Korean J Radiol.
2019 Feb;20(2):313-322. 10.3348/kjr.2017.0779.
Computed Tomography Pulmonary Angiography during Pregnancy: Radiation Dose of Commonly Used Protocols and the Effect of Scan Length Optimization
- Affiliations
-
- 1Department of Radiology & Nuclear Medicine, Maastricht University Medical Centre, Maastricht, The Netherlands. babs.hendriks@mumc.nl
- 2CARIM School for Cardiovascular Diseases, Maastricht University Medical Centre, Maastricht, The Netherlands.
- 3Department of Surgical Sciences, Division of Radiology, University of Parma, Parma, Italy.
- 4Department of Diagnostic and Interventional Radiology, Duisburg, Germany.
- KMID: 2438262
- DOI: http://doi.org/10.3348/kjr.2017.0779
Abstract
OBJECTIVE
To evaluate the radiation dose for pregnant women and fetuses undergoing commonly used computed tomography of the pulmonary arteries (CTPA) scan protocols and subsequently evaluate the simulated effect of an optimized scan length.
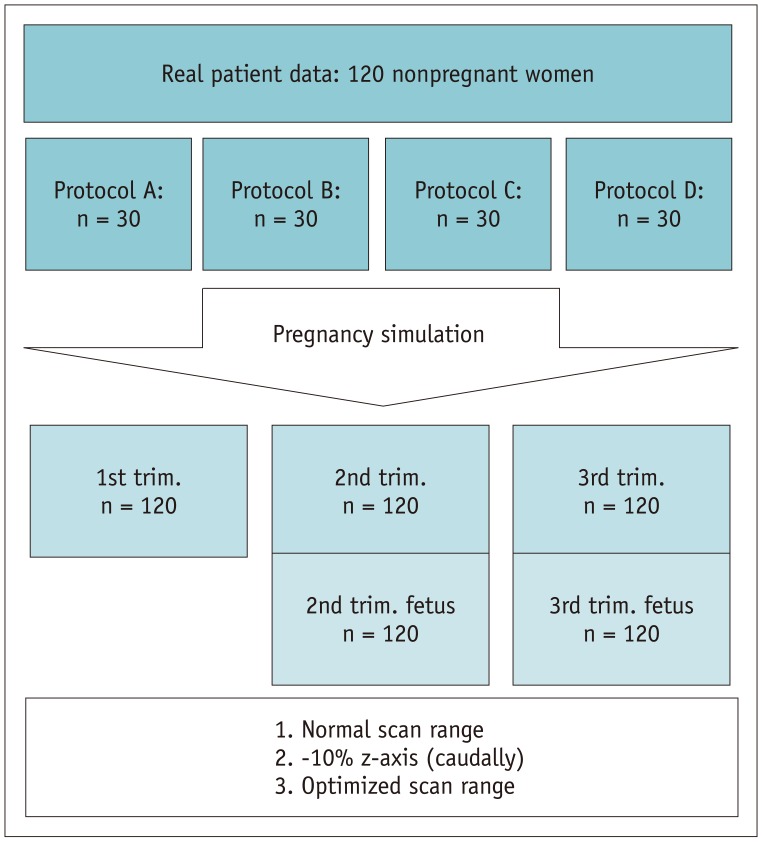
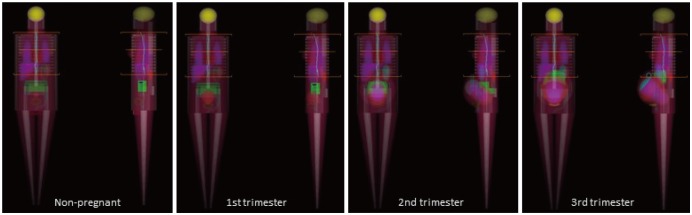
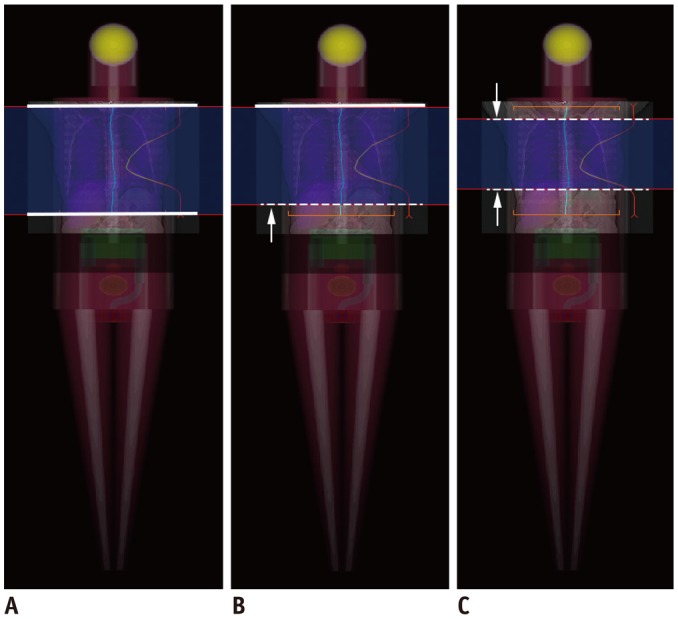
MATERIALS AND METHODS
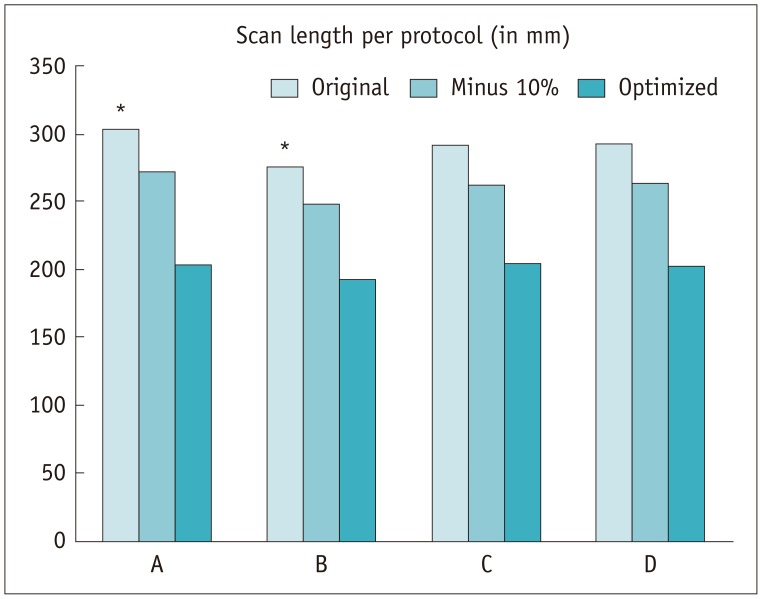
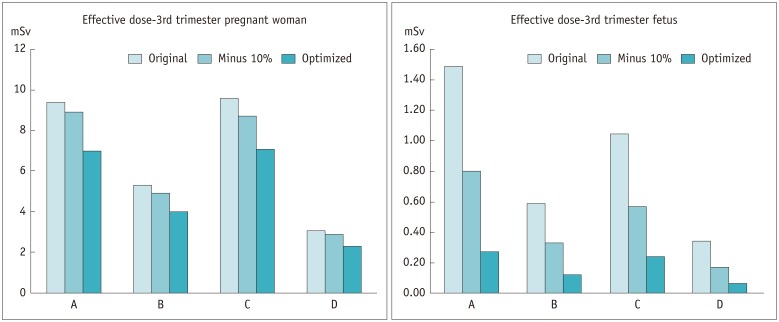
A total of 120 CTPA datasets were acquired using four distinctive scan protocols, with 30 patients per protocol. These datasets were mapped to Cristy phantoms in order to simulate pregnancy and to assess the effect of an effective radiation dose (in mSv) in the first, second, or third trimester of pregnancy, including a simulation of fetal dose in second and third trimesters. The investigated scan protocols involved a 64-slice helical scan at 120 kVp, a high-pitch dual source acquisition at 100 kVp, a dual-energy acquisition at 80/140 kVp, and an automated-kV-selection, high pitch helical scan at a reference kV of 100 kVref. The effective dose for women and fetuses was simulated before and after scan length adaptation. The original images were interpreted before and after scan length adaptations to evaluate potentially missed diagnoses.
RESULTS
Large inter-scanner and inter-protocol variations were found; application of the latest technology decreased the dose for non-pregnant women by 69% (7.0-2.2 mSv). Individual scan length optimization proved safe and effective, decreasing the fetal dose by 76-83%. Nineteen (16%) cases of pulmonary embolism were diagnosed and, after scan length optimization, none were missed.
CONCLUSION
Careful CTPA scan protocol selection and additional optimization of scan length may result in significant radiation dose reduction for a pregnant patient and her fetus, whilst maintaining diagnostic confidence.
Keyword
MeSH Terms
Figure
Reference
-
1. Kobayashi T, Nakabayashi M, Ishikawa M, Adachi T, Kobashi G, Maeda M, et al. Pulmonary thromboembolism in obstetrics and gynecology increased by 6.5-fold over the past decade in Japan. Circ J. 2008; 72:753–756. PMID: 18441455.
Article2. McLintock C, Brighton T, Chunilal S, Dekker G, McDonnell N, McRae S, et al. Councils of the Society of Obstetric Medicine of Australia and New Zealand. Australasian Society of Thrombosis and Haemostasis. Recommendations for the diagnosis and treatment of deep venous thrombosis and pulmonary embolism in pregnancy and the postpartum period. Aust N Z J Obstet Gynaecol. 2012; 52:14–22. PMID: 21972999.
Article3. Shakespeare J, Knight M. Maternal health in pregnancy: messages from the 2014 UK Confidential Enquiry into Maternal Death. Br J Gen Pract. 2015; 65:444–445. PMID: 26324470.
Article4. Heit JA, Kobbervig CE, James AH, Petterson TM, Bailey KR, Melton LJ 3rd. Trends in the incidence of venous thromboembolism during pregnancy or postpartum: a 30-year population-based study. Ann Intern Med. 2005; 143:697–706. PMID: 16287790.
Article5. Izadi M, Alemzadeh-Ansari MJ, Kazemisaleh D, Moshkani-Farahani M, Shafiee A. Do pregnant women have a higher risk for venous thromboembolism following air travel? Adv Biomed Res. 2015; 4:60. PMID: 25802829.
Article6. Leung AN, Bull TM, Jaeschke R, Lockwood CJ, Boiselle PM, Hurwitz LM, et al. American Thoracic Society documents: an official American Thoracic Society/Society of Thoracic Radiology clinical practice guideline--Evaluation of suspected pulmonary embolism in pregnancy. Radiology. 2012; 262:635–646. PMID: 22282185.
Article7. Linnemann B, Bauersachs R, Rott H, Halimeh S, Zotz R, Gerhardt A, et al. Diagnosis of pregnancy-associated venous thromboembolism - position paper of the Working Group in Women's Health of the Society of Thrombosis and Haemostasis (GTH). Vasa. 2016; 45:87–101. PMID: 27058795.
Article8. Jordan EJ, Godelman A, Levsky JM, Zalta B, Haramati LB. CT pulmonary angiography in pregnant and postpartum women: low yield, high dose. Clin Imaging. 2015; 39:251–253. PMID: 25482354.
Article9. Winer-Muram HT, Boone JM, Brown HL, Jennings SG, Mabie WC, Lombardo GT. Pulmonary embolism in pregnant patients: fetal radiation dose with helical CT. Radiology. 2002; 224:487–492. PMID: 12147847.
Article10. Gilet AG, Dunkin JM, Fernandez TJ, Button TM, Budorick NE. Fetal radiation dose during gestation estimated on an anthropomorphic phantom for three generations of CT scanners. AJR Am J Roentgenol. 2011; 196:1133–1137. PMID: 21512081.
Article11. Hendriks BM, Kok M, Mihl C, Bekkers SC, Wildberger JE, Das M. Individually tailored contrast enhancement in CT pulmonary angiography. Br J Radiol. 2016; 89:20150850. PMID: 26689096.
Article12. Shahir K, Goodman LR, Lam CA, Midia EC. Dose reduction of 69% for computed tomography pulmonary angiography: reduced z-axis computed tomography pulmonary angiography retains accuracy in those younger than 40 years. J Comput Assist Tomogr. 2013; 37:765–769. PMID: 24045255.13. Pontana F, Pagniez J, Duhamel A, Flohr T, Faivre JB, Murphy C, et al. Reduced-dose low-voltage chest CT angiography with Sinogram-affirmed iterative reconstruction versus standard-dose filtered back projection. Radiology. 2013; 267:609–618. PMID: 23297336.
Article14. Lu GM, Luo S, Meinel FG, McQuiston AD, Zhou CS, Kong X, et al. High-pitch computed tomography pulmonary angiography with iterative reconstruction at 80 kVp and 20 mL contrast agent volume. Eur Radiol. 2014; 24:3260–3268. PMID: 25100336.
Article15. Gill MK, Vijayananthan A, Kumar G, Jayarani K, Ng KH, Sun Z. Use of 100 kV versus 120 kV in computed tomography pulmonary angiography in the detection of pulmonary embolism: effect on radiation dose and image quality. Quant Imaging Med Surg. 2015; 5:524–533. PMID: 26435916.16. Li X, Ni QQ, Schoepf UJ, Wichmann JL, Felmly LM, Qi L, et al. 70-kVp high-pitch computed tomography pulmonary angiography with 40 mL contrast agent: initial experience. Acad Radiol. 2015; 22:1562–1570. PMID: 26432073.17. Wichmann JL, Hu X, Kerl JM, Schulz B, Frellesen C, Bodelle B, et al. 70 kVp computed tomography pulmonary angiography: potential for reduction of iodine load and radiation dose. J Thorac Imaging. 2015; 30:69–76. PMID: 25423130.18. Brenner D, Elliston C, Hall E, Berdon W. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol. 2001; 176:289–296. PMID: 11159059.
Article19. Remy-Jardin M, Remy J. Spiral CT angiography of the pulmonary circulation. Radiology. 1999; 212:615–636. PMID: 10478224.
Article20. Stabin MG, Watson EE, Cristy M, Ryman JC, Eckerman KF, Davis JL, et al. Mathematical models and specific absorbed fractions of photon energy in the nonpregnant adult female and at the end of each trimester of pregnancy. Oak Ridge, TN: Oak Ridge National Lab.;1995.21. Xu XG. An exponential growth of computational phantom research in radiation protection, imaging, and radiotherapy: a review of the fifty-year history. Phys Med Biol. 2014; 59:R233–R302. PMID: 25144730.
Article22. Kuzo RS, Pooley RA, Crook JE, Heckman MG, Gerber TC. Measurement of caval blood flow with MRI during respiratory maneuvers: implications for vascular contrast opacification on pulmonary CT angiographic studies. AJR Am J Roentgenol. 2007; 188:839–842. PMID: 17312076.
Article23. ICRP publication 103. The 2007 Recommendations of the International Commission on Radiological Protection. Ann ICRP. 2007; 37:1–332.24. Ozawa Y, Hara M, Shibamoto Y. The frequency of insufficient contrast enhancement of the pulmonary artery in routine contrast-enhanced chest CT and its improvement with an increased injection rate: a prospective study. J Thorac Imaging. 2011; 26:42–47. PMID: 20463614.25. Kelaranta A, Kaasalainen T, Seuri R, Toroi P, Kortesniemi M. Fetal radiation dose in computed tomography. Radiat Prot Dosimetry. 2015; 165:226–230. PMID: 25836690.
Article26. Goldberg-Stein SA, Liu B, Hahn PF, Lee SI. Radiation dose management: part 2, estimating fetal radiation risk from CT during pregnancy. AJR Am J Roentgenol. 2012; 198:W352–W356. PMID: 22451572.
Article27. Kalra MK, Maher MM, Toth TL, Hamberg LM, Blake MA, Shepard JA, et al. Strategies for CT radiation dose optimization. Radiology. 2004; 230:619–628. PMID: 14739312.
Article28. Schilham A, van der Molen AJ, Prokop M, de Jong HW. Overranging at multisection CT: an underestimated source of excess radiation exposure. Radiographics. 2010; 30:1057–1067. PMID: 20631368.
Article29. National Research Council. Health risks from exposure to low levels of ionizing radiation: BEIR VII Phase 2. Washington, DC: National Academies Press;2006.30. Pearce MS, Salotti JA, Little MP, McHugh K, Lee C, Kim KP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012; 380:499–505. PMID: 22681860.
Article31. Carrier M, Righini M, Wells PS, Perrier A, Anderson DR, Rodger MA, et al. Subsegmental pulmonary embolism diagnosed by computed tomography: incidence and clinical implications. A systematic review and meta-analysis of the management outcome studies. J Thromb Haemost. 2010; 8:1716–1722. PMID: 20546118.
Article32. Stein PD, Goodman LR, Hull RD, Dalen JE, Matta F. Diagnosis and management of isolated subsegmental pulmonary embolism: review and assessment of the options. Clin Appl Thromb Hemost. 2012; 18:20–26. PMID: 21949040.
Article33. Hutchinson BD, Navin P, Marom EM, Truong MT, Bruzzi JF. Overdiagnosis of pulmonary embolism by pulmonary CT angiography. AJR Am J Roentgenol. 2015; 205:271–277. PMID: 26204274.
Article34. Simcox LE, Ormesher L, Tower C, Greer IA. Pulmonary thrombo-embolism in pregnancy: diagnosis and management. Breathe (Sheff). 2015; 11:282–289. PMID: 27066121.
Article35. Patel SJ, Reede DL, Katz DS, Subramaniam R, Amorosa JK. Imaging the pregnant patient for nonobstetric conditions: algorithms and radiation dose considerations. Radiographics. 2007; 27:1705–1722. PMID: 18025513.
Article36. Shahir K, McCrea JM, Lozano LA, Goodman LR. Reduced z-axis technique for CT pulmonary angiography in pregnancy--validation for practical use and dose reduction. Emerg Radiol. 2015; 22:651–656. PMID: 26304188.
Article37. Kallen JA, Coughlin BF, O'Loughlin MT, Stein B. Reduced Z-axis coverage multidetector CT angiography for suspected acute pulmonary embolism could decrease dose and maintain diagnostic accuracy. Emerg Radiol. 2010; 17:31–35. PMID: 19468764.
Article38. Atalay MK, Walle NL, Egglin TK. Prevalence and nature of excluded findings at reduced scan length CT angiography for pulmonary embolism. J Cardiovasc Comput Tomogr. 2011; 5:325–332. PMID: 21930104.
Article39. Hurwitz LM, Yoshizumi TT, Goodman PC, Nelson RC, Toncheva G, Nguyen GB, et al. Radiation dose savings for adult pulmonary embolus 64-MDCT using bismuth breast shields, lower peak kilovoltage, and automatic tube current modulation. AJR Am J Roentgenol. 2009; 192:244–253. PMID: 19098206.
Article40. Perisinakis K, Tzedakis A, Spanakis K, Papadakis AE, Hatzidakis A, Damilakis J. The effect of iodine uptake on radiation dose absorbed by patient tissues in contrast enhanced CT imaging: implications for CT dosimetry. Eur Radiol. 2018; 28:151–158. PMID: 28710576.
Article41. Hendriks BMF, Eijsvoogel NG, Kok M, Martens B, Wildberger JE, Das M. Optimizing pulmonary embolism computed tomography in the age of individualized medicine: a prospective clinical study. Invest Radiol. 2018; 53:306–312. PMID: 29438139.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- CT radiation dose and radiation reduction strategies
- Strategies of computed tomography radiation dose reduction: justification and optimization
- Is It Better to Enter a Volume CT Dose Index Value before or after Scan Range Adjustment for Radiation Dose Optimization of Pediatric Cardiothoracic CT with Tube Current Modulation?
- Patient Dose Management: Focus on Practical Actions
- Radiological Justification for and Optimization of Nuclear Medicine Practices in Korea