J Korean Orthop Assoc.
2019 Feb;54(1):72-77. 10.4055/jkoa.2019.54.1.72.
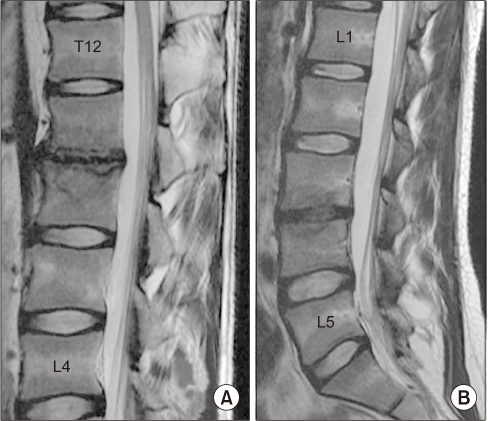
Late-Onset Candida Vertebral Osteomyelitis in Two Young Patients Who Underwent Heart Transplant Surgery
- Affiliations
-
- 1Department of Orthopedic Surgery, Seoul Red Cross Hospital, Seoul, Korea.
- 2Department of Orthopedic Surgery, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea. sthkim96@gmail.com
- KMID: 2438968
- DOI: http://doi.org/10.4055/jkoa.2019.54.1.72
Abstract
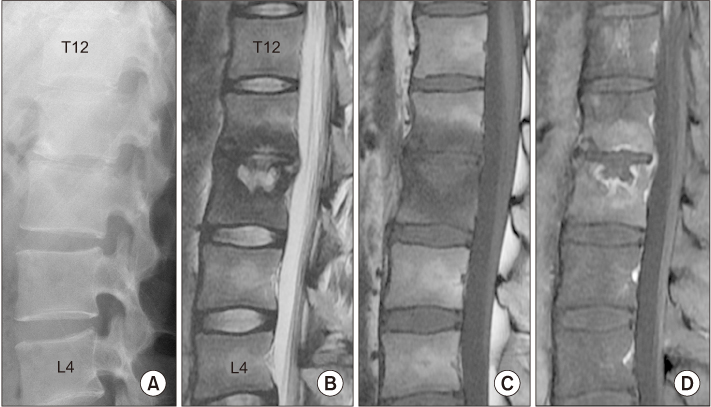
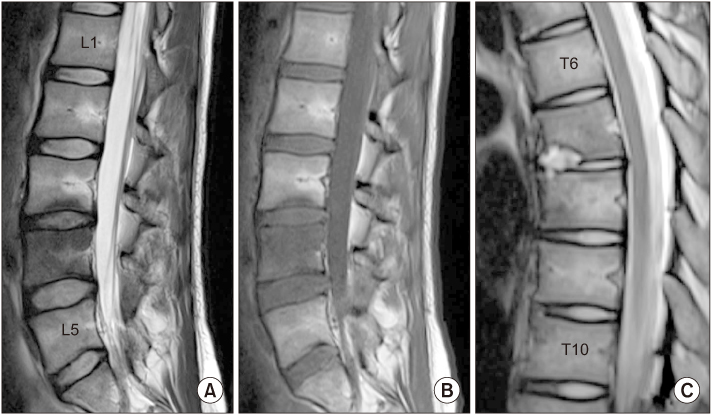
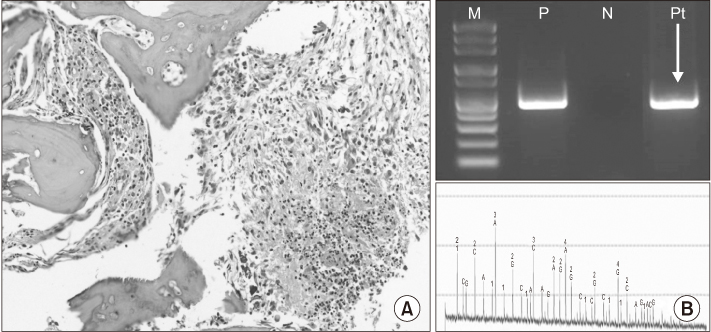
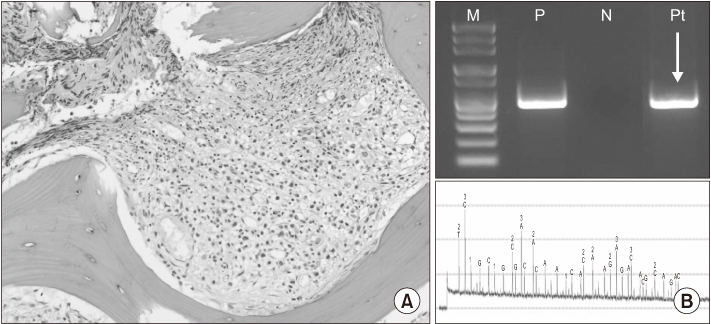
- Candida vertebral osteomyelitis (CVO) is a rare disease that is a complication of intravenous drug use, but recently it has been recognized as mostly an opportunistic infection. Because CVO appears to mimic pyogenic spondylodiscitis in terms of the clinical and radiologic presentations, it is often neglected in a usual clinical setting. The clinical, radiological, and biological characteristics of CVO are often used to make a differential diagnosis with vertebral osteomyelitis from other etiologies. Once an initial proper diagnosis was performed, the treatment relies on the prompt initiation of appropriate pharmacotherapy and serial monitoring of the clinical progress. This paper report late-onset CVO in two young patients who underwent a heart transplant surgery and had postoperative systemic candidiasis. These two cases are a good reminder of the potential of CVO in immunosuppressive patients treated with anti-fungal agents. This paper presents these two cases with a review of the relevant literature.
MeSH Terms
Figure
Reference
-
1. Frazier DD, Campbell DR, Garvey TA, Wiesel S, Bohlman HH, Eismont FJ. Fungal infections of the spine. Report of eleven patients with long-term follow-up. J Bone Joint Surg Am. 2001; 83-A:560–565.2. Edmond MB, Wallace SE, McClish DK, Pfaller MA, Jones RN, Wenzel RP. Nosocomial bloodstream infections in United States hospitals: a three-year analysis. Clin Infect Dis. 1999; 29:239–244.
Article3. Gharizadeh B, Norberg E, Löffler J, et al. Identification of medically important fungi by the pyrosequencing technology. Mycoses. 2004; 47:29–33.4. Rachapalli SM, Malaiya R, Mohd TA, Hughes RA. Successful treatment of Candida discitis with 5-flucytosine and fluconazole. Rheumatol Int. 2010; 30:1543–1544.
Article5. VandenBergh MF, Verweij PE, Voss A. Epidemiology of nosocomial fungal infections: invasive aspergillosis and the environment. Diagn Microbiol Infect Dis. 1999; 34:221–227.
Article6. Ganesh D, Gottlieb J, Chan S, Martinez O, Eismont F. Fungal infections of the spine. Spine (Phila Pa 1976). 2015; 40:E719–E728.
Article7. Miller DJ, Mejicano GC. Vertebral osteomyelitis due to Candida species: case report and literature review. Clin Infect Dis. 2001; 33:523–530.8. Dwyer K, McDonald M, Fitzpatrick T. Presentation of Candida glabrata spinal osteomyelitis 25 months after documented candidaemia. Aust N Z J Med. 1999; 29:571–572.
Article9. Golimbu C, Firooznia H, Rafii M. CT of osteomyelitis of the spine. AJR Am J Roentgenol. 1984; 142:159–163.
Article10. Williams RL, Fukui MB, Meltzer CC, Swarnkar A, Johnson DW, Welch W. Fungal spinal osteomyelitis in the immunocompromised patient: MR findings in three cases. AJNR Am J Neuroradiol. 1999; 20:381–385.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An infant with a palatal fistula secondary to Candida infection
- Treatment of Invasive Candida Osteomyelitis of the Mandible: A Case Report
- Vertebral Osteomyelitis caused by Mycobacterium abscessus in an Immunocompetent Patient
- A Case of Vertebral Osteomyelitis with Bacteremia and Psoas Abscess Caused by Non-typeable Haemophilus influenzae
- Epidural Abscess and Vertebral Osteomyelitis Induced by Epidural Injection: A case report