Ann Dermatol.
2012 May;24(2):175-180.
Onychomycosis Due to Nondermatophytic Molds
- Affiliations
-
- 1Department of Dermatology, Dongguk University College of Medicine, Gyeongju, Korea. smg@dongguk.ac.kr
- 2Department of Laboratory Medicine, Dongguk University College of Medicine, Gyeongju, Korea.
Abstract
- BACKGROUND
Although there have been many studies about onychomycosis due to nondermatophytic molds (NDM), few studies about etiologic agents including NDM in onychomycosis have been reported in Korea. Objective: This study investigated onychomycosis due to NDM in the Gyeongju area of Korea.
OBJECTIVE
This study investigated onychomycosis due to NDM in the Gyeongju area of Korea.
METHODS
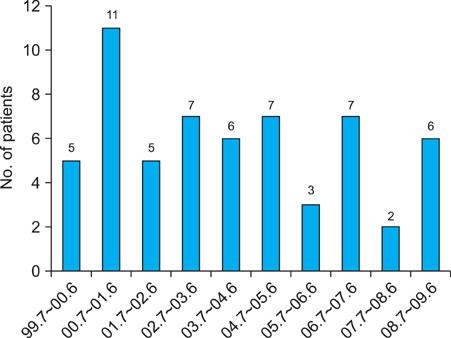
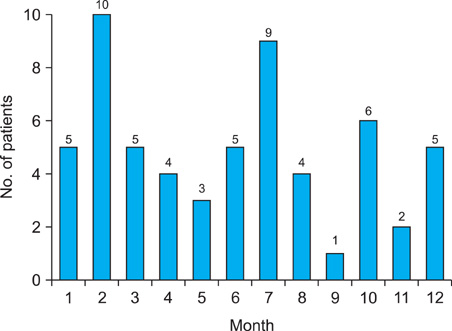
In the 10-year period from 1999~2009, we reviewed 59 patients with onychomycosis due to NDM. The etiologic agents were identified by cultures on Sabouraud's Dextrose agar with and without cycloheximide. In some cases, internal transcribed spacer sequence analysis was done. NDM isolated considered pathogens when the presence of fungal elements was identified by direct microscopy observation and in follow-up cultures yielding the same fungi.
RESULTS
Onychomycosis due to NDM comprised 2.3% of all onychomycosis. Of the 59 patients with onychomycosis due to NDM, 84.7% were toenail onychomycosis and 15.3% were fingernail onychomycosis. The incidence rate was highest in the fifth decade (27.1%). The ratio of male to female patients was 1:1.6. The frequency of associated diseases, in descending order, was hypertension, diabetes mellitus, and cerebral hematoma. Distal and lateral subungual onychomycosis (86.4%) was the most common clinical type of onychomycosis. Aspergillus spp. was the most frequently isolated etiologic agent of onychomycosis due to NDM (83.0%). Other causative agents were Scopulariopsis brevicaulis (10.2%), Acremonium spp. (3.4%), Fusarium solani (1.7%), and Chaetomium globosum (1.7%).
CONCLUSION
Because of the increase in onychomycosis due to NDM, we suggest the need of a careful mycological examination in patients with onychomycosis.
Keyword
MeSH Terms
Figure
Reference
-
1. Verma S, Heffernan MP. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Superficial fungal infections: dermatophytosis, onychomycosis, tinea nigra, piedra. Fitzpatrick's dermatology in general medicine. 2008. 7th ed. New York: McGraw-Hill;1807–1821.2. Tosti A, Piraccini BM, Lorenzi S. Onychomycosis caused by nondermatophytic molds: clinical features and response to treatment of 59 cases. J Am Acad Dermatol. 2000. 42:217–224.
Article3. Moreno G, Arenas R. Other fungi causing onychomycosis. Clin Dermatol. 2010. 28:160–163.
Article4. Bassiri-Jahromi S, Khaksar AA. Nondermatophytic moulds as a causative agent of onychomycosis in tehran. Indian J Dermatol. 2010. 55:140–143.
Article5. Hilmioğlu-Polat S, Metin DY, Inci R, Dereli T, Kilinç I, Tümbay E. Non-dermatophytic molds as agents of onychomycosis in Izmir, Turkey - a prospective study. Mycopathologia. 2005. 160:125–128.
Article6. Gianni C, Cerri A, Crosti C. Non-dermatophytic onychomycosis. An understimated entity? A study of 51 cases. Mycoses. 2000. 43:29–33.
Article7. Bonifaz A, Cruz-Aguilar P, Ponce RM. Onychomycosis by molds. Report of 78 cases. Eur J Dermatol. 2007. 17:70–72.8. Kim YJ, Lim SW, Suh MK, Choi JH, Bang JS, Lee JW, et al. Four cases of toenail onychomycosis caused by Scopulariopsis brevicaulis. Korean J Med Mycol. 2001. 6:97–103.9. Kim SC, Chon TH, Kim HU. Onychomycosis due to Scopulariopsis brevicaulis. Korean J Dermatol. 2000. 38:1566–1568.10. Lee BJ, Kim IJ, Suh SB. Two cases of onychomycosis due to Aspergillus repens. Korean J Dermatol. 1981. 19:881–886.11. Suh SB, Byun DK, Lee KY. A case of onychomycosis by Aspergillus sydowi. Korean J Dermatol. 1968. 6:39–43.12. Suh JC, Yeum JS, Na GY, Seo SK, Suh MK. A simple detection method to the resistance to the treatment of onychomycosis: a case report of Aspergillus sydowii onychomycosis. Ann Dermatol. 2001. 13:62–65.
Article13. Lim SW, Kwon SW, Suh MK, Lee HC, Choi JH, Lee JW, et al. A case of onychomycosis caused by Fusarium solani. Korean J Med Mycol. 2003. 8:21–25.14. Kim JE, Park HJ, Lee JY, Cho BK, Kim SO. A case of onychomycosis with acute paronychia caused by Fusarium oxysporum. Korean J Med Mycol. 2002. 7:170–174.15. Lim SW, Suh MK, Ha GY. Clinical features and identification of etiologic agents in onychomycosis. (1999-2002). Korean J Dermatol. 2004. 42:53–60.16. Baran R, Hay RJ, Tosti A, Haneke E. A new classification of onychomycosis. Br J Dermatol. 1998. 139:567–571.
Article17. English MP. Nails and fungi. Br J Dermatol. 1976. 94:697–701.
Article18. Roberts DT. Onychomycosis: current treatment and future challenges. Br J Dermatol. 1999. 141:Suppl 56. 1–4.
Article19. Baudraz-Rosselet F, Ruffieux C, Lurati M, Bontems O, Monod M. Onychomycosis insensitive to systemic terbinafine and azole treatments reveals non-dermatophyte moulds as infectious agents. Dermatology. 2010. 220:164–168.
Article20. Ranawaka RR, de Silva N, Ragunathan RW. Onychomycosis caused by Fusarium sp in Sri Lanka: prevalence, clinical features and response to itraconazole pulse therapy in six cases. J Dermatolog Treat. 2008. 19:308–312.
Article21. Gianni C, Romano C. Clinical and histological aspects of toenail onychomycosis caused by Aspergillus spp.: 34 cases treated with weekly intermittent terbinafine. Dermatology. 2004. 209:104–110.
Article22. Tosti A, Piraccini BM, Lorenzi S, Iorizzo M. Treatment of nondermatophyte mold and Candida onychomycosis. Dermatol Clin. 2003. 21:491–497.23. Gupta AK, Ryder JE, Summerbell RC. The diagnosis of nondermatophyte mold onychomycosis. Int J Dermatol. 2003. 42:272–273.
Article24. Gupta AK, Ryder JE, Baran R, Summerbell RC. Non-dermatophyte onychomycosis. Dermatol Clin. 2003. 21:257–268.
Article25. Kemna ME, Elewski BE. A U.S. epidemiologic survey of superficial fungal diseases. J Am Acad Dermatol. 1996. 35:539–542.
Article26. Dogra S, Kumar B, Bhansali A, Chakrabarty A. Epidemiology of onychomycosis in patients with diabetes mellitus in India. Int J Dermatol. 2002. 41:647–651.
Article27. Cathcart S, Cantrell W, Elewski B. Onychomycosis and diabetes. J Eur Acad Dermatol Venereol. 2009. 23:1119–1122.
Article28. Gupta M, Sharma NL, Kanga AK, Mahajan VK, Tegta GR. Onychomycosis: Clinico-mycologic study of 130 patients from Himachal Pradesh, India. Indian J Dermatol Venereol Leprol. 2007. 73:389–392.
Article29. Ramani R, Srinivas CR, Ramani A, Kumari TG, Shivananda PG. Molds in onychomycosis. Int J Dermatol. 1993. 32:877–878.
Article30. Latha R, Sasikala R, Muruganandam N, Shiva Prakash MR. Onychomycosis due to ascomycete Chaetomium globosum: a case report. Indian J Pathol Microbiol. 2010. 53:566–567.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Features and Identification of Etiologic Agents in Onychomycosis (1999-2002)
- A Clinical and Mycological Study of Onychomycosis in the Elderly Over 10 Years (2001-2010)
- A Case of Onychomycosis Caused by Fusarium solani
- A Case of Toenail Onychomycosis Due to Aspergillus terreus
- Four Cases of Toenail Onychomycosis Caused by Scopulariopsis brevicaulis