Acute Crit Care.
2018 Nov;33(4):197-205. 10.4266/acc.2018.00367.
Critical Care before Lung Transplantation
- Affiliations
-
- 1Department of Thoracic and Cardiovascular, Yonsei University College of Medicine, Seoul, Korea. HCPAIK@yuhs.ac
- 2Division of Pulmonology, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 3Division of Infectious Disease, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 4Department of Anesthesiology, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2441236
- DOI: http://doi.org/10.4266/acc.2018.00367
Abstract
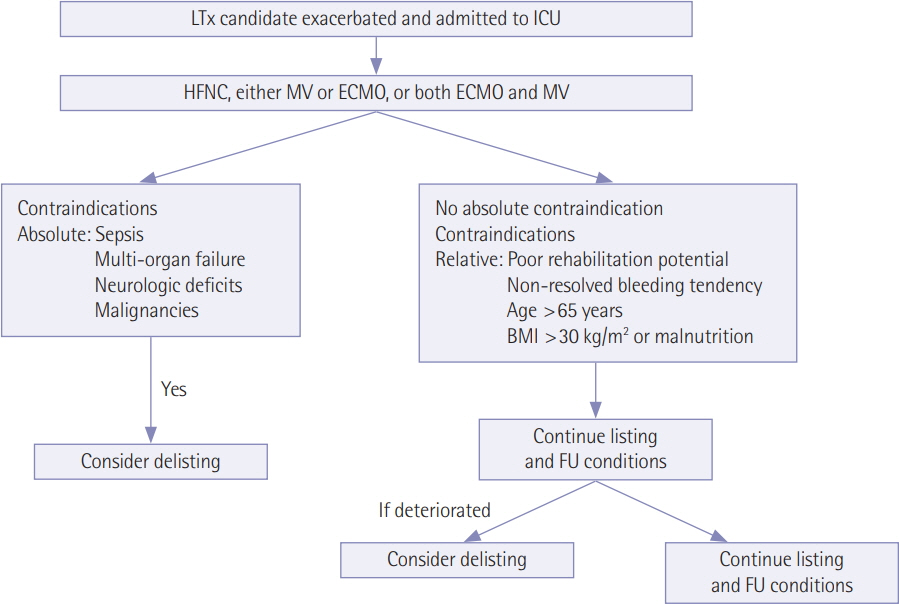
- Lung transplantation is widely accepted as the only viable treatment option for patients with end-stage lung disease. However, the imbalance between the number of suitable donor lungs available and the number of possible candidates often results in intensive care unit (ICU) admission for the latter. In the ICU setting, critical care is essential to keep these patients alive and to successfully bridge to lung transplantation. Proper management in the ICU is also one of the key factors supporting long-term success following transplantation. Critical care includes the provision of respiratory support such as mechanical ventilation (MV) and extracorporeal life support (ECLS). Accordingly, a working knowledge of the common critical care issues related to these unique patients and the early recognition and management of problems that arise before and after transplantation in the ICU setting are crucial for long-term success. In this review, we discuss the management and selection of candidates for lung transplantation as well as existing respiratory support strategies that involve MV and ECLS in the ICU setting.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Awakening in extracorporeal membrane oxygenation as a bridge to lung transplantation
Su Hwan Lee
Acute Crit Care. 2022;37(1):26-34. doi: 10.4266/acc.2022.00031.
Reference
-
1. Toronto Lung Transplant Group. Unilateral lung transplantation for pulmonary fibrosis. N Engl J Med. 1986; 314:1140–5.2. Chambers DC, Yusen RD, Cherikh WS, Goldfarb SB, Kucheryavaya AY, Khusch K, et al. The registry of the International Society for Heart and Lung Transplantation: thirty-fourth adult lung and heart-lung transplantation report-2017; focus theme: allograft ischemic time. J Heart Lung Transplant. 2017; 36:1047–59.
Article3. Egan TM, Bennett LE, Garrity ER, Grover FL, Ring WS, Robbins RC, et al. Predictors of death on the UNOS lung transplant waiting list: results of a multivariate analysis. J Heart Lung Transplant. 2001; 20:242.
Article4. De Meester J, Smits JM, Persijn GG, Haverich A. Listing for lung transplantation: life expectancy and transplant effect, stratified by type of end-stage lung disease, the Eurotransplant experience. J Heart Lung Transplant. 2001; 20:518–24.
Article5. Hosenpud JD, Bennett LE, Keck BM, Edwards EB, Novick RJ. Effect of diagnosis on survival benefit of lung transplantation for end-stage lung disease. Lancet. 1998; 351:24–7.
Article6. Charman SC, Sharples LD, McNeil KD, Wallwork J. Assessment of survival benefit after lung transplantation by patient diagnosis. J Heart Lung Transplant. 2002; 21:226–32.
Article7. Carlin BW, Lega M, Veynovich B. Management of the patient undergoing lung transplantation: an intensive care perspective. Crit Care Nurs Q. 2009; 32:49–57.8. Lau CL, Patterson GA, Palmer SM. Critical care aspects of lung transplantation. J Intensive Care Med. 2004; 19:83–104.
Article9. Pierre AF, Keshavjee S. Lung transplantation: donor and recipient critical care aspects. Curr Opin Crit Care. 2005; 11:339–44.
Article10. Simpson KP, Garrity ER. Perioperative management in lung transplantation. Clin Chest Med. 1997; 18:277–84.
Article11. Korean Network for Organ Sharing. KONOS data registry report 2016 [Internet]. Seoul: Korean Network for Organ Sharing;2017. [cited 2018 Nov 25]. Available from: https://www.konos.go.kr/konosis/index.jsp.12. Paik HC. Current perspective of lung transplantation. J Korean Med Assoc. 2016; 59:119–24.
Article13. Kim CY, Park JE, Leem AY, Song JH, Kim SY, Chung KS, et al. Prognostic value of pre-transplant mean pulmonary arterial pressure in lung transplant recipients: a single-institution experience. J Thorac Dis. 2018; 10:1578–87.
Article14. Park JE, Kim SY, Song JH, Kim YS, Chang J, Lee JG, et al. Comparison of short-term outcomes for connective tissue diseaserelated interstitial lung disease and idiopathic pulmonary fibrosis after lung transplantation. J Thorac Dis. 2018; 10:1538–47.
Article15. Yusen RD, Edwards LB, Kucheryavaya AY, Benden C, Dipchand AI, Dobbels F, et al. The registry of the International Society for Heart and Lung Transplantation: thirty-first adult lung and heart-lung transplant report-2014; focus theme: retransplantation. J Heart Lung Transplant. 2014; 33:1009–24.
Article16. Valapour M, Skeans MA, Heubner BM, Smith JM, Hertz MI, Edwards LB, et al. OPTN/SRTR 2013 Annual data report: lung. Am J Transplant. 2015; 15 Suppl 2:1–28.
Article17. Peek GJ, Mugford M, Tiruvoipati R, Wilson A, Allen E, Thalanany MM, et al. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet. 2009; 374:1351–63.
Article18. Elizur A, Sweet SC, Huddleston CB, Gandhi SK, Boslaugh SE, Kuklinski CA, et al. Pre-transplant mechanical ventilation increases short-term morbidity and mortality in pediatric patients with cystic fibrosis. J Heart Lung Transplant. 2007; 26:127–31.
Article19. Mason DP, Thuita L, Nowicki ER, Murthy SC, Pettersson GB, Blackstone EH. Should lung transplantation be performed for patients on mechanical respiratory support? The US experience. J Thorac Cardiovasc Surg. 2010; 139:765–73. e1.
Article20. Orens JB, Estenne M, Arcasoy S, Conte JV, Corris P, Egan JJ, et al. International guidelines for the selection of lung transplant candidates: 2006 update: a consensus report from the Pulmonary Scientific Council of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant. 2006; 25:745–55.21. Bartz RR, Love RB, Leverson GE, Will LR, Welter DL, Meyer KC. Pre-transplant mechanical ventilation and outcome in patients with cystic fibrosis. J Heart Lung Transplant. 2003; 22:433–8.
Article22. Baz MA, Palmer SM, Staples ED, Greer DG, Tapson VF, Davis DD. Lung transplantation after long-term mechanical ventilation: results and 1-year follow-up. Chest. 2001; 119:224–7.23. Christie JD, Edwards LB, Aurora P, Dobbels F, Kirk R, Rahmel AO, et al. The registry of the International Society for Heart and Lung Transplantation: twenty-sixth official adult lung and heart-lung transplantation report-2009. J Heart Lung Transplant. 2009; 28:1031–49.
Article24. Meyers BF, Lynch JP, Battafarano RJ, Guthrie TJ, Trulock EP, Cooper JD, et al. Lung transplantation is warranted for stable, ventilator-dependent recipients. Ann Thorac Surg. 2000; 70:1675–8.
Article25. Gottlieb J, Warnecke G, Hadem J, Dierich M, Wiesner O, Fühner T, et al. Outcome of critically ill lung transplant candidates on invasive respiratory support. Intensive Care Med. 2012; 38:968–75.
Article26. Qiu F, Lu CK, Palanzo D, Baer LD, Myers JL, Undar A. Hemodynamic evaluation of the Avalon Elite bi-caval dual lumen cannulae. Artif Organs. 2011; 35:1048–51.
Article27. Weill D, Benden C, Corris PA, Dark JH, Davis RD, Keshavjee S, et al. A consensus document for the selection of lung transplant candidates: 2014--an update from the Pulmonary Transplantation Council of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant. 2015; 34:1–15.
Article28. Jackson A, Cropper J, Pye R, Junius F, Malouf M, Glanville A. Use of extracorporeal membrane oxygenation as a bridge to primary lung transplant: 3 consecutive, successful cases and a review of the literature. J Heart Lung Transplant. 2008; 27:348–52.
Article29. Gulack BC, Hirji SA, Hartwig MG. Bridge to lung transplantation and rescue post-transplant: the expanding role of extracorporeal membrane oxygenation. J Thorac Dis. 2014; 6:1070–9.30. Lehr CJ, Zaas DW, Cheifetz IM, Turner DA. Ambulatory extracorporeal membrane oxygenation as a bridge to lung transplantation: walking while waiting. Chest. 2015; 147:1213–8.31. Hoopes CW, Kukreja J, Golden J, Davenport DL, Diaz-Guzman E, Zwischenberger JB. Extracorporeal membrane oxygenation as a bridge to pulmonary transplantation. J Thorac Cardiovasc Surg. 2013; 145:862–7.
Article32. Fuehner T, Kuehn C, Hadem J, Wiesner O, Gottlieb J, Tudorache I, et al. Extracorporeal membrane oxygenation in awake patients as bridge to lung transplantation. Am J Respir Crit Care Med. 2012; 185:763–8.
Article33. Chastre J, Fagon JY. Ventilator-associated pneumonia. Am J Respir Crit Care Med. 2002; 165:867–903.
Article34. Hermans G, De Jonghe B, Bruyninckx F, Van den Berghe G. Clinical review: critical illness polyneuropathy and myopathy. Crit Care. 2008; 12:238.
Article35. Vassilakopoulos T, Petrof BJ. Ventilator-induced diaphragmatic dysfunction. Am J Respir Crit Care Med. 2004; 169:336–41.
Article36. Strueber M. Bridges to lung transplantation. Curr Opin Organ Transplant. 2011; 16:458–61.
Article37. Turner DA, Cheifetz IM, Rehder KJ, Williford WL, Bonadonna D, Banuelos SJ, et al. Active rehabilitation and physical therapy during extracorporeal membrane oxygenation while awaiting lung transplantation: a practical approach. Crit Care Med. 2011; 39:2593–8.
Article38. Javidfar J, Brodie D, Wang D, Ibrahimiye AN, Yang J, Zwischenberger JB, et al. Use of bicaval dual-lumen catheter for adult venovenous extracorporeal membrane oxygenation. Ann Thorac Surg. 2011; 91:1763–8.
Article39. Hayes D Jr, Whitson BA, Black SM, Preston TJ, Papadimos TJ, Tobias JD. Influence of age on survival in adult patients on extracorporeal membrane oxygenation before lung transplantation. J Heart Lung Transplant. 2015; 34:832–8.
Article40. Abrams DC, Prager K, Blinderman CD, Burkart KM, Brodie D. Ethical dilemmas encountered with the use of extracorporeal membrane oxygenation in adults. Chest. 2014; 145:876–82.
Article41. Paden ML, Conrad SA, Rycus PT, Thiagarajan RR, ELSO Registry. Extracorporeal life support organization registry report 2012. ASAIO J. 2013; 59:202–10.
Article42. Orens JB, Boehler A, de Perrot M, Estenne M, Glanville AR, Keshavjee S, et al. A review of lung transplant donor acceptability criteria. J Heart Lung Transplant. 2003; 22:1183–200.
Article43. Snell GI, Griffiths A, Levvey BJ, Oto T. Availability of lungs for transplantation: exploring the real potential of the donor pool. J Heart Lung Transplant. 2008; 27:662–7.
Article44. Van Raemdonck D, Neyrinck A, Verleden GM, Dupont L, Coosemans W, Decaluwé H, et al. Lung donor selection and management. Proc Am Thorac Soc. 2009; 6:28–38.
Article45. Snell GI, Westall GP. Donor selection and management. Curr Opin Organ Transplant. 2009; 14:471–6.
Article46. Angel LF, Levine DJ, Restrepo MI, Johnson S, Sako E, Carpenter A, et al. Impact of a lung transplantation donor-management protocol on lung donation and recipient outcomes. Am J Respir Crit Care Med. 2006; 174:710–6.
Article47. Naik PM, Angel LF. Special issues in the management and selection of the donor for lung transplantation. Semin Immunopathol. 2011; 33:201–10.
Article48. Mascia L, Bosma K, Pasero D, Galli T, Cortese G, Donadio P, et al. Ventilatory and hemodynamic management of potential organ donors: an observational survey. Crit Care Med. 2006; 34:321–7.
Article49. Mascia L, Pasero D, Slutsky AS, Arguis MJ, Berardino M, Grasso S, et al. Effect of a lung protective strategy for organ donors on eligibility and availability of lungs for transplantation: a randomized controlled trial. JAMA. 2010; 304:2620–7.50. Rajagopal K, Hoeper MM. State of the art: bridging to lung transplantation using artificial organ support technologies. J Heart Lung Transplant. 2016; 35:1385–98.
Article51. Collaud S, Benden C, Ganter C, Hillinger S, Opitz I, Schneiter D, et al. Extracorporeal life support as bridge to lung retransplantation: a multicenter pooled data analysis. Ann Thorac Surg. 2016; 102:1680–6.
Article52. Biscotti M, Sonett J, Bacchetta M. ECMO as bridge to lung transplant. Thorac Surg Clin. 2015; 25:17–25.
Article53. Hayanga AJ, Aboagye J, Esper S, Shigemura N, Bermudez CA, D’Cunha J, et al. Extracorporeal membrane oxygenation as a bridge to lung transplantation in the United States: an evolving strategy in the management of rapidly advancing pulmonary disease. J Thorac Cardiovasc Surg. 2015; 149:291–6.
Article54. Combes A, Bacchetta M, Brodie D, Müller T, Pellegrino V. Extracorporeal membrane oxygenation for respiratory failure in adults. Curr Opin Crit Care. 2012; 18:99–104.
Article55. Hayanga JW, Lira A, Aboagye JK, Hayanga HK, D’Cunha J. Extracorporeal membrane oxygenation as a bridge to lung transplantation: what lessons might we learn from volume and expertise? Interact Cardiovasc Thorac Surg. 2016; 22:406–10.
Article56. Crotti S, Iotti GA, Lissoni A, Belliato M, Zanierato M, Chierichetti M, et al. Organ allocation waiting time during extracorporeal bridge to lung transplant affects outcomes. Chest. 2013; 144:1018–25.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Critical Care Management Following Lung Transplantation
- Critical Care after Lung Transplantation
- Recipient Management before Lung Transplantation
- Donor Selection, Management, and Procurement for Lung Transplantation
- Comment on “Risk factors for intensive care unit readmission after lung transplantation: a retrospective cohort study”