberg P, Berman DC, Andersen S, Bulow Pedersen I. Sustained control of Graves' hyperthyroidism during long-term low-dose antithyroid drug therapy of patients with severe Graves' orbitopathy. Thyroid. 2011; 21:951–956.
Article45. Azizi F, Malboosbaf R. Long-term antithyroid drug treatment: a systematic review and meta-analysis. Thyroid. 2017; 27:1223–1231.
Article46. Azizi F, Ataie L, Hedayati M, Mehrabi Y, Sheikholeslami F. Effect of long-term continuous methimazole treatment of hyperthyroidism: comparison with radioiodine. Eur J Endocrinol. 2005; 152:695–701.
Article47. Villagelin D, Romaldini JH, Santos RB, Milkos AB, Ward LS. Outcomes in relapsed Graves' disease patients following radioiodine or prolonged low dose of methimazole treatment. Thyroid. 2015; 25:1282–1290.
Article48. Irvine WJ, Gray RS, Toft AD, Seth J, Lidgard GP, Cameron EH. Spectrum of thyroid function in patient's remaining in remission after antithyroid drug therapy for thyrotoxicosis. Lancet. 1977; 2:179–181.
Article49. Wood LC, Ingbar SH. Hypothyroidism as a late sequela in patient with Graves’ disease treated with antithyroid agents. J Clin Invest. 1979; 64:1429–1436.50. Hirota Y, Tamai H, Hayashi Y, Matsubayashi S, Matsuzuka F, Kuma K, et al. Thyroid function and histology in forty-five patients with hyperthyroid Graves' disease in clinical remission more than ten years after thionamide drug treatment. J Clin Endocrinol Metab. 1986; 62:165–169.
Article51. Tamai H, Kasagi K, Takaichi Y, Takamatsu J, Komaki G, Matsubayashi S, et al. Development of spontaneous hypothyroidism in patients with Graves' disease treated with antithyroidal drugs: clinical, immunological, and histological findings in 26 patients. J Clin Endocrinol Metab. 1989; 69:49–53.
Article52. Strieder TG, Tijssen JG, Wenzel BE, Endert E, Wiersinga WM. Prediction of progression to overt hypothyroidism or hyperthyroidism in female relatives of patients with autoimmune thyroid disease using the Thyroid Events Amsterdam (THEA) score. Arch Intern Med. 2008; 168:1657–1663.
Article53. Takaichi Y, Tamai H, Honda K, Nagai K, Kuma K, Nakagawa T. The significance of antithyroglobulin and antithyroidal microsomal antibodies in patients with hyperthyroidism due to Graves' disease treated with antithyroidal drugs. J Clin Endocrinol Metab. 1989; 68:1097–1100.
Article54. Stefanic M, Karner I. Thyroid peroxidase autoantibodies are associated with a lesser likelihood of late reversion to hyperthyroidism after successful non-ablative treatment of Graves' disease in Croatian patients. J Endocrinol Invest. 2014; 37:71–77.
Article55. Lin HD, Tai FT, Chen HD, Lee SP, Chang FY, Wang GG, et al. Change of circulating thyroid autoantibody titers in Graves' hyperthyroidism after antithyroid drugs therapy. Zhonghua Yi Xue Za Zhi (Taipei). 1991; 47:86–90.56. Schott M, Eckstein A, Willenberg HS, Nguyen TB, Morgenthaler NG, Scherbaum WA. Improved prediction of relapse of Graves' thyrotoxicosis by combined determination of TSH receptor and thyroperoxidase antibodies. Horm Metab Res. 2007; 39:56–61.
Article57. Gill RG, Harmon JT, McLaren NK. Chapter 18, Autoimmune thyroid diseases. Immunologically mediated endocrine diseases. Philadelphia: Lippincott Williams & Wilkins;2002. p. 373–396.58. Wong M, Inder WJ. Alternating hyperthyroidism and hypothyroidism in Graves' disease. Clin Case Rep. 2018; 6:1684–1688.
Article59. Weetman AP. Graves' disease. N Engl J Med. 2000; 343:1236–1248.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Serum Neopterin Concentration in Children with Graves' Disease
- Euthyroid Graves' Ophthalmopathy with Negative Autoantibodies
- A clinical study of Graves' disease in children
- A Case of Graves' Disease Showing a Triad of Ophthalmopathy, Pretibial Myxedema and Thyroid Acropachy
- A Case of Pulmonary Hypertension Recurred by Graves' Disease