Anesth Pain Med.
2019 Jan;14(1):85-90. 10.17085/apm.2019.14.1.85.
Paraplegia after celiac plexus neurolysis in a patient with pancreatic cancer: A case report and literature review
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Konkuk University School of Medicine, Seoul, Korea. painfree@kuh.ac.kr
- KMID: 2434204
- DOI: http://doi.org/10.17085/apm.2019.14.1.85
Abstract
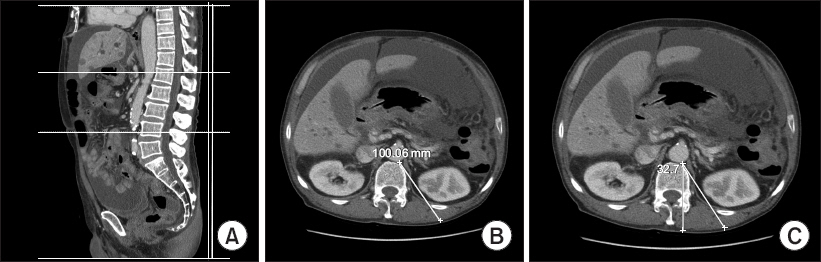
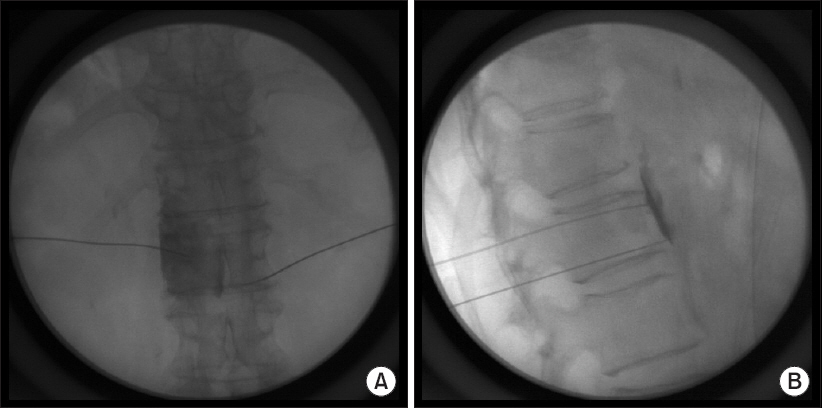
- A 65-year-old male patient underwent C-arm fluoroscopy-guided bilateral celiac plexus neurolysis to relieve peritoneal seeding-related pain associated with pancreatic cancer. Following confirmation of spreading, and no intravascular injection of contrast media, 7.5 ml of 0.25% chirocaine was injected in each side. The pain subsided after the block, with no motor or sensory deficits. Subsequently, celiac plexus neurolysis with 99.8% alcohol was performed using a posterolateral approach under fluoroscopic guidance. The patient was instructed to maintain a prone position for 2 hours while the procedure was performed. Approximately 4 hours later, the patient experienced paralysis of both lower extremities and hypoesthesia. Emergent magnetic resonance imaging of the thoracic and lumbar spine revealed gray matter signal change in the cord and conus medullaris at the T10-L1 level, and decreased perfusion at the T11-T12 vertebral bodies, suggesting spinal cord infarction. The patient remained paraplegic until his death 24 days later.
Keyword
MeSH Terms
Figure
Reference
-
1. Eisenberg E, Carr DB, Chalmers TC. Neurolytic celiac plexus block for treatment of cancer pain: a meta-analysis. Anesth Analg. 1995; 80:290–5. DOI: 10.1213/00000539-199502000-00015. PMID: 7818115.2. Na AJ, Moon DE, Suh JH. Paraplegia following celiac plexus block: a case report. J Korean Pain Soc. 1993; 6:129–32.3. Davies DD. Incidence of major complications of neurolytic coeliac plexus block. J R Soc Med. 1993; 86:264–6. DOI: 10.1097/00132586-199312000-00033. PMID: 8505748. PMCID: PMC1294001.4. Galizia EJ, Lahiri SK. Paraplegia following coeliac plexus block with phenol. Case report. Br J Anaesth. 1974; 46:539–40. DOI: 10.1093/bja/46.7.539. PMID: 4458776.5. Wong GY, Brown DL. Transient paraplegia following alcohol celiac plexus block. Reg Anesth. 1995; 20:352–5. PMID: 7577786.6. van Dongen RT, Crul BJ. Paraplegia following coeliac plexus block. Anaesthesia. 1991; 46:862–3. DOI: 10.1111/j.1365-2044.1991.tb09603.x. PMID: 1952003.7. Woodham MJ, Hanna MH. Paraplegia after coeliac plexus block. Anaesthesia. 1989; 44:487–9. DOI: 10.1111/j.1365-2044.1989.tb11376.x. PMID: 2474258.8. Jabbal SS, Hunton J. Reversible paraplegia following coeliac plexus block. Anaesthesia. 1992; 47:857–8. DOI: 10.1111/j.1365-2044.1992.tb03147.x. PMID: 1280001.9. Jeon SS, Moon DE, Ryu KH. A case of transient paraplegia following celiac plexus block with alcohol: a case report. Anesth Pain Med. 2010; 5:16–9.10. Fujii L, Clain JE, Morris JM, Levy MJ. Anterior spinal cord infarction with permanent paralysis following endoscopic ultrasound celiac plexus neurolysis. Endoscopy. 2012; 44(Suppl 2):UCTN: E265-6. DOI: 10.1055/s-0032-1309708. PMID: 22814912.11. Minaga K, Kitano M, Imai H, Miyata T, Kudo M. Acute spinal cord infarction after EUS-guided celiac plexus neurolysis. Gastrointest Endosc. 2016; 83:1039–40. DOI: 10.1016/j.gie.2015.10.044. PMID: 26551729.12. Koyyalagunta D, Engle MP, Yu J, Feng L, Novy DM. The effectiveness of alcohol versus phenol based splanchnic nerve neurolysis for the treatment of intra-abdominal cancer pain. Pain Physician. 2016; 19:281–92. PMID: 27228515.13. Ishiwatari H, Hayashi T, Yoshida M, Ono M, Masuko H, Sato T, et al. Phenol-based endoscopic ultrasound-guided celiac plexus neurolysis for East Asian alcohol-intolerant upper gastrointestinal cancer patients: a pilot study. World J Gastroenterol. 2014; 20:10512–7. DOI: 10.3748/wjg.v20.i30.10512. PMID: 25132769. PMCID: PMC4130860.14. Brown DL, Rorie DK. Altered reactivity of isolated segmental lumbar arteries of dogs following exposure to ethanol and phenol. Pain. 1994; 56:139–43. DOI: 10.1016/0304-3959(94)90087-6. PMID: 8008403.15. Mittal MK, Rabinstein AA, Wijdicks EF. Pearls & oy-sters: acute spinal cord infarction following endoscopic ultrasound-guided celiac plexus neurolysis. Neurology. 2012; 78:e57–9. DOI: 10.1212/WNL.0b013e318248df51. PMID: 22371417.16. Garcea G, Thomasset S, Berry DP, Tordoff S. Percutaneous splanchnic nerve radiofrequency ablation for chronic abdominal pain. ANZ J Surg. 2005; 75:640–4. DOI: 10.1111/j.1445-2197.2005.03486.x. PMID: 16076323.17. Kim DH, Kim YC, Kim KH. Minimally invasive percutaneous spinal techniques. Philadelphia: Elsevier Saunders;2010. p. 175.18. Kumar A, Tripathi SS, Dhar D, Bhattacharya A. A case of reversible paraparesis following celiac plexus block. Reg Anesth Pain Med. 2001; 26:75–8. DOI: 10.1053/rapm.2001.20090. DOI: 10.1097/00115550-200101000-00017. PMID: 11172517.19. Leung JW, Bowen-Wright M, Aveling W, Shorvon PJ, Cotton PB. Coeliac plexus block for pain in pancreatic cancer and chronic pancreatitis. Br J Surg. 1983; 70:730–2. DOI: 10.1002/bjs.1800701212. PMID: 6640255.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of transient paraplegia following celiac plexus block with alcohol: A case report
- Endoscopic ultrasound-guided celiac plexus neurolysis for managing abdominal pain related with advanced cancer
- Diaphragmatic paralysis following alcohol celiac plexus neurolysis and a review of literature: A case report
- A Case of Pancreatic Cancer and Opioid Withdrawal after Endoscopic Ultrasound-guided Celiac Plexus Neurolysis
- Recent topics on endoscopic ultrasonography-guided celiac plexus neurolysis