Anesth Pain Med.
2018 Apr;13(2):207-213. 10.17085/apm.2018.13.2.207.
The implication of using dominant hand to perform laryngoscopy: an analysis of the laryngoscopic view and blade-tooth distance
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. jmlee@catholic.ac.kr
- KMID: 2437431
- DOI: http://doi.org/10.17085/apm.2018.13.2.207
Abstract
- BACKGROUND
Existing laryngoscopes are designed to be handled by the left hand, whereas most healthcare professionals are right-handed. However, controlling the laryngoscope device requires considerable strength and refinement to control the blade. We examined the usefulness of a right-handed laryngoscope to validate its clinical applicability.
METHODS
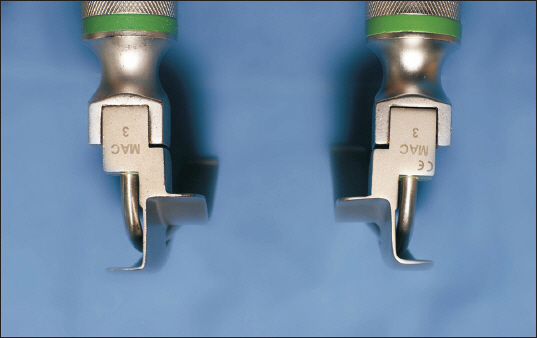
One hundred sixty-four patients for general anesthesia were involved. Laryngoscopy was performed twice for each patient, once using a conventional left-handed Macintosh No. 3 laryngoscope and once using a right-handed one, by 25 right-handed and 18 left-handed laryngoscopists. The perpendicular distance from the tip of the maxillary incisor to the flange of each blade was measured when the maximum visibility of the glottis was obtained. We compared the distances, chances of directly contacting the tooth, laryngoscopic views and subjective feeling of difficulty in handling device between the two laryngoscopes.
RESULTS
For the right-handed laryngoscopists, distance varied significantly between the two laryngoscopes (5.0 ± 3.5 and 5.7 ± 3.7 mm [mean ± standard deviation] for the conventional and right-handed laryngoscopes, respectively [P < 0.001]). The right-handed laryngoscope was associated with a decreased chance of directly contacting the teeth (P = 0.001). Additionally, the right-handed laryngoscope provided a better view than the conventional one (P = 0.005). Conversely, most of the left-handed laryngoscopists felt that the procedure using a conventional laryngoscope was easier than with a right-handed one.
CONCLUSIONS
When a right-handed laryngoscopist uses a right-handed laryngoscope, a better laryngoscopic view and a reduced chance of blade contact with the teeth can be achieved.
Keyword
MeSH Terms
Figure
Reference
-
1. Rosenblatt WH, Sukhupragarn W. Airway management. Clinical Anesthesia. 7th ed. Barash PG, Cullen BF, Stoelting RK, Cahalan MK, Stock MC, Ortega R, editors. Philadelphia: Lippincott Williams & Wilkins;2013. p. 776–7.2. Hawkins TJ. The left-handed laryngoscope. Anaesthesia. 1999; 54:1024. DOI: 10.1046/j.1365-2044.1999.1133ff.x. PMID: 10540087.3. Lee J, Choi JH, Lee YK, Kim ES, Kwon OK, Hastings RH. The Callander laryngoscope blade modification is associated with a decreased risk of dental contact. Can J Anaesth. 2004; 51:181–4. DOI: 10.1007/BF03018781. PMID: 14766698.4. Lee J, Kim BS, Chang HW, Lee Y. The usefulness of the modified laryngoscopic blade for training novice laryngoscopists. J Clin Anesth. 2005; 17:334–8. DOI: 10.1016/j.jclinane.2004.08.007. PMID: 16102681.5. Elder J, Waisel DB. Case report of the one-armed anesthesiology resident. J Clin Anesth. 2004; 16:445–8. DOI: 10.1016/j.jclinane.2004.07.004. PMID: 15567649.6. Das Adhikary S, Venkatesan T, Mohanty S, Ponniah M. Difficult laryngoscopy made easy with the use of left-hand laryngoscope blade. Br J Anaesth. 2007; 98:141–4. DOI: 10.1093/bja/ael289. PMID: 17074781.7. Rajeev S, Panda NB, Panda N, Batra YK. Left handed laryngoscope: a new look at an old instrument. Acta Anaesthesiol Belg. 2008; 59:139–40. PMID: 19051444.8. Watanabe S, Suga A, Asakura N, Takeshima R, Kimura T, Taguchi N, et al. Determination of the distance between the laryngoscope blade and the upper incisors during direct laryngoscopy: comparisons of a curved, an angulated straight, and two straight blades. Anesth Analg. 1994; 79:638–41. DOI: 10.1213/00000539-199410000-00004. PMID: 7943768.9. Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984; 39:1105–11. DOI: 10.1111/j.1365-2044.1984.tb08932.x.10. Rosenberg MB. Anesthesia-induced dental injury. Int Anesthesiol Clin. 1989; 27:120–5. DOI: 10.1097/00004311-198902720-00010. PMID: 2566582.11. Chen JJ, Susetio L, Chao CC. Oral complications associated with endotracheal general anesthesia. Ma Zui Xue Za Zhi. 1990; 28:163–9. PMID: 1977068.12. Owen H, Waddell-Smith I. Dental trauma associated with anaesthesia. Anaesth Intensive Care. 2000; 28:133–45. PMID: 10788963.13. Mulcaster JT, Mills J, Hung OR, MacQuarrie K, Law JA, Pytka S, et al. Laryngoscopic intubation: learning and performance. Anesthesiology. 2003; 98:23–7. DOI: 10.1097/00000542-200301000-00007. PMID: 12502974.14. Konrad C, Schüpfer G, Wietlisbach M, Gerber H. Learning manual skills in anesthesiology: is there a recommended number of cases for anesthetic procedures? Anesth Analg. 1998; 86:635–9. DOI: 10.1097/00000539-199803000-00037. DOI: 10.1213/00000539-199803000-00037. PMID: 9495429.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effectiveness of a Modified Laryngoscope Blade on Reducing the Potential of Dental Trauma
- Comparison between the Flexiblade Laryngoscope and the Macintosh Blade Laryngoscope in Endotracheal Intubation
- Is the Laryngeal Lift a Useful Maneuver Improving the Laryngoscopic View for Endotracheal Intubation?
- The Usefulness of Preoperative Airway Characteristics as Predictors of Dental Trauma during Laryngoscopy
- The effects of callander modification of laryngoscopic blade on hemodynamic changes according to the degree of difficult airway