Neonatal Med.
2019 Feb;26(1):24-33. 10.5385/nm.2019.26.1.24.
Association between the Nutritional Status at Birth and Need for Respiratory Support on the First Day of Life
- Affiliations
-
- 1Department of Pediatrics, School of Medicine, Kyungpook National University, Daegu, Korea. park_sh@knu.ac.kr
- 2Department of Pediatrics, Kyungpook National University Hospital, Daegu, Korea.
- 3Department of Pediatrics, Catholic University of Daegu School of Medicine, Daegu, Korea.
- KMID: 2440697
- DOI: http://doi.org/10.5385/nm.2019.26.1.24
Abstract
- PURPOSE
Nutritional markers, such as total protein, albumin, and vitamin D have been reportedly associated with neonatal outcomes. This study aimed to assess the correlation between nutritional markers at birth and the need for respiratory support on the first day of life.
METHODS
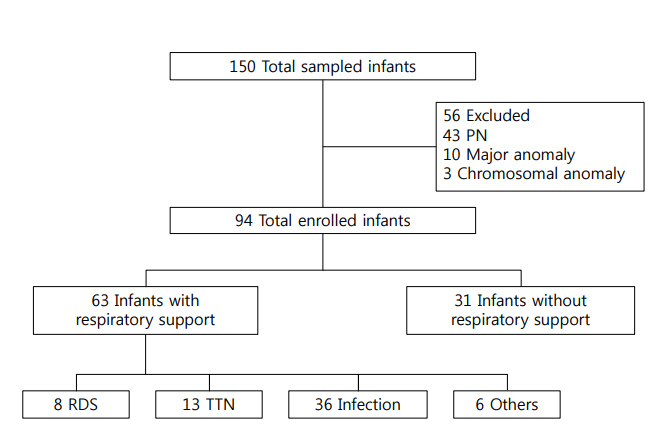
This retrospective study included 94 newborns admitted to the neonatal intensive care unit of Kyungpook National University Children's Hospital between March and December 2017. We measured levels of nutritional markers, including serum total protein, albumin, ferritin, 25-hydroxyvitamin D (25-OHD), and prealbumin, from cord blood or blood sample within 24 hours after birth. Respiratory support was defined as the use of nasal continuous positive airway pressure, humidified high-flow nasal cannula, or mechanical ventilation on the first day of life.
RESULTS
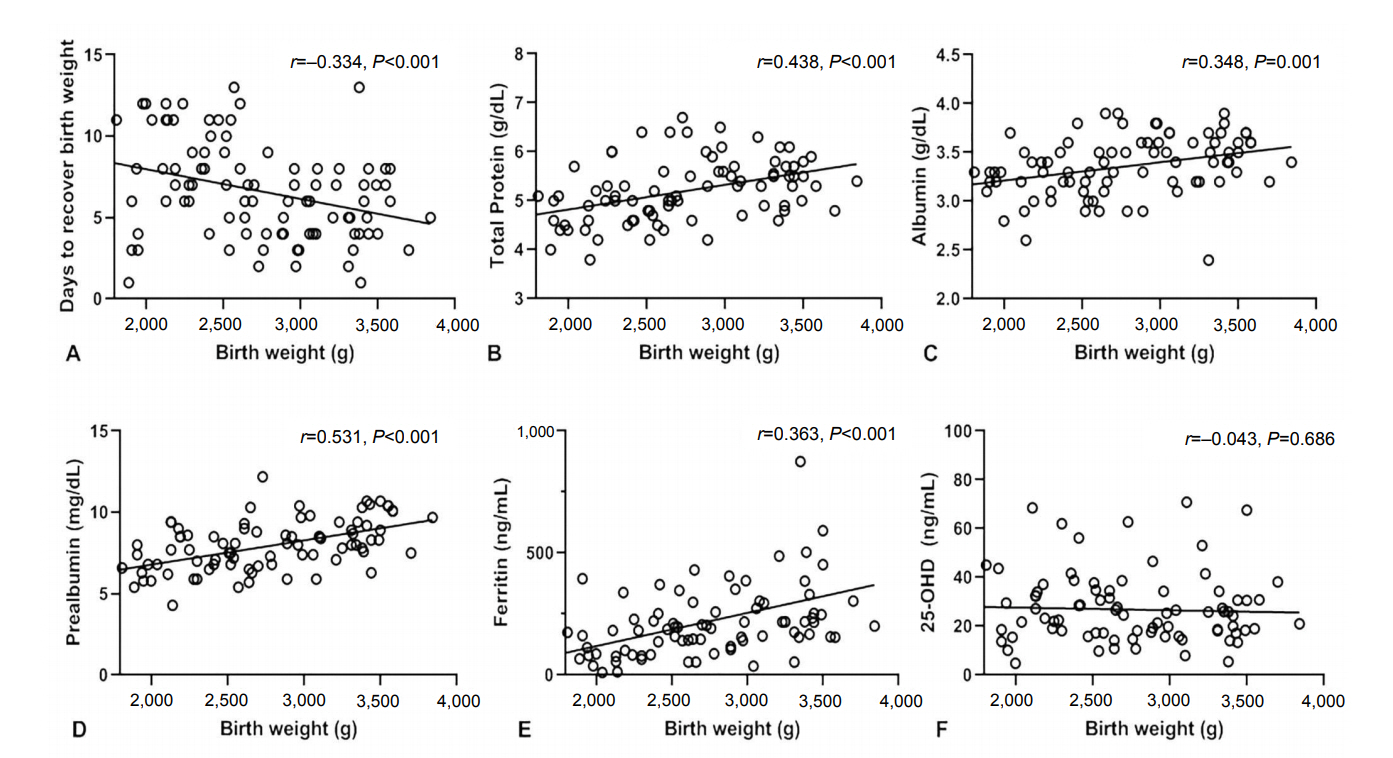
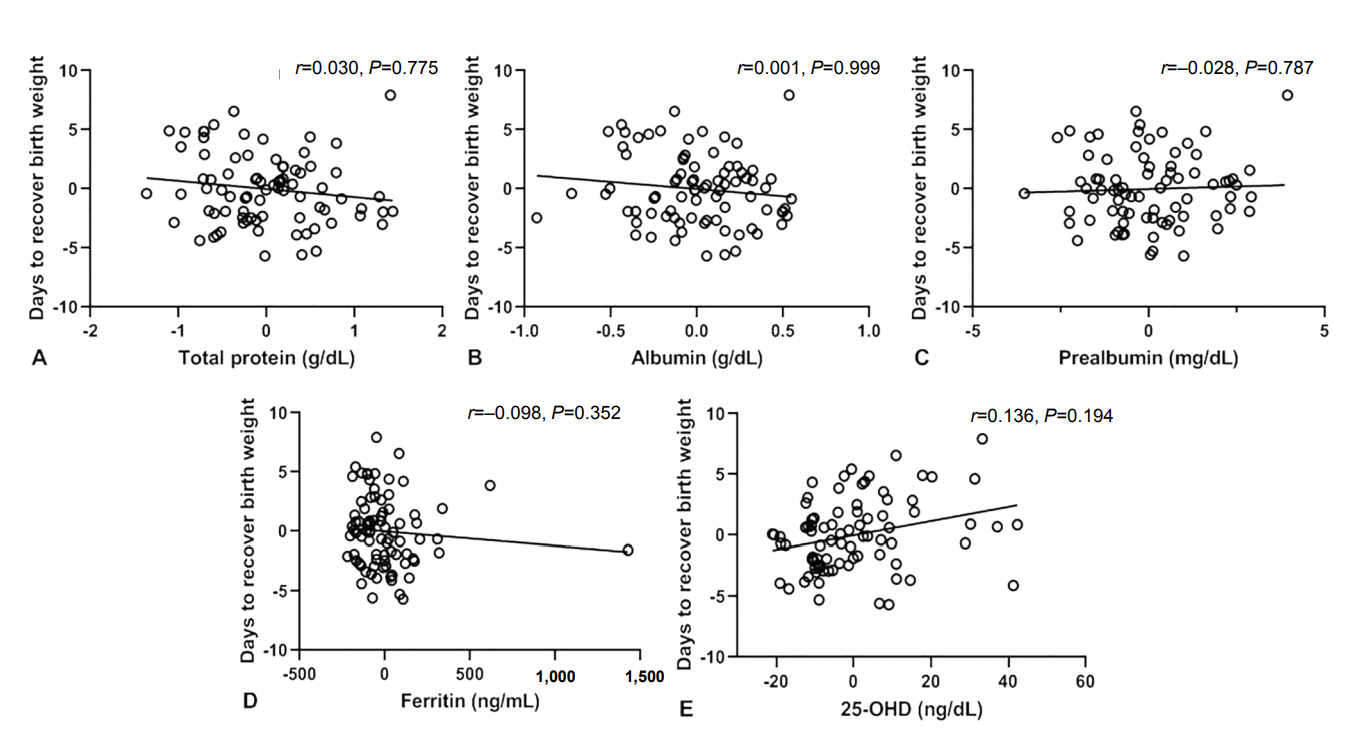
The mean gestational age and birth weight were 36.6±2.3 weeks and 2,714±575 g, respectively. Serum total protein, albumin, prealbumin, and ferritin levels at birth were significantly correlated with gestational age and birth weight. Total protein, albumin, ferritin, and 25-OHD levels were not correlated with the time to recover birth weight after adjusting for gestational age. Moreover, prealbumin levels at birth were significantly lower in small-for-gestational-age infants than in appropriate-for-gestational-age infants. The need for respiratory support on the first day of life decreased 0.058- and 0.001-fold for every 1 g/dL increase in serum total protein (95% confidence interval [CI], 0.004 to 0.833; P=0.036) and albumin (95% CI, 0.000 to 0.136; P=0.009) levels, respectively.
CONCLUSION
Nutritional status at birth could be associated with the need for respiratory support on the first day of life, regardless of the Apgar score.
MeSH Terms
-
Apgar Score
Birth Weight
Catheters
Continuous Positive Airway Pressure
Ferritins
Fetal Blood
Gestational Age
Gyeongsangbuk-do
Humans
Infant
Infant, Newborn
Intensive Care, Neonatal
Nutritional Status*
Parturition*
Prealbumin
Respiration, Artificial
Respiratory Insufficiency
Retrospective Studies
Vitamin D
Ferritins
Prealbumin
Vitamin D
Figure
Reference
-
1. Delliere S, Cynober L. Is transthyretin a good marker of nutritional status? Clin Nutr. 2017; 36:364–70.2. Mol N, Kwinta P. How to determine the nutritional status of preterm babies?: review of the literature. Dev Period Med. 2015; 19:3 Pt 1:324–9.3. Jung JA, Park EA, Seo JW, Lee SJ. The utility of serum prealbumin as a biochemical marker for nutritional adequacy in neonates. J Korean Pediatr Soc. 2000; 43:605–10.4. Moskowitz SR, Pereira G, Spitzer A, Heaf L, Amsel J, Watkins JB. Prealbumin as a biochemical marker of nutritional adequacy in premature infants. J Pediatr. 1983; 102:749–53.5. Bonsante F, Ramful D, Samperiz S, Daniel S, Godeluck A, Robillard PY, et al. Low plasma protein levels at birth are associated with poor cardiovascular adaptation and serious adverse outcome in infants with gestational age <32 weeks: the ProHémie study. Neonatology. 2017; 112:114–21.6. Iacobelli S, Bonsante F, Lacoutiere C, Ferdynus C, Cottenet J, Binquet C, et al. Hypoproteinemia on the first day of life and adverse outcome in very preterm infants admitted to the neonatal intensive care unit. J Perinatol. 2012; 32:520–4.7. Iacobelli S, Bonsante F, Quantin C, Robillard PY, Binquet C, Gouyon JB. Total plasma protein in very preterm babies: prognostic value and comparison with illness severity scores. PLoS One. 2013; 8:e62210.8. Torer B, Hanta D, Yapakci E, Gokmen Z, Parlakgumus A, Gulcan H, et al. Association of serum albumin level and mortality in premature infants. J Clin Lab Anal. 2016; 30:867–72.9. Yang CY, Li BY, Xu P, Yang YJ, Yang QZ. Correlation of serum albumin with the clinical features and prognosis of preterm neonates in the neonatal intensive care unit. Clin Exp Obstet Gynecol. 2016; 43:149–53.10. Onwuneme C, Martin F, McCarthy R, Carroll A, Segurado R, Murphy J, et al. The association of vitamin D status with acute respiratory morbidity in preterm infants. J Pediatr. 2015; 166:1175–80.11. Cetinkaya M, Cekmez F, Erener-Ercan T, Buyukkale G, Demirhan A, Aydemir G, et al. Maternal/neonatal vitamin D deficiency: a risk factor for bronchopulmonary dysplasia in preterms? J Perinatol. 2015; 35:813–7.12. Lykkedegn S, Sorensen GL, Beck-Nielsen SS, Christesen HT. The impact of vitamin D on fetal and neonatal lung maturation. A systematic review. Am J Physiol Lung Cell Mol Physiol. 2015; 308:L587–602.13. Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013; 13:59.14. Georgieff MK, Sasanow SR, Mammel MC, Ophoven J, Pereira GR. Cord prealbumin values in newborn infants: effect of prenatal steroids, pulmonary maturity, and size for dates. J Pediatr. 1986; 108:972–6.15. Su PH, Wang SL, Chen JY, Hu JM, Chang HP, Chen SJ. Transthyretin levels are not related to Apgar score in low birth weight and very low birth weight infants. Early Hum Dev. 2008; 84:533–8.16. Við Streym S, Kristine Moller U, Rejnmark L, Heickendorff L, Mosekilde L, Vestergaard P. Maternal and infant vitamin D status during the first 9 months of infant life-a cohort study. Eur J Clin Nutr. 2013; 67:1022–8.17. Ariyawatkul K, Lersbuasin P. Prevalence of vitamin D deficiency in cord blood of newborns and the association with maternal vitamin D status. Eur J Pediatr. 2018; 177:1541–5.18. McCarthy EK, Kenny LC, Hourihane JOB, Irvine AD, Murray DM, Kiely ME. Impact of maternal, antenatal and birth-associated factors on iron stores at birth: data from a prospective maternal-infant birth cohort. Eur J Clin Nutr. 2017; 71:782–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Enternal Nutritional Support on Tube-fed Elderly Patients
- Nutritional Support, Gastric Residual Volume and Nutritional Status during Enteral Nutrition in Intensive Care Unit Patients
- Degree of Nutritional Support and Nutritional Status in MICU Patients
- Nutritional Support in Patients with Inflammatory Bowel Diseases
- Attitudes of Medical Staff and Factors Related to Nutritional Support for Patient Care in a University Hospital