Ann Surg Treat Res.
2019 Mar;96(3):138-145. 10.4174/astr.2019.96.3.138.
Early experiences of endovascular aneurysm repair for ruptured abdominal aortic aneurysms
- Affiliations
-
- 1Department of Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. tslee@snubh.org
- 2Department of Surgery, The Catholic University of Korea School of Medicine, Seoul, Korea.
- KMID: 2438690
- DOI: http://doi.org/10.4174/astr.2019.96.3.138
Abstract
- PURPOSE
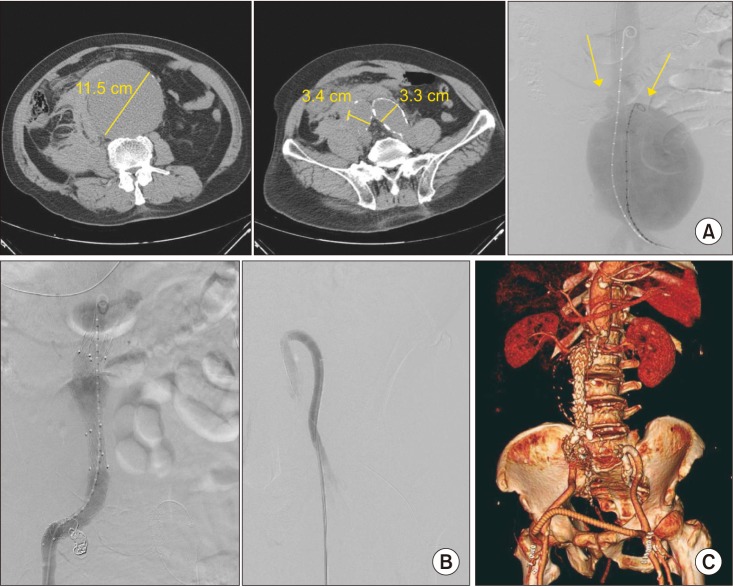
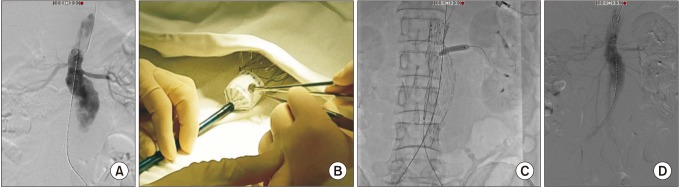
The use of endovascular aneurysm repair (EVAR) for ruptured abdominal aortic aneurysms (r-AAA) is steadily increasing. We report early experiences of EVAR for r-AAA performed in two tertiary referral centers in Korea.
METHODS
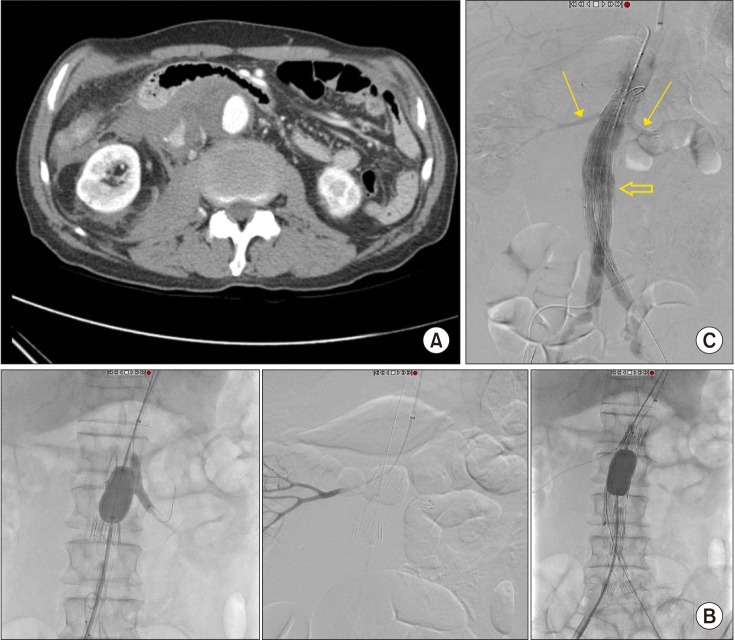
We retrospectively reviewed r-AAA patients treated by EVAR from May 2013 to December 2017. An EVAR-first strategy for r-AAA was adopted whenever feasible. The demographic information, anatomic characteristics, operative details, postoperative complications with special attention to abdominal compartment syndrome (ACS), and 30-day mortality were collected and analyzed.
RESULTS
We identified 13 patients who underwent EVAR for r-AAA. Mean age was 74.2 years and mean AAA size was 74.2 mm. Two patients underwent cardiopulmonary resuscitation at initial presentation. Bifurcated stent grafts were used in 12 out of 13 cases and physician-modified endografts with fenestrated/chimney techniques were performed in 2 cases with short neck. Successful stent graft deployment was achieved in all cases. Three patients were suspected of having ACS and 2 of them underwent laparotomy for decompression. The 30-day mortality was 7.7% (1 of 13), the only mortality being a patient that refused decompressive laparotomy for suspected ACS.
CONCLUSION
Despite the small numbers, the outcomes of EVAR for treatment of r-AAA were very promising, even in selected cases with unfavorable anatomy. These outcomes were achieved by a dedicated and well-trained team approach, and by use of high-end angiographic technology. Finally, ACS after EVAR is not uncommon, and requires a high index of suspicion as well as liberal use of decompressive surgery.
MeSH Terms
Figure
Reference
-
1. Aggarwal S, Qamar A, Sharma V, Sharma A. Abdominal aortic aneurysm: a comprehensive review. Exp Clin Cardiol. 2011; 16:11–15. PMID: 21523201.2. Harris LM, Faggioli GL, Fiedler R, Curl GR, Ricotta JJ. Ruptured abdominal aortic aneurysms: factors affecting mortality rates. J Vasc Surg. 1991; 14:812–818. PMID: 1960812.
Article3. Reimerink JJ, Hoornweg LL, Vahl AC, Wisselink W, van den Broek TA, Legemate DA, et al. Endovascular repair versus open repair of ruptured abdominal aortic aneurysms: a multicenter randomized controlled trial. Ann Surg. 2013; 258:248–256. PMID: 23549424.
Article4. Desgranges P, Kobeiter H, Katsahian S, Bouffi M, Gouny P, Favre JP, et al. Editor’s Choice - ECAR (Endovasculaire ou Chirurgie dans les Anevrysmes aortoiliaques Rompus): a french randomized controlled trial of endovascular versus open surgical repair of ruptured aortoiliac aneurysms. Eur J Vasc Endovasc Surg. 2015; 50:303–310. PMID: 26001320.5. IMPROVE Trial Investigators. Powell JT, Sweeting MJ, Thompson MM, Ashleigh R, Bell R, et al. Endovascular or open repair strategy for ruptured abdominal aortic aneurysm: 30 day outcomes from IMPROVE randomised trial. BMJ. 2014; 348:f7661. PMID: 24418950.
Article6. Sweeting MJ, Balm R, Desgranges P, Ulug P, Powell JT. Ruptured Aneurysm Trialists. Individual-patient meta-analysis of three randomized trials comparing endovascular versus open repair for ruptured abdominal aortic aneurysm. Br J Surg. 2015; 102:1229–1239. PMID: 26104471.
Article7. IMPROVE Trial Investigators. Comparative clinical effectiveness and cost effectiveness of endovascular strategy v open repair for ruptured abdominal aortic aneurysm: three year results of the IMPROVE randomised trial. BMJ. 2017; 359:j4859. PMID: 29138135.8. Mureebe L, Egorova N, Giacovelli JK, Gelijns A, Kent KC, McKinsey JF. National trends in the repair of ruptured abdominal aortic aneurysms. J Vasc Surg. 2008; 48:1101–1107. PMID: 18771883.
Article9. Lesperance K, Andersen C, Singh N, Starnes B, Martin MJ. Expanding use of emergency endovascular repair for ruptured abdominal aortic aneurysms: disparities in outcomes from a nationwide perspective. J Vasc Surg. 2008; 47:1165–1170. discussion 1170-1. PMID: 18394857.
Article10. Kirkpatrick AW, Roberts DJ, De Waele J, Jaeschke R, Malbrain ML, De Keulenaer B, et al. Intra-abdominal hypertension and the abdominal compartment syndrome: updated consensus definitions and clinical practice guidelines from the World Society of the Abdominal Compartment Syndrome. Intensive Care Med. 2013; 39:1190–1206. PMID: 23673399.
Article11. Badger SA, Harkin DW, Blair PH, Ellis PK, Kee F, Forster R. Endovascular repair or open repair for ruptured abdominal aortic aneurysm: a Cochrane systematic review. BMJ Open. 2016; 6:e008391.
Article12. IMPROVE Trial Investigators. Endovascular strategy or open repair for ruptured abdominal aortic aneurysm: one-year outcomes from the IMPROVE randomized trial. Eur Heart J. 2015; 36:2061–2069. PMID: 25855369.13. Karkos CD, Menexes GC, Patelis N, Kalogirou TE, Giagtzidis IT, Harkin DW. A systematic review and meta-analysis of abdominal compartment syndrome after endovascular repair of ruptured abdominal aortic aneurysms. J Vasc Surg. 2014; 59:829–842. PMID: 24439324.
Article14. Acosta S, Lindblad B, Zdanowski Z. Predictors for outcome after open and endovascular repair of ruptured abdominal aortic aneurysms. Eur J Vasc Endovasc Surg. 2007; 33:277–284. PMID: 17097899.
Article15. Rubenstein C, Bietz G, Davenport DL, Winkler M, Endean ED. Abdominal compartment syndrome associated with endovascular and open repair of ruptured abdominal aortic aneurysms. J Vasc Surg. 2015; 61:648–654. PMID: 25499708.
Article16. Chen X, Zhao J, Huang B, Yuan D, Yang Y, Ma Y. Abdominal compartment syndrome after endovascular repair for ruptured abdominal aortic aneurysm leads to acute intestinal necrosis: Case report. Medicine (Baltimore). 2016; 95:e5316. PMID: 27893667.17. Powell JT, Sweeting MJ, Ulug P, Thompson MM, Hinchliffe RJ. IMPROVE Trial Investigators. Editor’s choice - re-interventions after repair of ruptured abdominal aortic aneurysm: a report from the IMPROVE randomised trial. Eur J Vasc Endovasc Surg. 2018; 55:625–632. PMID: 29503083.
Article18. Quinn AA, Mehta M, Teymouri MJ, Keenan ME, Paty PSK, Zhou Y, et al. The incidence and fate of endoleaks vary between ruptured and elective endovascular abdominal aortic aneurysm repair. J Vasc Surg. 2017; 65:1617–1624. PMID: 28268109.
Article19. Wong LA, Milner R. Interhospital Transfer of Ruptured AAA’s for EVAR: preposterous or prudent? Vasc Endovascular Surg. 2016; 50:455–457. PMID: 27488418.20. Mehta M, Taggert J, Darling RC 3rd, Chang BB, Kreienberg PB, Paty PS, et al. Establishing a protocol for endovascular treatment of ruptured abdominal aortic aneurysms: outcomes of a prospective analysis. J Vasc Surg. 2006; 44:1–8. discussion 8. PMID: 16828417.
Article21. Moore R, Nutley M, Cina CS, Motamedi M, Faris P, Abuznadah W. Improved survival after introduction of an emergency endovascular therapy protocol for ruptured abdominal aortic aneurysms. J Vasc Surg. 2007; 45:443–450. PMID: 17257800.
Article22. Budtz-Lilly J, Bjorck M, Venermo M, Debus S, Behrendt CA, Altreuther M, et al. Editor’s choice - the impact of centralisation and endovascular aneurysm repair on treatment of ruptured abdominal aortic aneurysms based on international registries. Eur J Vasc Endovasc Surg. 2018; 56:181–188. PMID: 29482972.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Complications and Their Management after Endovascular Aneurysm Repair for the Treatment of Abdominal Aortic Aneurysms
- General Considerations of Ruptured Abdominal Aortic Aneurysm: Ruptured Abdominal Aortic Aneurysm
- Endovascular Treatment of Abdominal Aortic Aneurysm
- Ruptured Abdominal Aortic Aneurysm with Antecedent Endovascular Repair of Abdominal Aortic Aneurysm
- Simultaneous Endovascular Aneurysm Repair for Abdominal Aortic Aneurysm Combined with Saccular Thoracic Aortic Aneurysm