Korean J Radiol.
2019 Mar;20(3):498-504. 10.3348/kjr.2018.0508.
Quantitative Analysis of Parotid Gland Secretion Function in Sjögren's Syndrome Patients with Dynamic Magnetic Resonance Sialography
- Affiliations
-
- 1Department of Radiology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China. panchu@21cn.com
- 2Department of Rheumatology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China.
- KMID: 2438280
- DOI: http://doi.org/10.3348/kjr.2018.0508
Abstract
OBJECTIVE
To evaluate the secretory function of parotid glands by dynamic magnetic resonance (MR) sialography and determine the clinical performance of this technique in diagnosing and evaluating Sjögren's syndrome (SS) patients.
MATERIALS AND METHODS
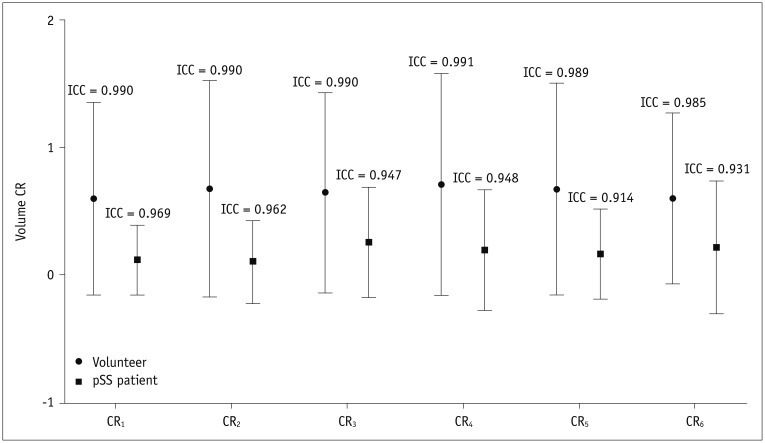
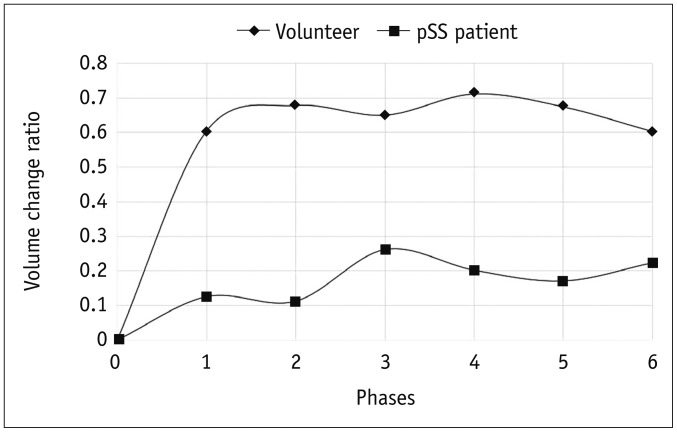
This study enrolled 29 healthy volunteers (25 women and 4 men; mean age, 34.8 ± 6.3 years; age range, 26-47 years) and 25 primary SS (pSS) patients (23 women and 2 men; mean age, 37.7 ± 7.9 years; age range, 25-50 years) with decreased secretory function. The volume of the parotid gland ducts was precisely measured for both groups at single pre- and 6 post-gustatory-stimulated phases. Time-dependent volume change ratio curves were generated, four parameters were derived from the curves: the slope of the increase in the first post-stimulation phase (slope(1st)), the peak value, the time-to-peak, the total saliva secretion post-stimulation. All values were used to quantitatively evaluate the secretory function of the parotid gland. The repeated measurement analysis, Mann-Whitney U test and receiver operating characteristic curve were applied.
RESULTS
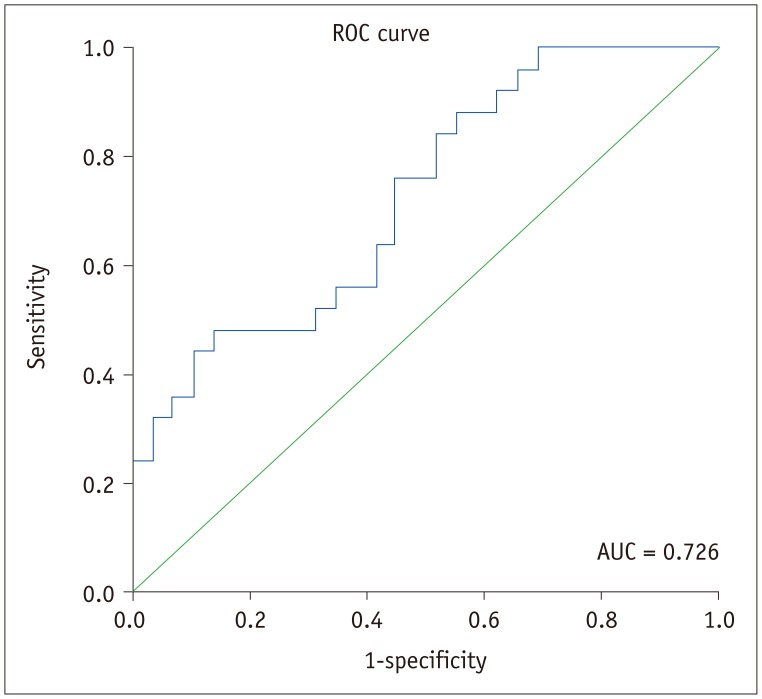
Time-dependent volume change ratio curves demonstrated that there is a statistically significant difference between the two groups (F = 8.750; p = 0.005). A quickly increasing curve was shown in the volunteer group, whereas a slowly increasing curve was shown in the pSS patient group. The slope(1st), peak value and total saliva secretion post-stimulation of the patient group were significantly lower than those of the volunteer group (p = 0.005, p = 0.003, and p = 0.002, respectively). The time-to-peak between the two groups was not significantly different (p = 0.383). The slope(1st) can be used as a discriminator to diagnose SS patients (p = 0.015; odds ratio = 4.234; area under the curve = 0.726).
CONCLUSION
Dynamic MR sialography is proven to be an effective method in evaluating salivary gland function and has a great potential in diagnosing and evaluating pSS patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Vitali C, Bombardieri S, Jonsson R, Moutsopoulos HM, Alexander EL, Carsons SE, et al. European Study Group on Classification Criteria for Sjögren's Syndrome. Classification criteria for Sjögren's syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. Ann Rheum Dis. 2002; 61:554–558. PMID: 12006334.2. Proctor GB, Carpenter GH. Regulation of salivary gland function by autonomic nerves. Auton Neurosci. 2007; 133:3–18. PMID: 17157080.
Article3. Morimoto Y, Habu M, Tomoyose T, Ono K, Tanaka T, Yoshioka I, et al. Dynamic magnetic resonance sialography as a new diagnostic technique for patients with Sjögren's syndrome. Oral Dis. 2006; 12:408–414. PMID: 16792727.4. Morimoto Y, Ono K, Tanaka T, Kito S, Inoue H, Shinohara Y, et al. The functional evaluation of salivary glands using dynamic MR sialography following citric acid stimulation: a preliminary study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005; 100:357–364. PMID: 16122666.
Article5. Morimoto Y, Tanaka T, Kito S, Tominaga K, Yoshioka I, Yamashita Y, et al. Utility of three dimension fast asymmetric spin-echo (3D-FASE) sequences in MR sialographic sequences: model and volunteer studies. Oral Dis. 2005; 11:35–43.
Article6. Arizono S, Isoda H, Maetani YS, Hirokawa Y, Shimada K, Nakamoto Y, et al. High-spatial-resolution three-dimensional MR cholangiography using a high-sampling-efficiency technique (SPACE) at 3T: comparison with the conventional constant flip angle sequence in healthy volunteers. J Magn Reson Imaging. 2008; 28:685–690. PMID: 18777552.
Article7. Ucar M, Tokgoz N, Damar C, Alimli AG, Oncu F. Diagnostic performance of heavily T2-weighted techniques in obstructive hydrocephalus: comparison study of two different 3D heavily T2-weighted and conventional T2-weighted sequences. Jpn J Radiol. 2015; 33:94–101. PMID: 25559932.
Article8. Ahmed NS, Mansour SM, El-Wakd MM, Al-Azizi HM, Abu-Taleb NS. The value of magnetic resonance sialography and magnetic resonance imaging versus conventional sialography of the parotid gland in the diagnosis and staging of Sjögren's syndrome. The Egyptian Rheumatologist. 2011; 33:147–154.
Article9. Jäger L, Menauer F, Holzknecht N, Scholz V, Grevers G, Reiser M. Sialolithiasis: MR sialography of the submandibular duct--an alternative to conventional sialography and US? Radiology. 2000; 216:665–671. PMID: 10966693.
Article10. Proctor GB. The physiology of salivary secretion. Periodontol 2000. 2016; 70:11–25. PMID: 26662479.
Article11. Nakaura T, Kidoh M, Maruyama N, Kawahara T, Namimoto T, Sakai Y, et al. Usefulness of the SPACE pulse sequence at 1.5T MR cholangiography: comparison of image quality and image acquisition time with conventional 3D-TSE sequence. J Magn Reson Imaging. 2013; 38:1014–1019. PMID: 24105679.
Article12. Sudholt P, Zaehringer C, Urigo C, Tyndall A, Bongartz G, Hohmann J. Comparison of optimized 3D-SPACE and 3D-TSE sequences at 1.5T MRCP in the diagnosis of choledocholithiasis. Rofo. 2015; 187:467–471. PMID: 25877993.
Article13. Tanaka T, Ono K, Ansai T, Yoshioka I, Habu M, Tomoyose T, et al. Dynamic magnetic resonance sialography for patients with xerostomia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 106:115–123. PMID: 18504153.
Article14. Richards TM, Hurley T, Grove L, Harrington KJ, Carpenter GH, Proctor GB, et al. The effect of parotid gland-sparing intensity-modulated radiotherapy on salivary composition, flow rate and xerostomia measures. Oral Dis. 2017; 23:990–1000. PMID: 28434191.
Article15. Roberts C, Parker GJ, Rose CJ, Watson Y, O'Connor JP, Stivaros SM, et al. Glandular function in Sjögren syndrome: assessment with dynamic contrast-enhanced MR imaging and tracer kinetic modeling--initial experience. Radiology. 2008; 246:845–853. PMID: 18235107.
Article16. Shiboski CH, Shiboski SC, Seror R, Criswell LA, Labetoulle M, Lietman TM, et al. International Sjögren's Syndrome Criteria Working Group. 2016 American College of Rheumatology/European League Against Rheumatism classification criteria for primary Sjögren's syndrome: a consensus and data-driven methodology involving three international patient cohorts. Arthritis Rheumatol. 2017; 69:35–45. PMID: 27785888.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Motor dominant polyradiculopathy with Primary Sjögren's syndrome mimicking motor neuron disease
- A Case of Treatment with Steroid and Hydrochloroquine of Thrombocytopenia in Primary Sjögren's Syndrome
- Sialography And Salivary Scan Study Of Salivary Diseases
- A Case of Sjögren-Larsson Syndrome
- Longitudinal Changes of the European League Against Rheumatism Sjögren's Syndrome Patient Reported Index in Korean Patients with Primary Sjögren's Syndrome