Anesth Pain Med.
2018 Jul;13(3):308-313. 10.17085/apm.2018.13.3.308.
Transiliac sacroplasty for Denis 3 fracture: Two cases report
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Wooridul Spine Hospital, Seoul, Korea. answs@naver.com
- 2Department of Neurosurgery, Wooridul Spine Hospital, Seoul, Korea.
- KMID: 2436040
- DOI: http://doi.org/10.17085/apm.2018.13.3.308
Abstract
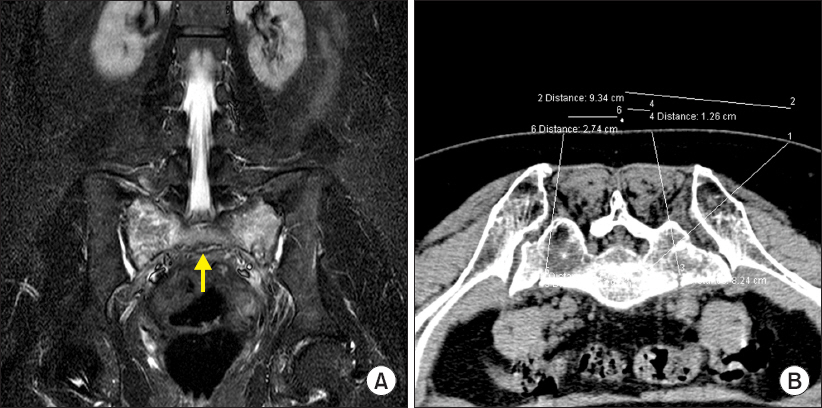
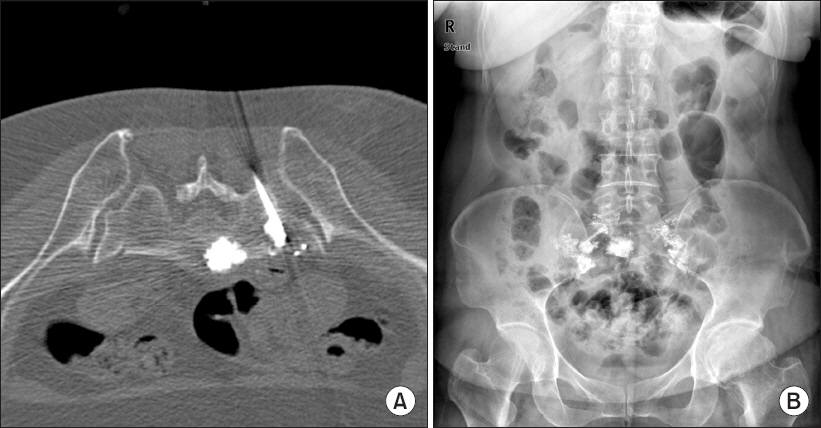
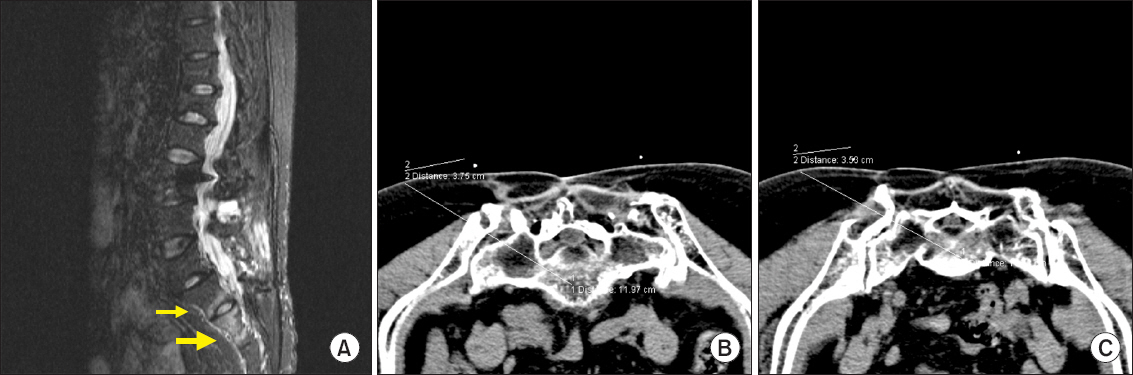
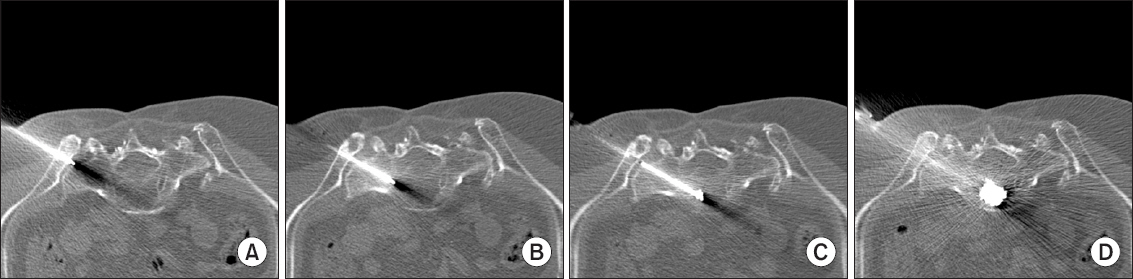
- We present two cases of percutaneous sacroplasty for sacral body fracture (Denis 3) and sacral alar fracture under multislice computed tomography (MSCT) guidance and discuss the clinical results and technical considerations. Sacroplasty is often recommended for the treatment of painful sacral insufficiency fractures, which destabilize the sacrum. However, sacroplasty for Denis zone 3 is rare because of the lack of validating controlled studies or unique technical considerations related to sacral anatomy. We performed sacroplasty for Denis zone 3 via the transiliac approach. Precise needle placement and polymethylmethacrylate cement injection were performed safely under the MSCT system. No complications occurred related to this procedure, such as iliac fracture, vascular leakage, or epidural leakage. MSCT-guided transiliac sacroplasty was a useful and effective solution in treating sacral body fracture.
Keyword
MeSH Terms
Figure
Reference
-
1. Weber M, Hasler P, Gerber H. Insufficiency fractures of the sacrum. Twenty cases and review of the literature. Spine (Phila Pa 1976). 1993; 18:2507–12. DOI: 10.1097/00007632-199312000-00021.2. Grasland A, Pouchot J, Mathieu A, Paycha F, Vinceneux P. Sacral insufficiency fractures: an easily overlooked cause of back pain in elderly women. Arch Intern Med. 1996; 156:668–74. DOI: 10.1001/archinte.1996.00440060096012. PMID: 8629880.3. Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res. 1988; 227:67–81. DOI: 10.1097/00003086-198802000-00010.4. Babayev M, Lachmann E, Nagler W. The controversy surrounding sacral insufficiency fractures: to ambulate or not to ambulate? Am J Phys Med Rehabil. 2000; 79:404–9. DOI: 10.1097/00002060-200007000-00014. PMID: 10892628.5. Lin JT, Lane JM. Sacral stress fractures. J Womens Health (Larchmt). 2003; 12:879–88. DOI: 10.1089/154099903770948104. PMID: 14670167.6. Garant M. Sacroplasty: a new treatment for sacral insufficiency fracture. J Vasc Interv Radiol. 2002; 13:1265–7. DOI: 10.1016/S1051-0443(07)61976-9.7. Brook AL, Mirsky DM, Bello JA. Computerized tomography guided sacroplasty: a practical treatment for sacral insufficiency fracture: case report. Spine (Phila Pa 1976). 2005; 30:E450–4. DOI: 10.1097/01.brs.0000172182.35619.d1. PMID: 16094265.8. Sciubba DM, Wolinsky JP, Than KD, Gokaslan ZL, Witham TF, Murphy KP. CT fluoroscopically guided percutaneous placement of transiliosacral rod for sacral insufficiency fracture: case report and technique. AJNR Am J Neuroradiol. 2007; 28:1451–4. DOI: 10.3174/ajnr.A0665. PMID: 17846189.9. Butler CL, Given CA 2nd, Michel SJ, Tibbs PA. Percutaneous sacroplasty for the treatment of sacral insufficiency fractures. AJR Am J Roentgenol. 2005; 184:1956–9. DOI: 10.2214/ajr.184.6.01841956. PMID: 15908561.10. Pommersheim W, Huang-Hellinger F, Baker M, Morris P. Sacroplasty: a treatment for sacral insufficiency fractures. AJNR Am J Neuroradiol. 2003; 24:1003–7. PMID: 12748113.11. Deen HG, Nottmeier EW. Balloon kyphoplasty for treatment of sacral insufficiency fractures. Report of three cases. Neurosurg Focus. 2005; 18:e7. DOI: 10.3171/foc.2005.18.3.8. PMID: 15771397.12. Whitlow CT, Mussat-Whitlow BJ, Mattern CW, Baker MD, Morris PP. Sacroplasty versus vertebroplasty: comparable clinical outcomes for the treatment of fracture-related pain. AJNR Am J Neuroradiol. 2007; 28:1266–70. DOI: 10.3174/ajnr.A0561. PMID: 17698526.13. Betts A. Vertebroplasty of the first sacral vertebra. Pain Physician. 2009; 12:651–7. PMID: 19461832.14. Choi G, Kim JS, Lokhande P, Lee SH. Percutaneous endoscopic lumbar discectomy by transiliac approach: a case report. Spine (Phila Pa 1976). 2009; 34:E443–6. DOI: 10.1097/BRS.0b013e31817c4f39. PMID: 19454997.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Therapeutic Considerations of Percutaneous Sacroplasty for the Sacral Insufficiency Fracture
- Percutaneous Sacroplasty for the Sacral Insufficiency Fracture Caused by Metastasis
- Biomechanical Study of Posterior Pelvic Fixations in Vertically Unstable Sacral Fractures: An Alternative to Triangular Osteosynthesis
- Teriparatide treatment shows faster healing than sacroplasty for postmenopausal women with sacral insufficiency fracture
- Percutaneous Iliosacral Screw Fixation with Cement Augmentation in Sacral Insufficient Fracture: A Case Report