Korean J Radiol.
2019 Mar;20(3):422-428. 10.3348/kjr.2018.0270.
Computed Tomography Arteriography for Detecting the Origin of the Inferior Pyloric Artery in Patients with Gastric Cancer
- Affiliations
-
- 1Department of Radiology, Peking University Cancer Hospital & Institute, Beijing, China; Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education), Beijing, China.
- 2Department of Gastrointestinal Surgery, Peking University Cancer Hospital & Institute, Beijing, China; Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education), Beijing, China. jijiafu@hsc.pku.edu.cn
- KMID: 2438272
- DOI: http://doi.org/10.3348/kjr.2018.0270
Abstract
OBJECTIVE
To analyze the detection rate of the inferior pyloric artery (IPA) in patients with gastric cancer by computed tomography arteriography (CTA).
MATERIALS AND METHODS
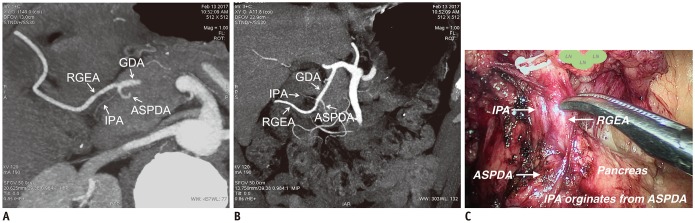
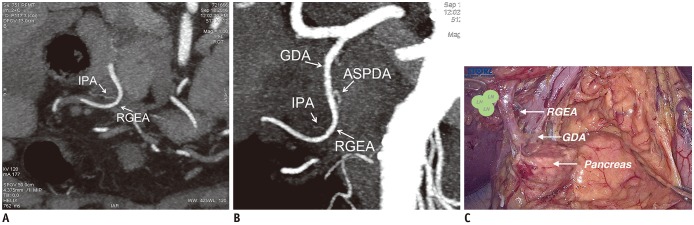
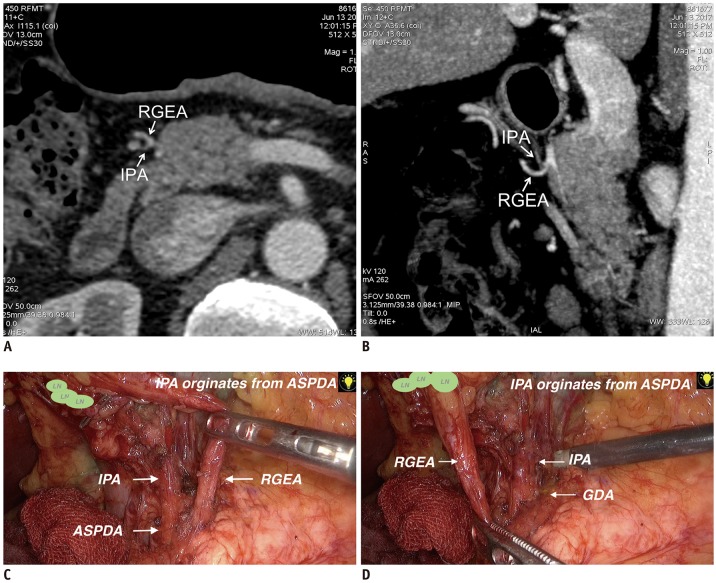
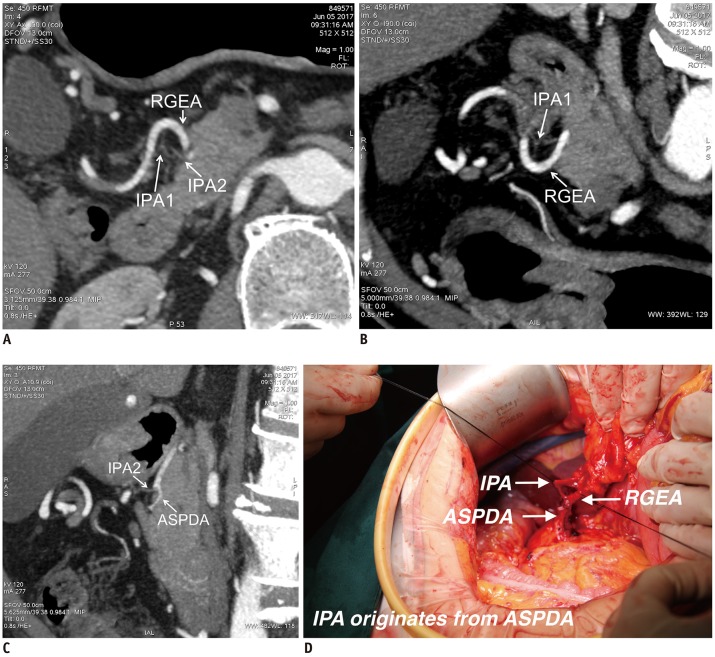
Fifty-four patients (48 males and 6 females; mean age, 59.0 ± 1.5 years) who had undergone radical gastrectomy for gastric cancer from September 2016 to July 2017 at our institution were recruited prospectively. Patients underwent abdominal contrast-enhanced CT scans and CTA imaging reconstruction before the operation. The origin of the IPA in all cases was determined by a radiologist based on CTA images and verified by the surgeon. The accuracy of CTA in diagnosing the origin of the IPA was calculated. Dominant vessels of the origin were analyzed.
RESULTS
IPAs were detected by CTA in 51 patients (94.4%). Among these, IPAs originated from the right gastroepiploic artery (RGEA) (24 cases), the gastroduodenal artery (GDA) (4 cases), and the anterior superior pancreaticoduodenal artery (ASPDA) (20 cases). In the remaining 3 cases, the IPAs contained two branches originating from the RGEA and ASPDA, respectively. During surgery, in 2 (3.7%) of the 54 cases of gastric cancer, IPAs could not be detected; the IPAs originated from the RGEA (22 cases), GDA (5 cases), and ASPDA (24 cases). One case had an IPA originating from both the RGEA and the GDA. Finally, the accuracy of CTA in diagnosing the origin artery of the IPA was 85.2% (46/54).
CONCLUSION
CTA can detect the origin of the IPA accurately, which can aid surgeons while performing pylorus-preserving operations.
MeSH Terms
Figure
Reference
-
1. Mizuno A, Shinohara H, Haruta S, Tsunoda S, Kurahashi Y, Ohkura Y, et al. Lymphadenectomy along the infrapyloric artery may be dispensable when performing pylorus-preserving gastrectomy for early middle-third gastric cancer. Gastric Cancer. 2017; 20:543–547. PMID: 27516348.
Article2. Shibata C, Saijo F, Kakyo M, Kinouchi M, Tanaka N, Sasaki I, et al. Society for the Study of Postoperative Morbidity After Gastrectomy. Current status of pylorus-preserving gastrectomy for the treatment of gastric cancer: a questionnaire survey and review of literatures. World J Surg. 2012; 36:858–863. PMID: 22350486.
Article3. Hiki N, Kaminishi M. Pylorus-preserving gastrectomy in gastric cancer surgery--open and laparoscopic approaches. Langenbecks Arch Surg. 2005; 390:442–447. PMID: 16096761.
Article4. Iino I, Sakaguchi T, Kikuchi H, Miyazaki S, Fujita T, Hiramatsu Y, et al. Usefulness of three-dimensional angiographic analysis of perigastric vessels before laparoscopic gastrectomy. Gastric Cancer. 2013; 16:355–361. PMID: 22965813.
Article5. Kumano S, Tsuda T, Tanaka H, Hirata M, Kim T, Murakami T, et al. Preoperative evaluation of perigastric vascular anatomy by 3-dimensional computed tomographic angiography using 16-channel multidetector-row computed tomography for laparoscopic gastrectomy in patients with early gastric cancer. J Comput Assist Tomogr. 2007; 31:93–97. PMID: 17259839.
Article6. Miyaki A, Imamura K, Kobayashi R, Takami M, Matsumoto J, Takada Y. Preoperative assessment of perigastric vascular anatomy by multidetector computed tomography angiogram for laparoscopy-assisted gastrectomy. Langenbecks Arch Surg. 2012; 397:945–950. PMID: 22562645.
Article7. Shinohara H, Kurahashi Y, Kanaya S, Haruta S, Ueno M, Udagawa H, et al. Topographic anatomy and laparoscopic technique for dissection of no. 6 infrapyloric lymph nodes in gastric cancer surgery. Gastric Cancer. 2013; 16:615–620. PMID: 23314832.
Article8. Rossi G, Cova E. Studio morfolgico delle arterie dello stomaco. Arch Ital Anat Embriol. 1904; 3:485–657.9. Kuroda C, Nakamura H, Sato T, Yoshioka H, Tokunaga K, Hori S, et al. Normal anatomy of the pyloric branch and its diagnostic significance in angiography. Acta Radiol Diagn (Stockh). 1982; 23:479–484. PMID: 7158412.
Article10. Vandamme JP, Bonte J. The blood supply of the stomach. Acta Anat (Basel). 1988; 131:89–96. PMID: 3369288.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- 18F-2-Deoxy-2-Fluoro-D-Glucose Positron Emission Tomography: Computed Tomography for Preoperative Staging in Gastric Cancer Patients
- A Rare Case in the Pattern of the Origin of the Celiac Artery
- Comparison of 18F-Fluorodeoxyglucose Positron Emission Tomography/Computed Tomography, Hydro-Stomach Computed Tomography, and Their Combination for Detecting Primary Gastric Cancer
- Prevalence and clinical relevance of the anatomical variations of suprarenal arteries: a review
- Variant Origin of Obturator Artery: A Branch of Inferior Epigastric Artery from External Iliac Artery