J Breast Cancer.
2017 Sep;20(3):264-269. 10.4048/jbc.2017.20.3.264.
Clinicopathologic Characteristics of Pregnancy-Associated Breast Cancer: Results of Analysis of a Nationwide Breast Cancer Registry Database
- Affiliations
-
- 1Department of Surgery, Bundang Jesaeng General Hospital, Seongnam, Korea.
- 2Department of Surgery, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 3Department of Surgery, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
- 4Division of Breast and Endocrine Surgery, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 5Department of Surgery, Seoul National University Bundang Hospital, Seongnam, Korea.
- 6Department of Surgery, Ewha Womans University Mokdong Hospital, Ewha Womans University School of Medicine, Seoul, Korea.
- 7Department of Surgery, Chonbuk National University Hospital, Chonbuk National University Medical School, Jeonju, Korea.
- 8Department of Surgery, Korea Cancer Center Hospital, Korea Institute of Radiological & Medical Sciences, Seoul, Korea. hyunah@kcch.re.kr
- KMID: 2438993
- DOI: http://doi.org/10.4048/jbc.2017.20.3.264
Abstract
- PURPOSE
This study aimed to evaluate the clinicopathological characteristics of pregnancy-associated breast cancer (PABC) in comparison with non-pregnancy associated breast cancer (non-PABC).
METHODS
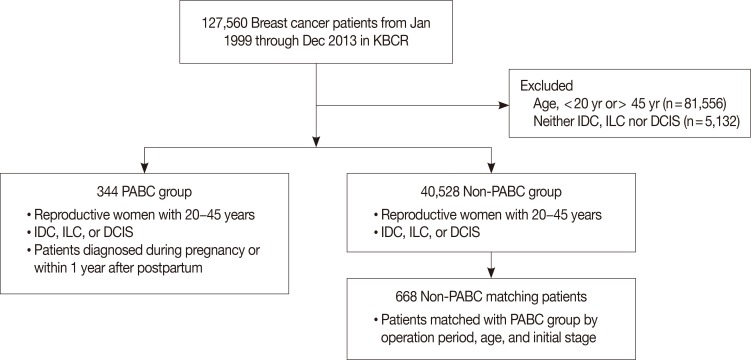
A total of 344 eligible patients with PABC were identified in the Korean Breast Cancer Society Registry database. PABC was defined as ductal carcinoma in situ, invasive ductal carcinoma, or invasive lobular carcinoma diagnosed during pregnancy or within 1 year after the birth of a child. Patients with non-PABC were selected from the same database using a 1:2 matching method. The matching variables were operation, age, and initial stage.
RESULTS
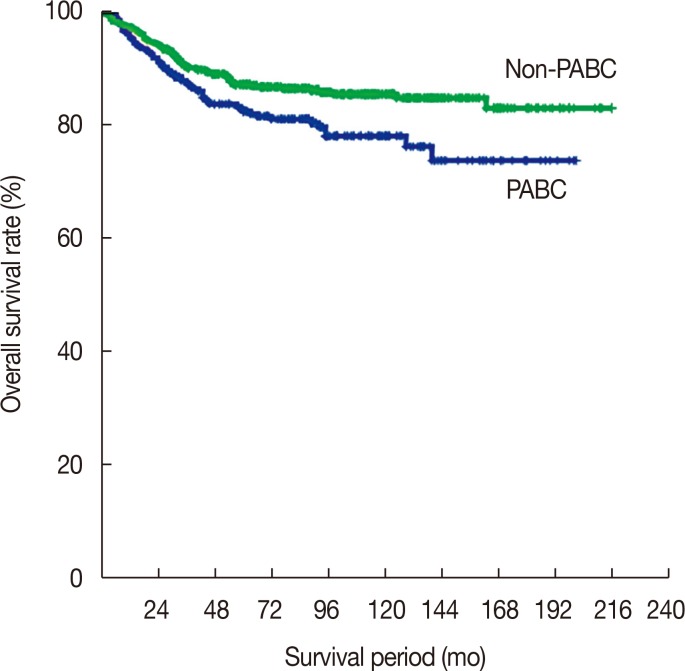
Patients with PABC had significantly lower survival rates than patient with non-PABC (10-year survival rate: PABC, 76.4%; non-PABC, 85.1%; p=0.011). PABC patients had higher histologic grade and were more frequently hormone receptor negative than non-PABC patients. Being overweight (body mass index [BMI], ≥23 kg/m²), early menarche (≤13 years), late age at first childbirth (≥30 years), and a family history of breast cancer were more common in the PABC group than in the non-PABC group. Multivariate analysis showed the following factors to be significantly associated with PABC (vs. non-PABC): early menarche (odds ratio [OR], 2.165; 95% confidence interval [CI], 1.566-2.994; p<0.001), late age at first childbirth (OR, 2.446; 95% CI, 1.722-3.473; p<0.001), and being overweight (OR, 1.389; 95% CI, 1.007-1.917; p=0.045).
CONCLUSION
Early menarche, late age at first childbirth, and BMI ≥23 kg/m² were more associated with PABC than non-PABC.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Neoadjuvant Chemotherapy and Prognosis of Pregnancy-Associated Breast Cancer: A Time-Trends Study of the Korean Breast Cancer Registry Database
Soo Youn Bae, Ku Sang Kim, Jeong-Soo Kim, Sae Byul Lee, Byeong-Woo Park, Seok Won Lee, Hyouk Jin Lee, Hong Kyu Kim, Ji-Young You, Seung Pil Jung,
J Breast Cancer. 2018;21(4):425-432. doi: 10.4048/jbc.2018.21.e58.
Reference
-
1. Pavlidis N, Pentheroudakis G. The pregnant mother with breast cancer: diagnostic and therapeutic management. Cancer Treat Rev. 2005; 31:439–447. PMID: 15946802.
Article2. Bodner-Adler B, Bodner K, Zeisler H. Breast cancer diagnosed during pregnancy. Anticancer Res. 2007; 27:1705–1707. PMID: 17595801.3. Bladström A, Anderson H, Olsson H. Worse survival in breast cancer among women with recent childbirth: results from a Swedish population-based register study. Clin Breast Cancer. 2003; 4:280–285. PMID: 14651773.
Article4. Azim HA Jr, Santoro L, Russell-Edu W, Pentheroudakis G, Pavlidis N, Peccatori FA. Prognosis of pregnancy-associated breast cancer: a metaanalysis of 30 studies. Cancer Treat Rev. 2012; 38:834–842. PMID: 22785217.
Article5. Ahn SH, Son BH, Kim SW, Kim SI, Jeong J, Ko SS, et al. Poor outcome of hormone receptor-positive breast cancer at very young age is due to tamoxifen resistance: nationwide survival data in Korea: a report from the Korean Breast Cancer Society. J Clin Oncol. 2007; 25:2360–2368. PMID: 17515570.6. Ko BS, Noh WC, Kang SS, Park BW, Kang EY, Paik NS, et al. Changing patterns in the clinical characteristics of Korean breast cancer from 1996-2010 using an online nationwide breast cancer database. J Breast Cancer. 2012; 15:393–400. PMID: 23346167.
Article7. Park HS, Chae BJ, Song BJ, Jung SS, Han W, Nam SJ, et al. Effect of axillary lymph node dissection after sentinel lymph node biopsy on overall survival in patients with T1 or T2 node-positive breast cancer: report from the Korean Breast Cancer Society. Ann Surg Oncol. 2014; 21:1231–1236. PMID: 24318094.
Article8. Inoue S, Zimmet P, Caterson I, Chunming C, Ikeda Y, Khalid AK, et al. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment. Sydney: Health Communications Australia;2000. p. 19.9. Rodriguez AO, Chew H, Cress R, Xing G, McElvy S, Danielsen B, et al. Evidence of poorer survival in pregnancy-associated breast cancer. Obstet Gynecol. 2008; 112:71–78. PMID: 18591310.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Breast Cancer During Pregnancy
- Breast Cancer during Pregnancy
- The Basic Facts of Korean Breast Cancer in 2013: Results of a Nationwide Survey and Breast Cancer Registry Database
- The Basic Facts of Korean Breast Cancer in 2012: Results from a Nationwide Survey and Breast Cancer Registry Database
- Basic Findings Regarding Breast Cancer in Korea in 2015: Data from a Breast Cancer Registry