Anesth Pain Med.
2018 Oct;13(4):363-371. 10.17085/apm.2018.13.4.363.
Current strategy for chronic pain after spinal surgery
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Seoul National University Bundang Hospital, Seongnam, Korea. ejchoi@snubh.org
- KMID: 2435993
- DOI: http://doi.org/10.17085/apm.2018.13.4.363
Abstract
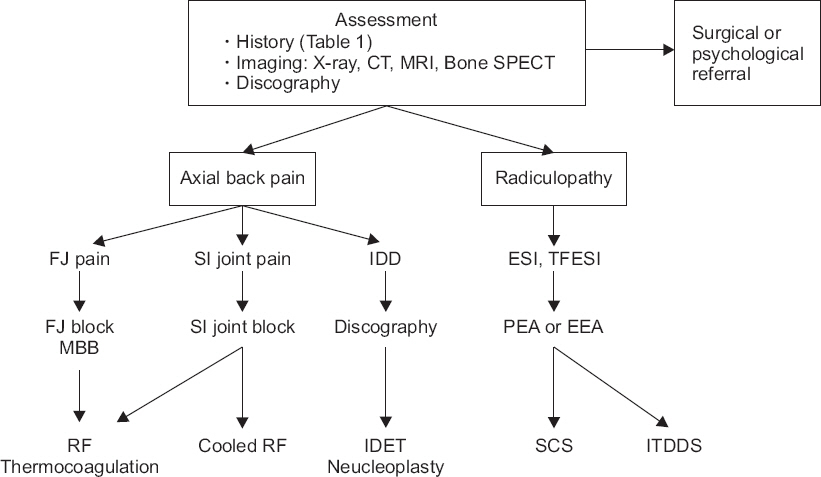
- Failed back surgery syndrome was recently renamed, as chronic pain after spinal surgery (CPSS) by international classification of disease-11. CPSS is a challenging clinical condition. It has a variety of causes associated with preoperative, intraoperative and postoperative periods. Also, psychosocial factors should be considered. Diagnostic tools must be used differently, for each patient. Imaging and interventional nerve block for diagnosis, should be used properly. Strategy of management requires a multidisciplinary approach. The effect of conservative management (medication, interventional management) and invasive procedure (spinal cord stimulator, intrathecal drug delivery system) has been studied by many researchers. However, an evidence-based guide on management of CPSS, remains necessary, and further research is needed. This review focuses on understanding and clinical approaches for CPSS.
MeSH Terms
Figure
Cited by 1 articles
-
Multimodal management strategies for chronic pain after spinal surgery: a comprehensive review
Jung-Pil Yoon, Hong-Sik Son, Jimin Lee, Gyeong-Jo Byeon
Anesth Pain Med. 2024;19(1):12-23. doi: 10.17085/apm.23122.
Reference
-
REFERENCE
1. North RB, Campbell JN, James CS, Conover-Walker MK, Wang H, Piantadosi S, et al. Failed back surgery syndrome:5-year follow-up in 102 patients undergoing repeated operation. Neurosurgery. 1991; 28:685–90. DOI: 10.1227/00006123-199105000-00008. PMID: 1831546.2. Chan CW, Peng P. Failed back surgery syndrome. Pain Med. 2011; 12:577–606. DOI: 10.1111/j.1526-4637.2011.01089.x. PMID: 21463472.3. World Health Organization. ICD-11 for mortality and morbidity statistics (ICD-11 MMS) 2018 version. World Health Organization [serial on the Internet]. 2018. [2018 Sep 1]. Available from https://icd.who.int/brows.e11/l-m/en.4. Law JD, Lehman RA, Kirsch WM. Reoperation after lumbar intervertebral disc surgery. J Neurosurg. 1978; 48:259–63. DOI: 10.3171/jns.1978.48.2.0259. PMID: 146731.5. Lehmann TR, LaRocca HS. Repeat lumbar surgery. A review of patients with failure from previous lumbar surgery treated by spinal canal exploration and lumbar spinal fusion. Spine (Phila Pa 1976). 1981; 6:615–9. DOI: 10.1097/00007632-198111000-00014.6. Lee J, Shin JS, Lee YJ, Kim MR, Choi A, Lee JH, et al. Long-term Course of Failed Back Surgery Syndrome (FBSS) patients receiving integrative Korean medicine treatment:a 1 year prospective observational multicenter study. PLoS One. 2017; 12:e0170972. DOI: 10.1371/journal.pone.0170972. PMID: 28129399. PMCID: PMC5271391.7. Shamim MS, Parekh MA, Bari ME, Enam SA, Khursheed F. Microdiscectomy for lumbosacral disc herniation and frequency of failed disc surgery. World Neurosurg. 2010; 74:611–6. DOI: 10.1016/j.wneu.2010.06.016. PMID: 21492628.8. Peul WC, van Houwelingen HC, van den Hout WB, Brand R, Eekhof JA, Tans JT, et al. Surgery versus prolonged conservative treatment for sciatica. N Engl J Med. 2007; 356:2245–56. DOI: 10.1056/NEJMoa064039. PMID: 17538084.9. Peul WC, van den Hout WB, Brand R, Thomeer RT, Koes BW. Prolonged conservative care versus early surgery in patients with sciatica caused by lumbar disc herniation:two year results of a randomised controlled trial. BMJ. 2008; 336:1355–8. DOI: 10.1136/bmj.a143. PMID: 18502911. PMCID: PMC2427077.10. Nachemson AL. Evaluation of results in lumbar spine surgery. Acta Orthop Scand Suppl. 1993; 251:130–3. DOI: 10.3109/17453679309160143. PMID: 8451971.11. Burton CV. Failed back surgery patients:the alarm bells are ringing. Surg Neurol. 2006; 65:5–6. DOI: 10.1016/j.surneu.2005.08.018. PMID: 16378838.12. Mark VH. Instrumented fusions:a need for guidelines and research. Surg Neurol. 2004; 61:318–9. DOI: 10.1016/j.surneu.2004.01.004. PMID: 15031064.13. Talbot L. Failed back surgery syndrome. BMJ. 2003; 327:985–6. DOI: 10.1136/bmj.327.7421.985. PMID: 14576254. PMCID: PMC259174.14. Carragee EJ, Alamin TF, Miller JL, Carragee JM. Discographic, MRI and psychosocial determinants of low back pain disability and remission:a prospective study in subjects with benign persistent back pain. Spine J. 2005; 5:24–35. DOI: 10.1016/j.spinee.2004.05.250. PMID: 15653082.15. Celestin J, Edwards RR, Jamison RN. Pretreatment psychosocial variables as predictors of outcomes following lumbar surgery and spinal cord stimulation:a systematic review and literature synthesis. Pain Med. 2009; 10:639–53. DOI: 10.1111/j.1526-4637.2009.00632.x. PMID: 19638142.16. Mannion AF, Elfering A. Predictors of surgical outcome and their assessment. Eur Spine J. 2006; 15(Suppl 1):S93–108. DOI: 10.1007/s00586-005-1045-9. PMID: 16320033. PMCID: PMC3454547.17. Spengler DM, Freeman C, Westbrook R, Miller JW. Low-back pain following multiple lumbar spine procedures. Failure of initial selection? Spine (Phila Pa 1976). 1980; 5:356–60. DOI: 10.1097/00007632-198007000-00008.18. Voorhies RM, Jiang X, Thomas N. Predicting outcome in the surgical treatment of lumbar radiculopathy using the pain drawing score, McGill Short Form Pain Questionnaire, and risk factors including psychosocial issues and axial joint pain. Spine J. 2007; 7:516–24. DOI: 10.1016/j.spinee.2006.10.013. PMID: 17905313.19. Carragee EJ. Psychological screening in the surgical treatment of lumbar disc herniation. Clin J Pain. 2001; 17:215–9. DOI: 10.1097/00002508-200109000-00005. PMID: 11587111.20. Guyer RD, Patterson M, Ohnmeiss DD. Failed back surgery syndrome:diagnostic evaluation. J Am Acad Orthop Surg. 2006; 14:534–43. DOI: 10.5435/00124635-200609000-00003. PMID: 16959891.21. Phillips FM, Cunningham B. Managing chronic pain of spinal origin after lumbar surgery:the role of decompressive surgery. Spine (Phila Pa 1976). 2002; 27:2547–53. DOI: 10.1097/00007632-200211150-00029.22. Slipman C. Posterior joints of the lumbar spine as a potential cause of low back pain. Pain Med. 2004; 5:287–8. DOI: 10.1111/j.1526-4637.2004.04045.x. PMID: 15367307.23. Carroll SE, Wiesel SW. Neurologic complications and lumbar laminectomy. A standardized approach to the multiply-operated lumbar spine. Clin Orthop Relat Res. 1992; (284):14–23. PMID: 1395283.24. Schaeren S, Broger I, Jeanneret B. Minimum four-year follow-up of spinal stenosis with degenerative spondylolisthesis treated with decompression and dynamic stabilization. Spine (Phila Pa 1976). 2008; 33:E636–42. DOI: 10.1097/BRS.0b013e31817d2435. PMID: 18708915.25. Harrop JS, Youssef JA, Maltenfort M, Vorwald P, Jabbour P, Bono CM, et al. Lumbar adjacent segment degeneration and disease after arthrodesis and total disc arthroplasty. Spine (Phila Pa 1976). 2008; 33:1701–7. DOI: 10.1097/BRS.0b013e31817bb956. PMID: 18594464.26. Hong X, Liu L, Bao J, Shi R, Fan Y, Wu X. Characterization and risk factor analysis for reoperation after microendoscopic diskectomy. Orthopedics. 2015; 38:e490–6. DOI: 10.3928/01477447-20150603-57. PMID: 26091222.27. Parker SL, Mendenhall SK, Godil SS, Sivasubramanian P, Cahill K, Ziewacz J, et al. Incidence of low back pain after lumbar discectomy for herniated disc and its effect on patient-reported outcomes. Clin Orthop Relat Res. 2015; 473:1988–99. DOI: 10.1007/s11999-015-4193-1. PMID: 25694267. PMCID: PMC4419014.28. Manchikanti L, Manchikanti KN, Gharibo CG, Kaye AD. Efficacy of percutaneous adhesiolysis in the treatment of lumbar post surgery syndrome. Anesth Pain Med. 2016; 6:e26172. PMID: 27574583. PMCID: PMC4979454.29. Jamison DE, Hsu E, Cohen SP. Epidural adhesiolysis:an evidence-based review. J Neurosurg Sci. 2014; 58:65–76. PMID: 24819483.30. Kizilkilic O, Yalcin O, Sen O, Aydin MV, Yildirim T, Hurcan C. The role of standing flexion-extension radiographs for spondylolisthesis following single level disk surgery. Neurol Res. 2007; 29:540–3. DOI: 10.1179/016164107X164166. PMID: 17535575.31. Manchikanti L, Manchukonda R, Pampati V, Damron KS, McManus CD. Prevalence of facet joint pain in chronic low back pain in postsurgical patients by controlled comparative local anesthetic blocks. Arch Phys Med Rehabil. 2007; 88:449–55. DOI: 10.1016/j.apmr.2007.01.015. PMID: 17398245.32. Al-Riyami K, Vöö S, Gnanasegaran G, Pressney I, Meir A, Casey A, et al. The role of bone SPECT/CT in patients with persistent or recurrent lumbar pain following lumbar spine stabilization surgery. Eur J Nucl Med Mol Imaging. 2018; Advance Access published on Sep 6 2018. doi:10.1007/s00259-018-4141-x. DOI: 10.1007/s00259-018-4141-x.33. Russo VM, Dhawan RT, Baudracco I, Dharmarajah N, Lazzarino AI, Casey AT. Hybrid bone SPECT/CT imaging in evaluation of chronic low back pain:correlation with facet joint arthropathy. World Neurosurg. 2017; 107:732–8. DOI: 10.1016/j.wneu.2017.08.092. PMID: 28847557.34. Van de Kelft E, Verleye G, Van de Kelft AS, Melis K, Van Goethem J. Validation of topographic hybrid single-photon emission computerized tomography with computerized tomography scan in patients with and without nonspecific chronic low back pain. A prospective comparative study. Spine J. 2017; 17:1457–63. DOI: 10.1016/j.spinee.2017.05.007. PMID: 28495243.35. Waguespack A, Schofferman J, Slosar P, Reynolds J. Etiology of long-term failures of lumbar spine surgery. Pain Med. 2002; 3:18–22. DOI: 10.1046/j.1526-4637.2002.02007.x. PMID: 15102214.36. Slipman CW, Shin CH, Patel RK, Isaac Z, Huston CW, Lipetz JS, et al. Etiologies of failed back surgery syndrome. Pain Med. 2002; 3:200–14. DOI: 10.1046/j.1526-4637.2002.02033.x. PMID: 15099254.37. Thawrani DP, Agabegi SS, Asghar F. Diagnosing sacroiliac joint pain. J Am Acad Orthop Surg. 2018; Advance Access published on Oct 1 2018. doi:10.5435/JAAOS-D-17-00132. DOI: 10.5435/JAAOS-D-17-00132.38. Horton WC, Daftari TK. Which disc as visualized by magnetic resonance imaging is actually a source of pain? A correlation between magnetic resonance imaging and discography. Spine (Phila Pa 1976). 1992; 17(6 Suppl):S164–71. DOI: 10.1097/00007632-199206001-00018. PMID: 1385901.39. Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med. 1994; 331:69–73. DOI: 10.1056/NEJM199407143310201. PMID: 8208267.40. Carragee EJ, Chen Y, Tanner CM, Truong T, Lau E, Brito JL. Provocative discography in patients after limited lumbar discectomy:a controlled, randomized study of pain response in symptomatic and asymptomatic subjects. Spine (Phila Pa 1976). 2000; 25:3065–71. DOI: 10.1097/00007632-200012010-00014.41. Manchikanti L, Soin A, Benyamin RM, Singh V, Falco FJ, Calodney AK, et al. An update of the systematic appraisal of the accuracy and utility of discography in chronic spinal pain. Pain Physician. 2018; 21:91–110. PMID: 29565943.42. Sachs BL, Vanharanta H, Spivey MA, Guyer RD, Videman T, Rashbaum RF, et al. Dallas discogram description. A new classification of CT/discography in low-back disorders. Spine (Phila Pa 1976). 1987; 12:287–94. DOI: 10.1097/00007632-198704000-00018.43. Schellhas KP, Pollei SR, Gundry CR, Heithoff KB. Lumbar disc high-intensity zone. Correlation of magnetic resonance imaging and discography. Spine (Phila Pa 1976). 1996; 21:79–86. DOI: 10.1097/00007632-199601010-00018.44. Lee JH, Shin KH, Park SJ, Lee GJ, Lee CH, Kim DH, et al. Comparison of clinical efficacy between transforaminal and interlaminar epidural injections in lumbosacral disc herniation:a systematic review and meta-analysis. Pain Physician. 2018; 21:433–48. PMID: 30282389.45. Eckel TS, Bartynski WS. Epidural steroid injections and selective nerve root blocks. Tech Vasc Interv Radiol. 2009; 12:11–21. DOI: 10.1053/j.tvir.2009.06.004. PMID: 19769903.46. Wong JJ, Côté P, Ameis A, Varatharajan S, Varatharajan T, Shearer HM, et al. Are non-steroidal anti-inflammatory drugs effective for the management of neck pain and associated disorders, whiplash-associated disorders, or non-specific low back pain? A systematic review of systematic reviews by the Ontario Protocol for Traffic Injury Management (OPTIMa) collaboration. Eur Spine J. 2016; 25:34–61. DOI: 10.1007/s00586-015-3891-4. PMID: 25827308.47. Roelofs PD, Deyo RA, Koes BW, Scholten RJ, van Tulder MW. Non-steroidal anti-inflammatory drugs for low back pain. Cochrane Database Syst Rev. 2008; (1):CD000396. DOI: 10.1002/14651858.CD000396.pub3.48. Machado GC, Maher CG, Ferreira PH, Pinheiro MB, Lin CW, Day RO, et al. Efficacy and safety of paracetamol for spinal pain and osteoarthritis:systematic review and meta-analysis of randomised placebo controlled trials. BMJ. 2015; 350:h1225. DOI: 10.1136/bmj.h1225. PMID: 25828856. PMCID: PMC4381278.49. Tetsunaga T, Tetsunaga T, Tanaka M, Ozaki T. Efficacy of tramadol-acetaminophen tablets in low back pain patients with depression. J Orthop Sci. 2015; 20:281–6. DOI: 10.1007/s00776-014-0674-4. PMID: 25644033.50. Imamura T. Significant efficacy of Tramadol/Acetaminophen in elderly patients with chronic low back pain uncontrolled by NSAIDs:an observational study. Open Orthop J. 2015; 9:120–5. DOI: 10.2174/1874325001509010120. PMID: 26157527. PMCID: PMC4484344.51. Hussain A, Erdek M. Interventional pain management for failed back surgery syndrome. Pain Pract. 2014; 14:64–78. DOI: 10.1111/papr.12035. PMID: 23374545.52. Attal N, Cruccu G, Baron R, Haanpää M, Hansson P, Jensen TS, et al. European Federation of Neurological Societies. EFNS guidelines on the pharmacological treatment of neuropathic pain:2010 revision. Eur J Neurol. 2010; 17:1113-. e88. DOI: 10.1111/j.1468-1331.2010.02999.x. PMID: 20402746.53. Abdi S, Datta S, Trescot AM, Schultz DM, Adlaka R, Atluri SL, et al. Epidural steroids in the management of chronic spinal pain:a systematic review. Pain Physician. 2007; 10:185–212. PMID: 17256030.54. Benny B, Azari P. The efficacy of lumbosacral transforaminal epidural steroid injections:a comprehensive literature review. J Back Musculoskelet Rehabil. 2011; 24:67–76. DOI: 10.3233/BMR-2011-0279. PMID: 21558610.55. Parr AT, Diwan S, Abdi S. Lumbar interlaminar epidural injections in managing chronic low back and lower extremity pain:a systematic review. Pain Physician. 2009; 12:163–88. PMID: 19165302.56. Manchikanti L, Singh V, Cash KA, Pampati V, Datta S. Preliminary results of a randomized, equivalence trial of fluoroscopic caudal epidural injections in managing chronic low back pain:part 3--post surgery syndrome. Pain Physician. 2008; 11:817–31. PMID: 19057628.57. Schofferman J, Kine G. Effectiveness of repeated radiofrequency neurotomy for lumbar facet pain. Spine (Phila Pa 1976). 2004; 29:2471–3. DOI: 10.1097/01.brs.0000143170.47345.44.58. Cohen SP, Hurley RW, Christo PJ, Winkley J, Mohiuddin MM, Stojanovic MP. Clinical predictors of success and failure for lumbar facet radiofrequency denervation. Clin J Pain. 2007; 23:45–52. DOI: 10.1097/01.ajp.0000210941.04182.ea. PMID: 17277644.59. Cohen SP, Hurley RW, Buckenmaier CC 3rd, Kurihara C, Morlando B, Dragovich A. Randomized placebo-controlled study evaluating lateral branch radiofrequency denervation for sacroiliac joint pain. Anesthesiology. 2008; 109:279–88. DOI: 10.1097/ALN.0b013e31817f4c7c. PMID: 18648237. PMCID: PMC2666931.60. Hansen H, Manchikanti L, Simopoulos TT, Christo PJ, Gupta S, Smith HS, et al. A systematic evaluation of the therapeutic effectiveness of sacroiliac joint interventions. Pain Physician. 2012; 15:E247–78. PMID: 22622913.61. Manchikanti L, Singh V, Cash KA, Pampati V, Datta S. A comparative effectiveness evaluation of percutaneous adhesiolysis and epidural steroid injections in managing lumbar post surgery syndrome:a randomized, equivalence controlled trial. Pain Physician. 2009; 12:E355–68. PMID: 19935992.62. Yousef AA, EL-Deen AS, Al-Deeb AE. The role of adding hyaluronidase to fluoroscopically guided caudal steroid and hypertonic saline injection in patients with failed back surgery syndrome:a prospective, double-blinded, randomized study. Pain Pract. 2010; 10:548–53. DOI: 10.1111/j.1533-2500.2009.00357.x. PMID: 20412501.63. Kim SB, Lee KW, Lee JH, Kim MA, An BW. The effect of hyaluronidase in interlaminar lumbar epidural injection for failed back surgery syndrome. Ann Rehabil Med. 2012; 36:466–73. DOI: 10.5535/arm.2012.36.4.466. PMID: 22977771. PMCID: PMC3438412.64. Lee F, Jamison DE, Hurley RW, Cohen SP. Epidural lysis of adhesions. Korean J Pain. 2014; 27:3–15. DOI: 10.3344/kjp.2014.27.1.3. PMID: 24478895. PMCID: PMC3903797.65. Kim SH, Choi SS. Epidural neuroplasty/epidural adhesiolysis. Anesth Pain Med. 2016; 11:14–22. DOI: 10.17085/apm.2016.11.1.14.66. Manchikanti L, Rivera JJ, Pampati V, Damron KS, Beyer CD, Brandon DE, et al. Spinal endoscopic adhesiolysis in the management of chronic low back pain:a preliminary report of a randomized, double-blind trial. Pain Physician. 2003; 6:259–67. PMID: 16880869.67. Manchikanti L, Pampati V, Bakhit CE, Pakanati RR. Non-endoscopic and endoscopic adhesiolysis in post-lumbar laminectomy syndrome:a one-year outcome study and cost effectiveness analysis. Pain Physician. 1999; 2:52–8. PMID: 16906216.68. Dashfield AK, Taylor MB, Cleaver JS, Farrow D. Comparison of caudal steroid epidural with targeted steroid placement during spinal endoscopy for chronic sciatica:a prospective, randomized, double-blind trial. Br J Anaesth. 2005; 94:514–9. DOI: 10.1093/bja/aei084. PMID: 15695544.69. Helm Ii S, Simopoulos TT, Stojanovic M, Abdi S, El Terany MA. Effectiveness of thermal annular procedures in treating discogenic low back pain. Pain Physician. 2017; 20:447–70. PMID: 28934777.70. Saal JA, Saal JS. Intradiscal electrothermal treatment for chronic discogenic low back pain:prospective outcome study with a minimum 2-year follow-up. Spine (Phila Pa 1976). 2002; 27:966–73. DOI: 10.1097/00007632-200205010-00017.71. Cohen SP, Williams S, Kurihara C, Griffith S, Larkin TM. Nucleoplasty with or without intradiscal electrothermal therapy (IDET) as a treatment for lumbar herniated disc. J Spinal Disord Tech. 2005; 18(Suppl):S119–24. DOI: 10.1097/01.bsd.0000127823.54485.3f. PMID: 15699797.72. Kumar K, Taylor RS, Jacques L, Eldabe S, Meglio M, Molet J, et al. Spinal cord stimulation versus conventional medical management for neuropathic pain:a multicentre randomised controlled trial in patients with failed back surgery syndrome. Pain. 2007; 132:179–88. DOI: 10.1016/j.pain.2007.07.028. PMID: 17845835.73. Kumar K, Taylor RS, Jacques L, Eldabe S, Meglio M, Molet J, et al. The effects of spinal cord stimulation in neuropathic pain are sustained:a 24-month follow-up of the prospective randomized controlled multicenter trial of the effectiveness of spinal cord stimulation. Neurosurgery. 2008; 63:762–70. DOI: 10.1227/01.NEU.0000325731.46702.D9. PMID: 18981888.74. Manca A, Kumar K, Taylor RS, Jacques L, Eldabe S, Meglio M, et al. Quality of life, resource consumption and costs of spinal cord stimulation versus conventional medical management in neuropathic pain patients with failed back surgery syndrome (PROCESS trial). Eur J Pain. 2008; 12:1047–58. DOI: 10.1016/j.ejpain.2008.01.014. PMID: 18359255.75. North RB, Kidd D, Shipley J, Taylor RS. Spinal cord stimulation versus reoperation for failed back surgery syndrome:a cost effectiveness and cost utility analysis based on a randomized, controlled trial. Neurosurgery. 2007; 61:361–9. DOI: 10.1227/01.NEU.0000255522.42579.EA. PMID: 17762749.76. Hamza M, Doleys D, Wells M, Weisbein J, Hoff J, Martin M, et al. Prospective study of 3-year follow-up of low-dose intrathecal opioids in the management of chronic nonmalignant pain. Pain Med. 2012; 13:1304–13. DOI: 10.1111/j.1526-4637.2012.01451.x. PMID: 22845187.77. Caraway D, Walker V, Becker L, Hinnenthal J. Successful Discontinuation of systemic opioids after implantation of an intrathecal drug delivery system. Neuromodulation. 2015; 18:508–15. DOI: 10.1111/ner.12318. PMID: 26053626.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spinal Cord Stimulation in Pain Management: A Review
- Treatment of Failed Back Surgery Syndrome with a Spinal Cord Stimulator: A report of 2 cases
- Treatment of Chronic Low Back and Leg Pain Using a Spinal Cord Stimulator: Two case reports
- Spinal Cord Stimulation for Control of Chronic Pain
- Spontaneous Lead Breakage in Implanted Spinal Cord Stimulation Systems