Ann Hepatobiliary Pancreat Surg.
2019 Feb;23(1):8-12. 10.14701/ahbps.2019.23.1.8.
Surgical indications for focal nodular hyperplasia of the liver: Single-center experience of 48 adult cases
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. shwang@amc.seoul.kr
- KMID: 2439040
- DOI: http://doi.org/10.14701/ahbps.2019.23.1.8
Abstract
- BACKGROUNDS/AIMS
Focal nodular hyperplasia (FNH) is one of the most common benign tumors of the liver. There is still a lack of evidence on surgical indications for FNH. This study intended to analyze the surgical indications for FNH.
METHODS
We analyzed 48 cases of FNH diagnosed after hepatic resection.
RESULTS
Common reasons leading to surgical resection were diagnostic uncertainty (n=31), and persistent symptoms (n=8). None of our patients had a past history of contraceptive use. Percutaneous biopsy was performed in 14 patients and FNH was diagnosed in nine patients, and hepatic adenoma, hepatocellular carcinoma, plasmacytoma, angiosarcoma, and atypical hepatocellular proliferation in one patient each. Minor hepatectomy (n=37) was performed more frequently than major hepatectomy (n=11). Open hepatectomy (n=29) was performed more frequently than laparoscopic hepatectomy (n=19), but laparoscopic and minimally-invasive surgery was frequently performed during the late phase of the study period. Postoperative surgical complications occurred in two patients (4.1%).
CONCLUSIONS
FNH can be diagnosed by imaging studies, but surgical treatment may be considered in cases of diagnostic uncertainty or persistent symptoms.
Keyword
MeSH Terms
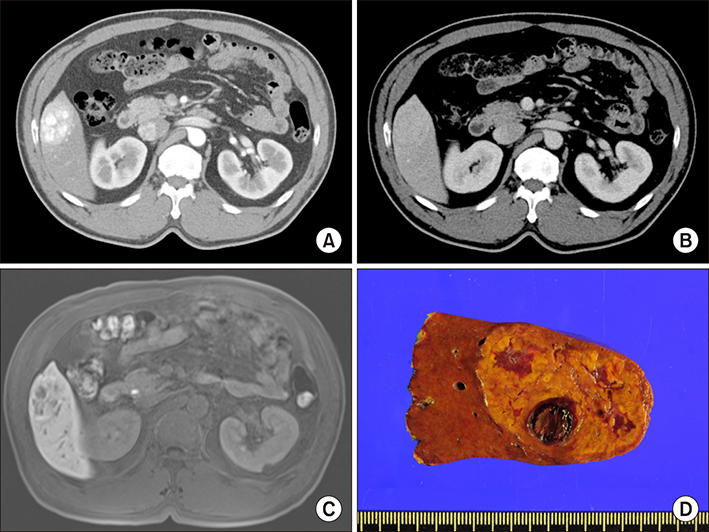
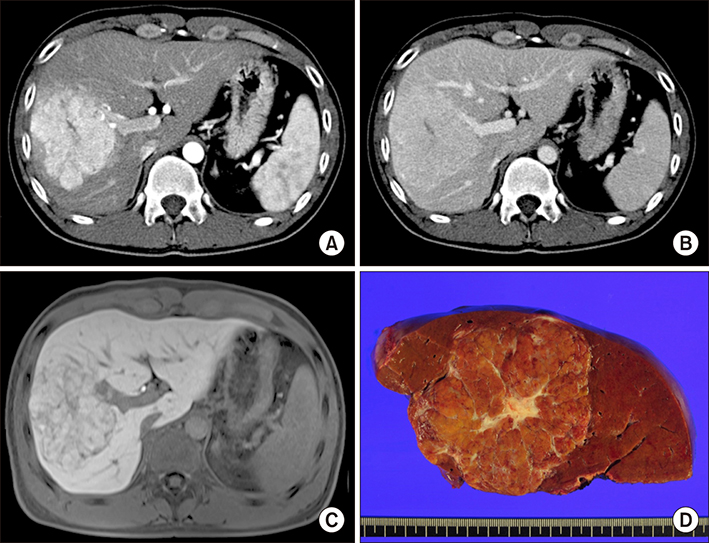
Figure
Reference
-
1. Stocker JT, Ishak KG. Focal nodular hyperplasia of the liver: a study of 21 pediatric cases. Cancer. 1981; 48:336–345.
Article2. Di Stasi M, Caturelli E, De Sio I, Salmi A, Buscarini E, Buscarini L. Natural history of focal nodular hyperplasia of the liver: an ultrasound study. J Clin Ultrasound. 1996; 24:345–350.
Article3. Mathieu D, Kobeiter H, Maison P, Rahmouni A, Cherqui D, Zafrani ES, et al. Oral contraceptive use and focal nodular hyperplasia of the liver. Gastroenterology. 2000; 118:560–564.
Article4. Leconte I, Van Beers BE, Lacrosse M, Sempoux C, Jamart J, Materne R, et al. Focal nodular hyperplasia: natural course observed with CT and MRI. J Comput Assist Tomogr. 2000; 24:61–66.
Article5. Kuo YH, Wang JH, Lu SN, Hung CH, Wei YC, Hu TH, et al. Natural course of hepatic focal nodular hyperplasia: a long-term follow-up study with sonography. J Clin Ultrasound. 2009; 37:132–137.
Article6. Song KH, Lee KU, Kim JH, Shin WY, Lee HW, Yi NJ, et al. Clinical analysis of focal nodular hyperplasia of the liver in 11 patients. Korean J Hepatobiliary Pancreat Surg. 2007; 11:41–46.7. Cho HD, Hwang S, Lee YJ, Park KM, Kim KH, Kim JC, et al. Changes in the types of liver diseases requiring hepatic resection: a single-institution experience of 9016 cases over a 10-year period. Korean J Hepatobiliary Pancreat Surg. 2016; 20:49–52.
Article8. Jung DH, Hwang S, Hong SM, Kim KH, Ahn CS, Moon DB, et al. Clinico-pathological correlation of hepatic angiomyolipoma: a series of 23 resection cases. ANZ J Surg. 2018; 88:E60–E65.
Article9. Hau HM, Atanasov G, Tautenhahn HM, Ascherl R, Wiltberger G, Schoenberg MB, et al. The value of liver resection for focal nodular hyperplasia: resection yes or no? Eur J Med Res. 2015; 20:86.
Article10. Bröker MEE, Klompenhouwer AJ, Gaspersz MP, Alleleyn AME, Dwarkasing RS, Pieters IC, et al. Growth of focal nodular hyperplasia is not a reason for surgical intervention, but patients should be referred to a tertiary referral centre. World J Surg. 2018; 42:1506–1513.
Article11. Mamone G, Caruso S, Cortis K, Miraglia R. Complete spontaneous regression of giant focal nodular hyperplasia of the liver: magnetic resonance imaging evaluation with hepatobiliary contrast media. World J Gastroenterol. 2016; 22:10461–10464.
Article12. Lee J, Jeong WK, Lim HK, Kim AY. Focal nodular hyperplasia of the liver: contrast-enhanced ultrasonographic features with sonazoid. J Ultrasound Med. 2018; 37:1473–1480.
Article13. Kitao A, Matsui O, Yoneda N, Kita R, Kozaka K, Kobayashi S, et al. Differentiation between hepatocellular carcinoma showing hyperintensity on the hepatobiliary phase of gadoxetic acid-enhanced MRI and focal nodular hyperplasia by CT and MRI. AJR Am J Roentgenol. 2018; 211:347–357.
Article14. Jung DH, Hwang S, Kim KH, Hong SM, Lee YJ, Ahn CS, et al. Clinicopathological features and post-resection prognosis of double primary hepatocellular carcinoma and intrahepatic cholangiocarcinoma. World J Surg. 2017; 41:825–834.
Article