Korean J Radiol.
2019 Mar;20(3):378-384. 10.3348/kjr.2018.0248.
Diagnostic Performance of MRI for Assessing Parametrial Invasion in Cervical Cancer: A Head-to-Head Comparison between Oblique and True Axial T2-Weighted Images
- Affiliations
-
- 1Department of Radiology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. iwishluv@empas.com
- 2Department of Radiology, Seoul Metropolitan Government, Seoul National University Boramae Medical Center, Seoul, Korea.
- 3Institute of Radiation Medicine and Kidney Research Institute, Seoul National University Medical Research Center, Seoul, Korea.
- KMID: 2438267
- DOI: http://doi.org/10.3348/kjr.2018.0248
Abstract
OBJECTIVE
To directly compare the diagnostic performance of true and oblique axial T2-weighted imaging (T2WI) for assessing parametrial invasion (PMI) in cervical cancer.
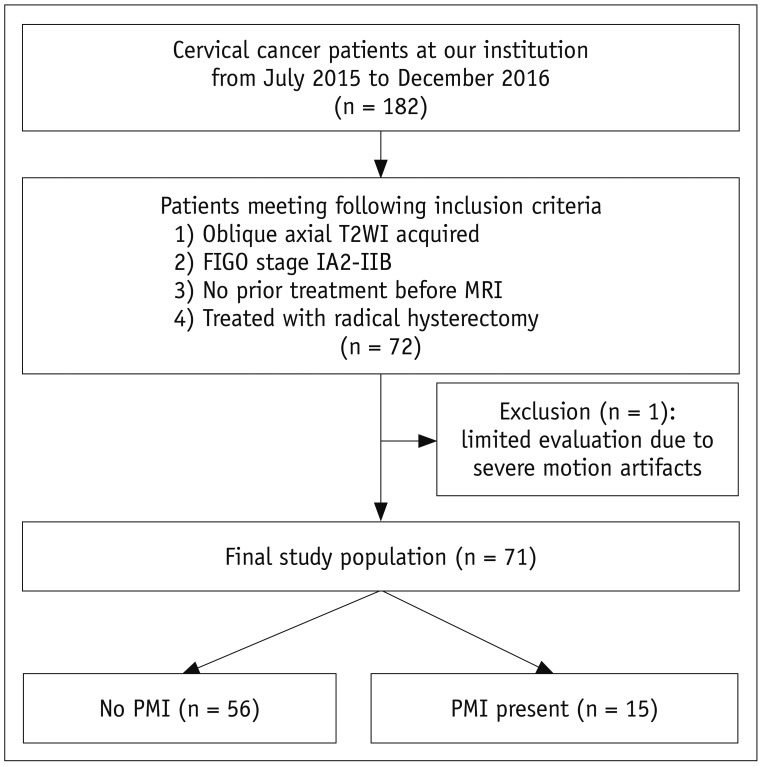
MATERIALS AND METHODS
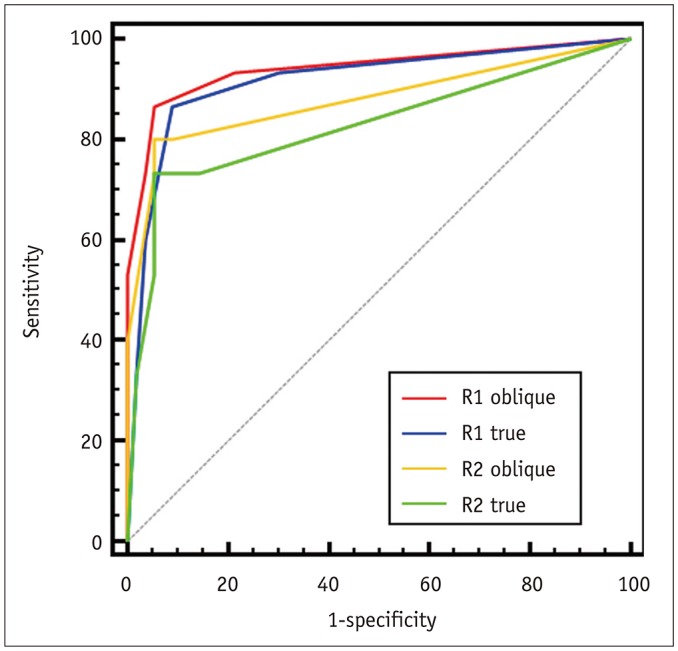
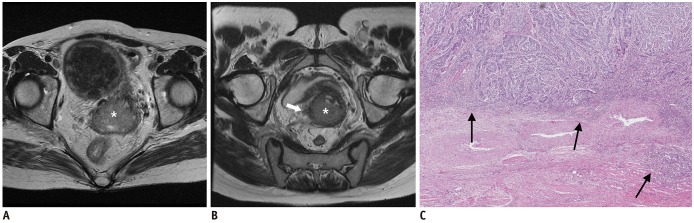
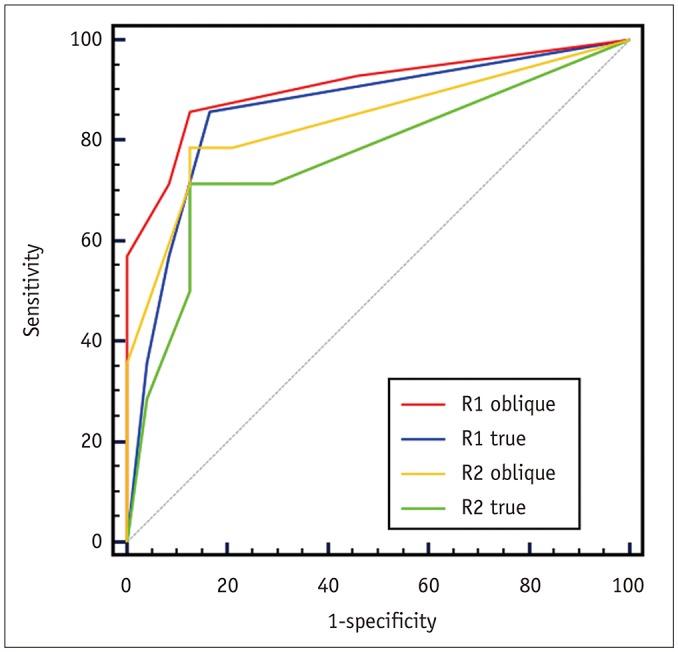
This retrospective study included 71 women with treatment-naive cervical cancer who underwent MRI that included both oblique and true axial T2WI, followed by radical hysterectomy. Two blinded radiologists (Radiologist 1 and Radiologist 2) independently assessed the presence of PMI on both sequences using a 5-point Likert scale. Receiver operating characteristic (ROC) curve analysis was performed, with a subgroup analysis for tumors sized > 2.5 cm and ≤ 2.5 cm in diameter. Inter-reader agreement was assessed with kappa (k) statistics.
RESULTS
At hysterectomy, 15 patients (21.1%) had PMI. For Radiologist 1, the area under the ROC curve (AUC) was greater for oblique axial than for true axial T2WI {0.941 (95% confidence interval [CI] = 0.858-0.983) vs. 0.917 (95% CI = 0.827-0.969), p = 0.027}. The difference was not significant for Radiologist 2 (0.879 [95% CI = 0.779-0.944] vs. 0.827 [95% CI = 0.719-0.906], p = 0.153). For tumors > 2.5 cm, AUC was greater with oblique than with true axial T2WI (0.906 vs. 0.860, p = 0.046 for Radiologist 1 and 0.839 vs. 0.765, p = 0.086 for Radiologist 2). Agreement between the radiologists was almost perfect for oblique axial T2WI (k = 0.810) and was substantial for true axial T2WI (k = 0.704).
CONCLUSION
Oblique axial T2WI potentially provides greater diagnostic performance than true axial T2WI for determining PMI, particularly for tumors > 2.5 cm. The inter-reader agreement was greater with oblique axial T2WI.
MeSH Terms
Figure
Reference
-
1. Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012; 62:10–29. PMID: 22237781.
Article2. Landoni F, Bocciolone L, Perego P, Maneo A, Bratina G, Mangioni C. Cancer of the cervix, FIGO stages IB and IIA: patterns of local growth and paracervical extension. Int J Gynecol Cancer. 1995; 5:329–334. PMID: 11578499.
Article3. Peters WA 3rd, Liu PY, Barrett RJ 2nd, Stock RJ, Monk BJ, Berek JS, et al. Concurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high-risk early-stage cancer of the cervix. J Clin Oncol. 2000; 18:1606–1613. PMID: 10764420.
Article4. Pecorelli S, Benedet JL, Creasman WT, Shepherd JH. FIGO staging of gynecologic cancer. 1994-1997 FIGO Committee on Gynecologic Oncology. International Federation of Gynecology and Obstetrics. Int J Gynaecol Obstet. 1999; 65:243–249. PMID: 10428343.5. Thomeer MG, Gerestein C, Spronk S, van Doorn HC, van der Ham E, Hunink MG. Clinical examination versus magnetic resonance imaging in the pretreatment staging of cervical carcinoma: systematic review and meta-analysis. Eur Radiol. 2013; 23:2005–2018. PMID: 23455762.
Article6. Woo S, Suh CH, Kim SY, Cho JY, Kim SH. Magnetic resonance imaging for detection of parametrial invasion in cervical cancer: an updated systematic review and meta-analysis of the literature between 2012 and 2016. Eur Radiol. 2018; 28:530–541. PMID: 28726120.
Article7. Balleyguier C, Sala E, Da Cunha T, Bergman A, Brkljacic B, Danza F, et al. Staging of uterine cervical cancer with MRI: guidelines of the European Society of Urogenital Radiology. Eur Radiol. 2011; 21:1102–1110. PMID: 21063710.
Article8. Sala E, Rockall AG, Freeman SJ, Mitchell DG, Reinhold C. The added role of MR imaging in treatment stratification of patients with gynecologic malignancies: what the radiologist needs to know. Radiology. 2013; 266:717–740. PMID: 23431227.
Article9. Sala E, Wakely S, Senior E, Lomas D. MRI of malignant neoplasms of the uterine corpus and cervix. AJR Am J Roentgenol. 2007; 188:1577–1587. PMID: 17515380.
Article10. Rauch GM, Kaur H, Choi H, Ernst RD, Klopp AH, Boonsirikamchai P, et al. Optimization of MR imaging for pretreatment evaluation of patients with endometrial and cervical cancer. Radiographics. 2014; 34:1082–1098. PMID: 25019443.
Article11. Park JJ, Kim CK, Park SY, Park BK, Kim B. Value of diffusion-weighted imaging in predicting parametrial invasion in stage IA2-IIA cervical cancer. Eur Radiol. 2014; 24:1081–1088. PMID: 24522622.
Article12. Sala E, Micco M, Burger IA, Yakar D, Kollmeier MA, Goldman DA, et al. Complementary prognostic value of pelvic magnetic resonance imaging and whole-body fluorodeoxyglucose positron emission tomography/computed tomography in the pretreatment assessment of patients with cervical cancer. Int J Gynecol Cancer. 2015; 25:1461–1467. PMID: 26397068.
Article13. Das M, Mühlenbruch G, Mahnken AH, Flohr TG, Gündel L, Stanzel S, et al. Small pulmonary nodules: effect of two computer-aided detection systems on radiologist performance. Radiology. 2006; 241:564–571. PMID: 17057074.
Article14. Lee JY, Youm J, Kim TH, Cho JY, Kim MA, Suh DH, et al. Preoperative MRI criteria for trials on less radical surgery in stage IB1 cervical cancer. Gynecol Oncol. 2014; 134:47–51. PMID: 24768849.
Article15. McCarville MB, Kaste SC, Hoffer FA, Khan RB, Walton RC, Alpert BS, et al. Contrast-enhanced sonography of malignant pediatric abdominal and pelvic solid tumors: preliminary safety and feasibility data. Pediatr Radiol. 2012; 42:824–833. PMID: 22249601.
Article16. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–174. PMID: 843571.
Article17. Shiraiwa M, Joja I, Asakawa T, Okuno K, Shibutani O, Akamatsu N, et al. Cervical carcinoma: efficacy of thin-section oblique axial T2-weighted images for evaluating parametrial invasion. Abdom Imaging. 1999; 24:514–519. PMID: 10475940.
Article18. Lee JY, Youm J, Kim JW, Cho JY, Kim MA, Kim TH, et al. Identifying a low-risk group for parametrial involvement in microscopic stage IB1 cervical cancer using criteria from ongoing studies and a new MRI criterion. BMC Cancer. 2015; 15:167. PMID: 25885786.
Article19. Kong TW, Piao X, Chang SJ, Paek J, Lee Y, Lee EJ, et al. A predictive model for parametrial invasion in patients with FIGO stage IB cervical cancer: individualized approach for primary treatment. Int J Gynecol Cancer. 2016; 26:184–191. PMID: 26512782.
Article20. Kamimori T, Sakamoto K, Fujiwara K, Umayahara K, Sugiyama Y, Utsugi K, et al. Parametrial involvement in FIGO stage IB1 cervical carcinoma diagnostic impact of tumor diameter in preoperative magnetic resonance imaging. Int J Gynecol Cancer. 2011; 21:349–354. PMID: 21721193.
Article21. Fridsten S, Hellström AC, Hellman K, Sundin A, Söderén B, Blomqvist L. Preoperative MR staging of cervical carcinoma: are oblique and contrast-enhanced sequences necessary? Acta Radiol Open. 2016; 5:2058460116679460. PMID: 27900204.
Article22. Woo S, Kim SY, Cho JY, Kim SH. Assessment of deep myometrial invasion of endometrial cancer on MRI: added value of second-opinion interpretations by radiologists subspecialized in gynaecologic oncology. Eur Radiol. 2017; 27:1877–1882. PMID: 27655304.
Article23. Lakhman Y, D'Anastasi M, Miccò M, Scelzo C, Vargas HA, Nougaret S, et al. Second-opinion interpretations of gynecologic oncologic MRI examinations by sub-specialized radiologists influence patient care. Eur Radiol. 2016; 26:2089–2098. PMID: 26494640.
Article24. Hori M, Kim T, Murakami T, Imaoka I, Onishi H, Tomoda K, et al. Uterine cervical carcinoma: preoperative staging with 3.0-T MR imaging--comparison with 1.5-T MR imaging. Radiology. 2009; 251:96–104. PMID: 19221059.
Article25. Park HJ, Lee SY, Choi SH, Ahn JH, Park SJ, Park JH, et al. Comparison of oblique coronal images in knee of three-dimensional isotropic T2-weighted turbo spin echo MRI versus two-dimensional fast spin echo T2-weighted sequences for evaluation of posterior cruciate ligament injury. Br J Radiol. 2016; 89:20160554. PMID: 27653673.26. Shin YR, Rha SE, Choi BG, Oh SN, Park MY, Byun JY. Uterine cervical carcinoma: a comparison of two- and three-dimensional T2-weighted turbo spin-echo MR imaging at 3.0 T for image quality and local-regional staging. Eur Radiol. 2013; 23:1150–1157. PMID: 22868482.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- MR Imaging of Cervical Carcinomas : Comparison between Body Coil, Endorectal Surface Coil and Dynamic Enhanced Images on the Aspect of Parametrial and Vaginal Invasion
- The Usefulness of Dynamic MR Imaging for the Evaluation of Cervical Cancer
- Avascular Necrosis of Femoral Head: Findings of Contrast-Enhanced MR Imaging
- Carcinoma of the Cervix: Usefulness of Dynamic and Contrast-Enhanced T1-weighted MR Imaging in Assessing theDepth of Stromal Invasion
- MR Imaging findings of Diffuse Axonal Injury: Comparison of T2*-weighted Gradient Images and T1- andT2-weighted Spin-Echo Images