J Breast Cancer.
2017 Sep;20(3):254-263. 10.4048/jbc.2017.20.3.254.
Prognostic Influence of Preoperative Fibrinogen to Albumin Ratio for Breast Cancer
- Affiliations
-
- 1Department of Surgery, Seoul National University Boramae Medical Center, Seoul, Korea. kiterius@snu.ac.kr
- 2Department of Laboratory Medicine, Seoul National University Boramae Medical Center, Seoul, Korea.
- 3Department of Biostatistics, Seoul National University Boramae Medical Center, Seoul, Korea.
- 4Department of Pathology, Seoul National University Boramae Medical Center, Seoul, Korea.
- 5Department of Radiation Oncology, Seoul National University Boramae Medical Center, Seoul, Korea.
- KMID: 2438992
- DOI: http://doi.org/10.4048/jbc.2017.20.3.254
Abstract
- PURPOSE
Elevated serum concentration of fibrinogen and decreased serum concentration of albumin have been reported to be markers of elevated systemic inflammation. We attempted to investigate the prognostic influence of preoperative fibrinogen to albumin ratio (FAR) for breast cancer.
METHODS
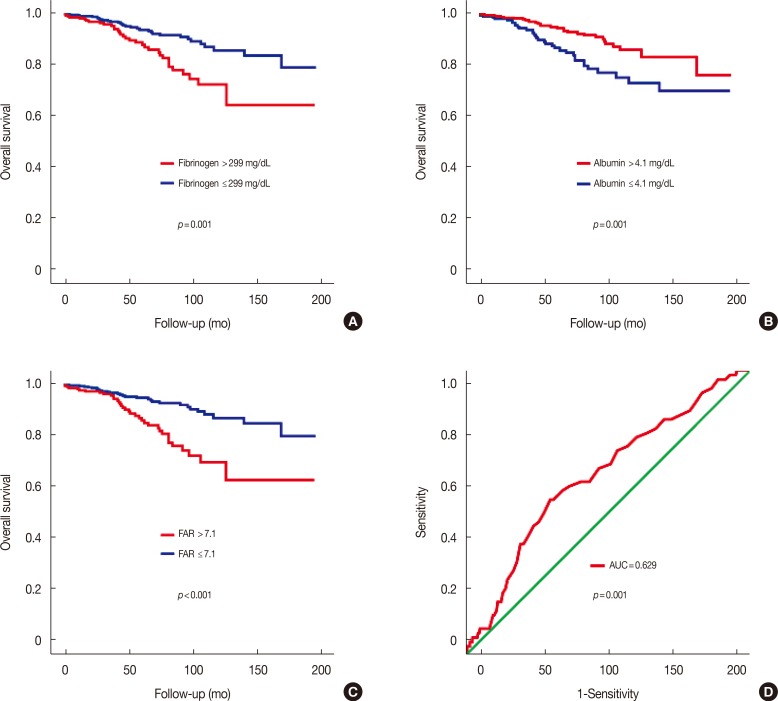
Data from 793 consecutive primary breast cancer patients were retrospectively analyzed. Serum levels of fibrinogen and albumin were tested before curative surgery. Subjects were grouped into two groups according to the cutoff value determined by performing the receiver operating characteristic curve analysis: the high FAR group (FAR>7.1) and the low FAR group (FAR≤7.1). Overall survival was assessed using the Kaplan-Meier estimator. Independent prognostic significance was analyzed using the Cox proportional hazards model.
RESULTS
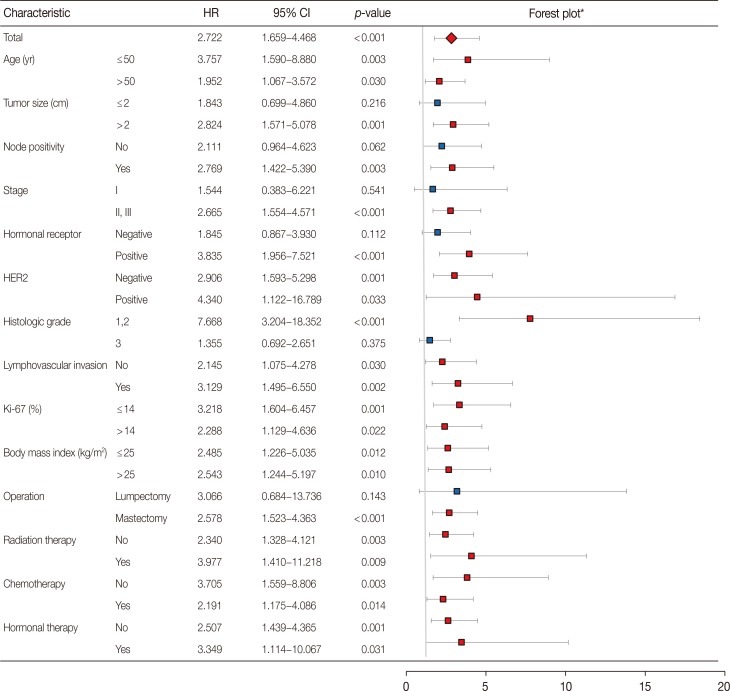
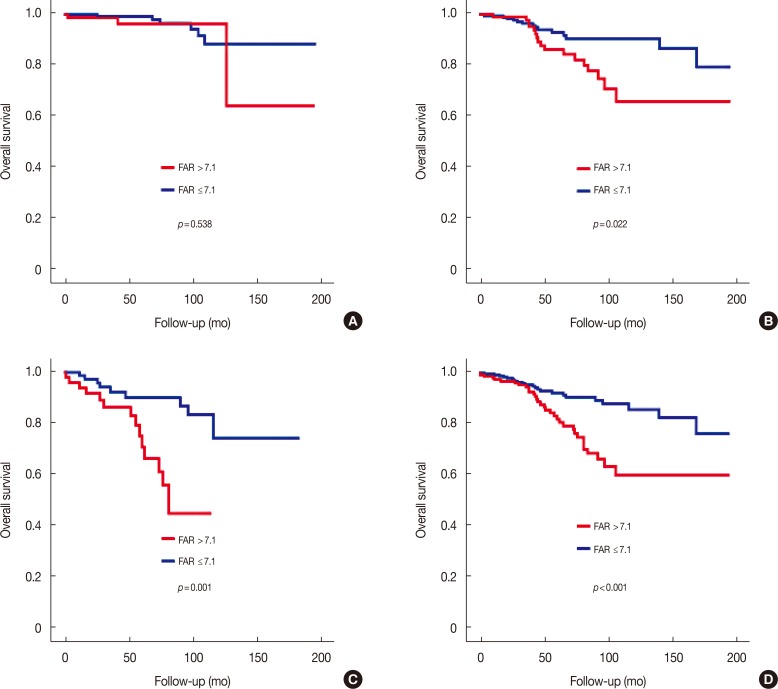
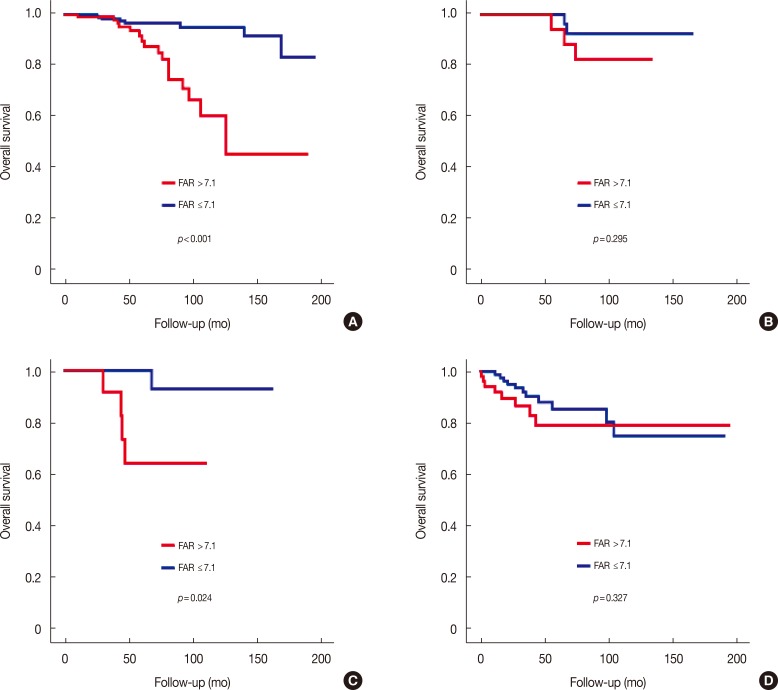
The high FAR group had a worse prognosis compared to the low FAR group (log-rank test, p<0.001). The prognostic effect of FAR was more significant than that of single markers such as fibrinogen (log-rank test, p=0.001) or albumin (log-rank test, p=0.001). The prognostic effect of FAR was prominent in the stage II/III subgroup (log-rank test, p<0.001) and luminal A-like subtype (log-rank test, p<0.001). FAR was identified as a significant independent factor on both univariate (hazard ratio [HR], 2.722; 95% confidence interval [CI], 1.659-4.468; p<0.001) and multivariate analysis (HR, 2.622; 95% CI, 1.455-4.724; p=0.001).
CONCLUSION
Preoperative FAR was a strong independent prognostic factor in breast cancer. Its prognostic effect was more prominent in the stage II/III subgroup and in the luminal A-like subtype. Therefore, preoperative FAR can be utilized as a useful prognosticator for breast cancer patients. Further studies are needed to validate its applications in clinical settings.
MeSH Terms
Figure
Reference
-
1. Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008; 454:436–444. PMID: 18650914.
Article2. Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow? Lancet. 2001; 357:539–545. PMID: 11229684.
Article3. Colotta F, Allavena P, Sica A, Garlanda C, Mantovani A. Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis. 2009; 30:1073–1081. PMID: 19468060.
Article4. Shrotriya S, Walsh D, Bennani-Baiti N, Thomas S, Lorton C. C-reactive protein is an important biomarker for prognosis tumor recurrence and treatment response in adult solid tumors: a systematic review. PLoS One. 2015; 10:e0143080. PMID: 26717416.
Article5. Gupta D, Lis CG. Pretreatment serum albumin as a predictor of cancer survival: a systematic review of the epidemiological literature. Nutr J. 2010; 9:69. PMID: 21176210.
Article6. Uribe-Querol E, Rosales C. Neutrophils in cancer: two sides of the same coin. J Immunol Res. 2015; 2015:983698. PMID: 26819959.
Article7. Menter DG, Tucker SC, Kopetz S, Sood AK, Crissman JD, Honn KV. Platelets and cancer: a casual or causal relationship: revisited. Cancer Metastasis Rev. 2014; 33:231–269. PMID: 24696047.
Article8. Liang L, Zhu J, Jia H, Huang L, Li D, Li Q, et al. Predictive value of pretreatment lymphocyte count in stage II colorectal cancer and in high-risk patients treated with adjuvant chemotherapy. Oncotarget. 2016; 7:1014–1028. PMID: 26510910.
Article9. Perisanidis C, Psyrri A, Cohen EE, Engelmann J, Heinze G, Perisanidis B, et al. Prognostic role of pretreatment plasma fibrinogen in patients with solid tumors: a systematic review and meta-analysis. Cancer Treat Rev. 2015; 41:960–970. PMID: 26604093.
Article10. McMillan DC. The systemic inflammation-based Glasgow prognostic score: a decade of experience in patients with cancer. Cancer Treat Rev. 2013; 39:534–540. PMID: 22995477.
Article11. Sun J, Chen X, Gao P, Song Y, Huang X, Yang Y, et al. Can the neutrophil to lymphocyte ratio be used to determine gastric cancer treatment outcomes? A systematic review and meta-analysis. Dis Markers. 2016; 2016:7862469. PMID: 26924872.
Article12. Templeton AJ, Ace O, McNamara MG, Al-Mubarak M, Vera-Badillo FE, Hermanns T, et al. Prognostic role of platelet to lymphocyte ratio in solid tumors: a systematic review and meta-analysis. Cancer Epidemiol Biomarkers Prev. 2014; 23:1204–1212. PMID: 24793958.
Article13. Gu L, Li H, Chen L, Ma X, Li X, Gao Y, et al. Prognostic role of lymphocyte to monocyte ratio for patients with cancer: evidence from a systematic review and meta-analysis. Oncotarget. 2016; 7:31926–31942. PMID: 26942464.
Article14. Bugada D, Allegri M, Lavand'homme P, De Kock M, Fanelli G. Inflammation-based scores: a new method for patient-targeted strategies and improved perioperative outcome in cancer patients. Biomed Res Int. 2014; 2014:142425. PMID: 24877056.
Article15. Roxburgh CS, McMillan DC. Role of systemic inflammatory response in predicting survival in patients with primary operable cancer. Future Oncol. 2010; 6:149–163. PMID: 20021215.
Article16. Wei B, Yao M, Xing C, Wang W, Yao J, Hong Y, et al. The neutrophil lymphocyte ratio is associated with breast cancer prognosis: an updated systematic review and meta-analysis. Onco Targets Ther. 2016; 9:5567–5575. PMID: 27660475.
Article17. Krenn-Pilko S, Langsenlehner U, Thurner EM, Stojakovic T, Pichler M, Gerger A, et al. The elevated preoperative platelet-to-lymphocyte ratio predicts poor prognosis in breast cancer patients. Br J Cancer. 2014; 110:2524–2530. PMID: 24675383.
Article18. Wang D, Duan L, Tu Z, Yan F, Zhang C, Li X, et al. The Glasgow prognostic score predicts response to chemotherapy in patients with metastatic breast cancer. Chemotherapy. 2016; 61:217–222. PMID: 26905743.
Article19. Mei Y, Zhao S, Lu X, Liu H, Li X, Ma R. Clinical and prognostic significance of preoperative plasma fibrinogen levels in patients with operable breast cancer. PLoS One. 2016; 11:e0146233. PMID: 26799214.
Article20. Lis CG, Grutsch JF, Vashi PG, Lammersfeld CA. Is serum albumin an independent predictor of survival in patients with breast cancer? JPEN J Parenter Enteral Nutr. 2003; 27:10–15. PMID: 12549592.
Article21. Wen J, Yang Y, Ye F, Huang X, Li S, Wang Q, et al. The preoperative plasma fibrinogen level is an independent prognostic factor for overall survival of breast cancer patients who underwent surgical treatment. Breast. 2015; 24:745–750. PMID: 26482138.
Article22. Krenn-Pilko S, Langsenlehner U, Stojakovic T, Pichler M, Gerger A, Kapp KS, et al. An elevated preoperative plasma fibrinogen level is associated with poor disease-specific and overall survival in breast cancer patients. Breast. 2015; 24:667–672. PMID: 26346586.
Article23. Liu X, Meng QH, Ye Y, Hildebrandt MA, Gu J, Wu X. Prognostic significance of pretreatment serum levels of albumin, LDH and total bilirubin in patients with non-metastatic breast cancer. Carcinogenesis. 2015; 36:243–248. PMID: 25524924.
Article24. Mohri T, Mohri Y, Shigemori T, Takeuchi K, Itoh Y, Kato T. Impact of prognostic nutritional index on long-term outcomes in patients with breast cancer. World J Surg Oncol. 2016; 14:170. PMID: 27349744.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- High Preoperative Fibrinogen and Systemic Inflammation Response Index (F-SIRI) Predict Unfavorable Survival of Resectable Gastric Cancer Patients
- Albumin-to-Fibrinogen Ratio as an Independent Prognostic Parameter in Untreated Chronic Lymphocytic Leukemia: A Retrospective Study of 191 Cases
- Clinical significance and prognostic value of C-reactive protein/albumin ratio in gastric cancer
- The Fibrinogen to Mean Platelet Volume Ratio Can Predict Overall Survival of Patients with Non-Metastatic Gastric Cancer
- In vitro inhibition of biophysical surface properties and change in ultrastructures of exogenous pulmonary surfactant by albumin or fibrinogen