Intest Res.
2018 Oct;16(4):546-553. 10.5217/ir.2018.00052.
Experience of patients with inflammatory bowel disease in using a home fecal calprotectin test as an objective reported outcome for self-monitoring
- Affiliations
-
- 1Department of Internal Medicine, National Taiwan University Hospital, National Taiwan University College of Medicine, Taipei, Taiwan. shuchenwei@ntu.edu.tw
- 2Department of Integrated Diagnostics & Therapeutics, National Taiwan University Hospital, Taipei, Taiwan.
- 3Department of Internal Medicine, Far Eastern Memorial Hospital, New Taipei, Taiwan.
- 4Department of Chemical Engineering & Materials Science, Yuan-Ze University, Taoyuan, Taiwan.
- KMID: 2434156
- DOI: http://doi.org/10.5217/ir.2018.00052
Abstract
- BACKGROUND/AIMS
Fecal calprotectin (fC) level is a predictive marker of mucosal healing for patients with inflammatory bowel disease (IBD). Home fC tests are now available. We evaluated the performance of the smartphone-based IBDoc home testing system in patients with IBD and obtained their feedback as an objective patient-reported outcome.
METHODS
This prospective study enrolled consecutive patients with IBD in clinical remission. fC in the same stool sample was assessed by using both the laboratory test (Quantum Blue calprotectin test) and home test (IBDoc). The correlation between the 2 tests was analyzed using the Pearson method. In addition, the patients were asked to fill a questionnaire based on their experience.
RESULTS
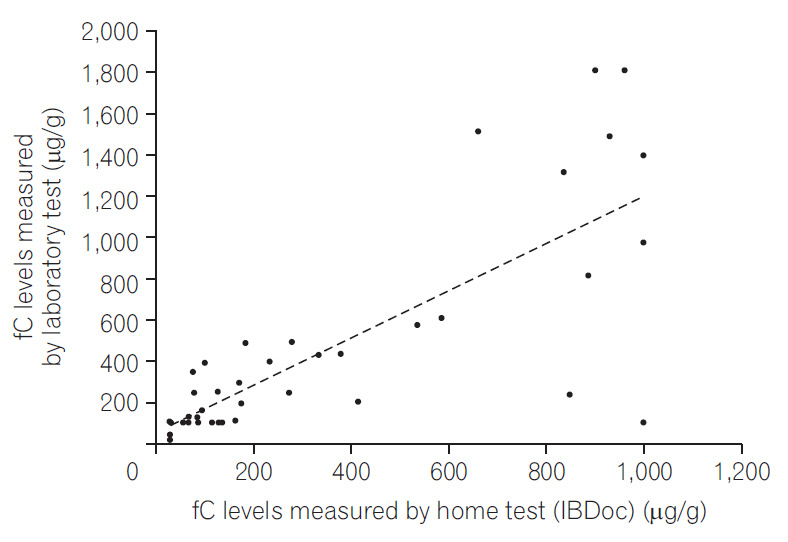
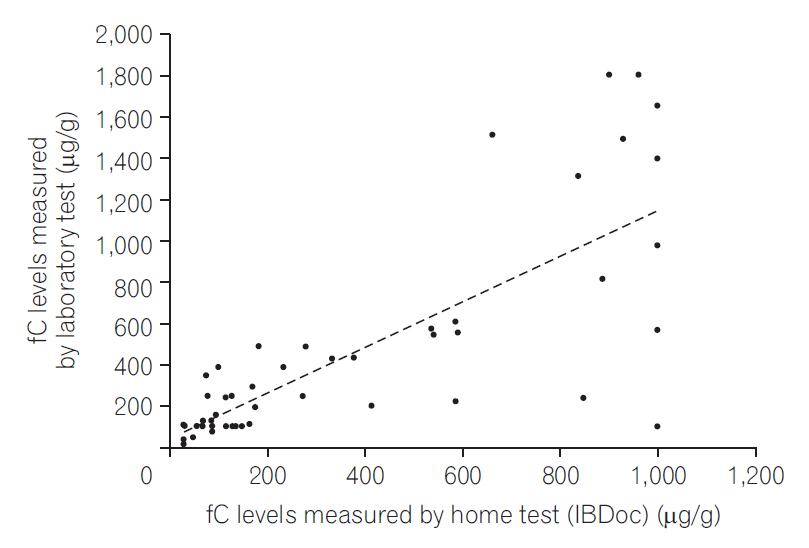
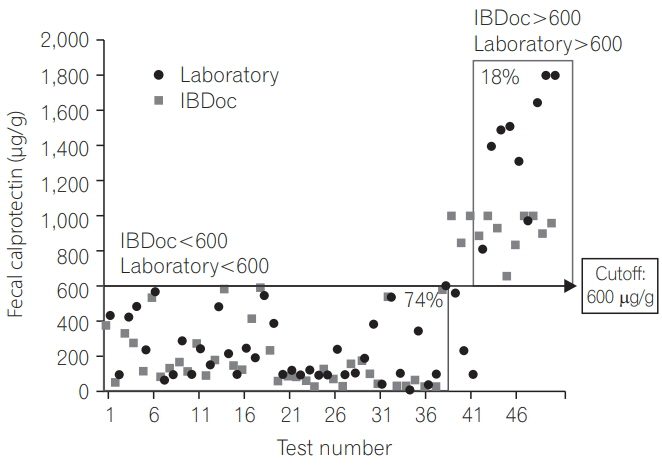
Fifty-one patients with IBD (68 tests and 49 questionnaires) were included. The correlation between Quantum Blue test and IBDoc was good (r=0.776, P < 0.0001). After the test, 56% patients found IBDoc easy to perform, and 96% were satisfied with it. Thirty-nine patients (80%) had a strong (>70%) probability to use it for future monitoring if the price was acceptable. By using 250 μg/g as the cutoff, the agreement between home test and laboratory results was 80%, and by using 600 μg/g as the cutoff, the agreement increased to 92%.
CONCLUSIONS
The correlation between the laboratory and home tests was good. Most patients found the home test to be feasible and easy to use and preferred it over laboratory test and endoscopy for monitoring. Therefore, the home test could be used as an objective patient-reported outcome.
MeSH Terms
Figure
Cited by 1 articles
-
Home-based fecal calprotectin test is expected to play an important role in patients with inflammatory bowel diseases
Young-Ho Kim
Intest Res. 2018;16(4):507-508. doi: 10.5217/ir.2018.00136.
Reference
-
1. Rutter M, Saunders B, Wilkinson K, et al. Severity of inflammation is a risk factor for colorectal neoplasia in ulcerative colitis. Gastroenterology. 2004; 126:451–459.
Article2. Colombel JF, Panaccione R, Bossuyt P, et al. Effect of tight control management on Crohn’s disease (CALM): a multicentre, randomised, controlled phase 3 trial. Lancet. 2018; 390:2779–2789.
Article3. Nielsen OH, Vainer B, Madsen SM, Seidelin JB, Heegaard NH. Established and emerging biological activity markers of inflammatory bowel disease. Am J Gastroenterol. 2000; 95:359–367.
Article4. Vermeire S, Van Assche G, Rutgeerts P. Laboratory markers in IBD: useful, magic, or unnecessary toys? Gut. 2006; 55:426–431.
Article5. D’Haens G, Ferrante M, Vermeire S, et al. Fecal calprotectin is a surrogate marker for endoscopic lesions in inflammatory bowel disease. Inflamm Bowel Dis. 2012; 18:2218–2224.
Article6. Lin WC, Wong JM, Tung CC, et al. Fecal calprotectin correlated with endoscopic remission for Asian inflammatory bowel disease patients. World J Gastroenterol. 2015; 21:13566–13573.
Article7. Wei SC. Could fecal calprotectin enter mainstream use for diagnosing and monitoring inflammatory bowel disease? Intest Res. 2016; 14:293–294.
Article8. Jang HW, Kim HS, Park SJ, et al. Accuracy of three different fecal calprotectin tests in the diagnosis of inflammatory bowel disease. Intest Res. 2016; 14:305–313.
Article9. Elkjaer M, Burisch J, Voxen Hansen V, et al. A new rapid home test for faecal calprotectin in ulcerative colitis. Aliment Pharmacol Ther. 2010; 31:323–330.
Article10. Heida A, Knol M, Kobold AM, et al. Agreement between home-based measurement of stool calprotectin and ELISA results for monitoring inflammatory bowel disease activity. Clin Gastroenterol Hepatol. 2017; 15:1742–1749. e2.
Article11. Bello C, Roseth A, Guardiola J, et al. Usability of a home-based test for the measurement of fecal calprotectin in asymptomatic IBD patients. Dig Liver Dis. 2017; 49:991–996.
Article12. Vinding KK, Elsberg H, Thorkilgaard T, et al. Fecal calprotectin measured by patients at home using smartphones: a new clinical tool in monitoring patients with inflammatory bowel disease. Inflamm Bowel Dis. 2016; 22:336–344.
Article13. Elkjaer M. E-health: web-guided therapy and disease self-management in ulcerative colitis. Impact on disease outcome, quality of life and compliance. Dan Med J. 2012; 59:B4478.14. Kawashima K, Ishihara S, Yuki T, et al. Fecal calprotectin more accurately predicts endoscopic remission of Crohn’s disease than serological biomarkers evaluated using balloon-assisted enteroscopy. Inflamm Bowel Dis. 2017; 23:2027–2034.
Article15. Vázquez Morón JM, Pallarés Manrique H, Machancoses FH, Ramos Lora M, Ruiz Frutos C. Accurate cut-offs for predicting endoscopic activity and mucosal healing in Crohn’s disease with fecal calprotectin. Rev Esp Enferm Dig. 2017; 109:130–136.
Article16. Sandborn WJ, Panés J, Zhang H, Yu D, Niezychowski W, Su C. Correlation between concentrations of fecal calprotectin and outcomes of patients with ulcerative colitis in a phase 2 trial. Gastroenterology. 2016; 150:96–102.
Article17. Yamaguchi S, Takeuchi Y, Arai K, et al. Fecal calprotectin is a clinically relevant biomarker of mucosal healing in patients with quiescent ulcerative colitis. J Gastroenterol Hepatol. 2016; 31:93–98.
Article18. Dhaliwal A, Zeino Z, Tomkins C, et al. Utility of faecal calprotectin in inflammatory bowel disease (IBD): what cut-offs should we apply? Frontline Gastroenterol. 2015; 6:14–19.
Article19. Bjarnason I. The use of fecal calprotectin in inflammatory bowel disease. Gastroenterol Hepatol (N Y). 2017; 13:53–56.20. Bossuyt P, Vermeire S. Treat to target in inflammatory bowel disease. Curr Treat Options Gastroenterol. 2016; 14:61–72.
Article21. Bossuyt P, Pouillon L, Bonnaud G, Danese S, Peyrin-Biroulet L. E-health in inflammatory bowel diseases: more challenges than opportunities? Dig Liver Dis. 2017; 49:1320–1326.
Article22. Bossuyt P, Pouillon L, Peyrin-Biroulet L. Primetime for e-health in IBD? Nat Rev Gastroenterol Hepatol. 2017; 14:133–134.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fecal Calprotectin in Inflammatory Bowel Disease
- Accuracy of three different fecal calprotectin tests in the diagnosis of inflammatory bowel disease
- Home-based fecal calprotectin test is expected to play an important role in patients with inflammatory bowel diseases
- The role of fecal calprotectin in pediatric disease
- Could fecal calprotectin enter mainstream use for diagnosing and monitoring inflammatory bowel disease?