Allergy Asthma Respir Dis.
2019 Jan;7(1):44-50. 10.4168/aard.2019.7.1.44.
Clinical application of the Pediatric Acute Lung Injury Consensus Conference definition of acute respiratory distress syndrome
- Affiliations
-
- 1Department of Pediatrics, Severance Children's Hospital, Yonsei University College of Medicine, Seoul, Korea. sophi1@yuhs.ac
- 2Sowha Children's Hospital, Seoul, Korea.
- KMID: 2434129
- DOI: http://doi.org/10.4168/aard.2019.7.1.44
Abstract
- PURPOSE
Despite improved quality of intensive care, acute respiratory distress syndrome (ARDS) significantly contributes to mortality in critically ill children. As pre-existing definitions of ARDS were adult-oriented standards, the Pediatric Acute Lung Injury Consensus Conference (PALICC) group released a new definition of pediatric ARDS. In this study, we aimed to assess the performance of PALICC definition for ARDS risk stratification.
METHODS
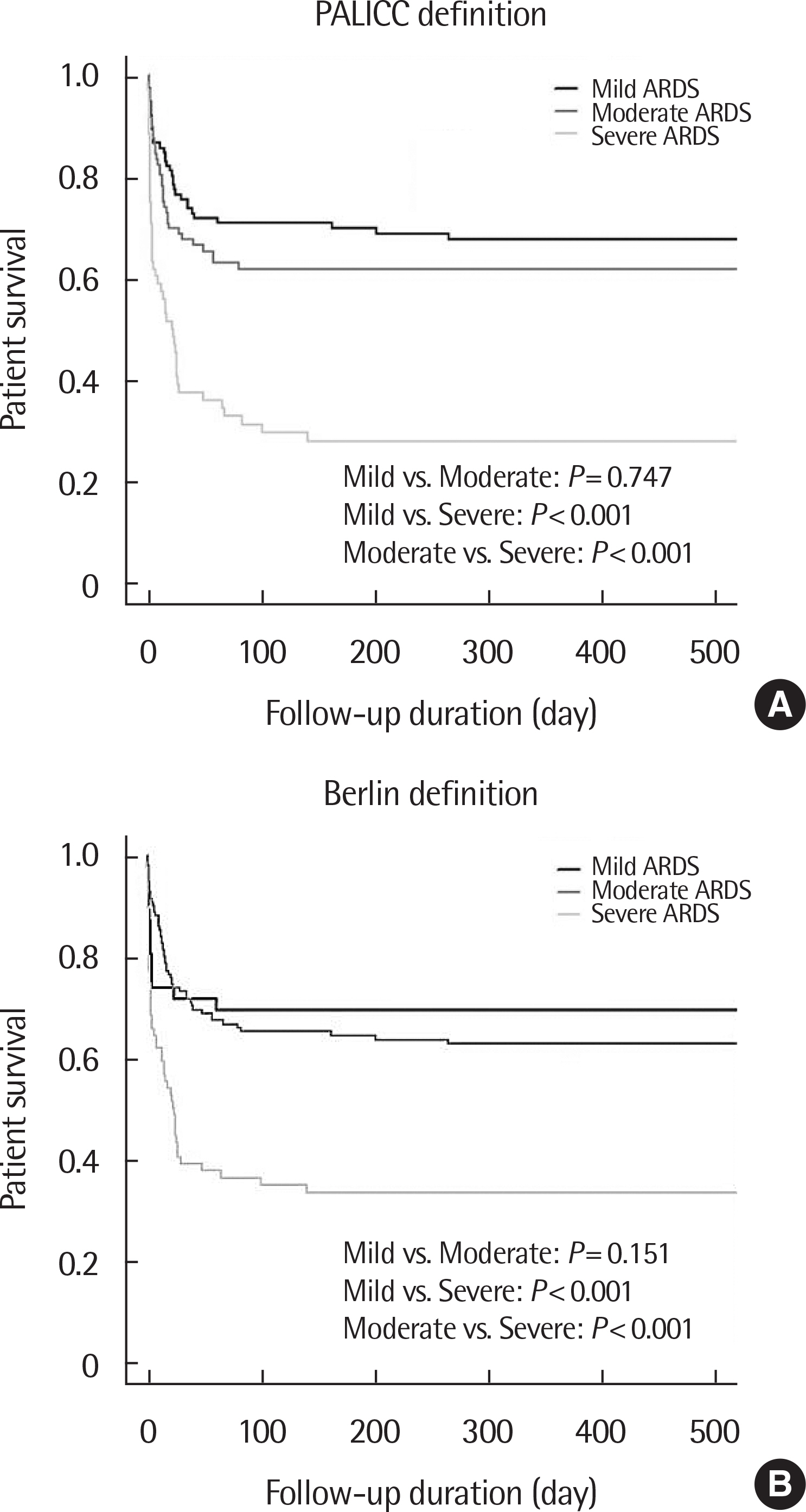
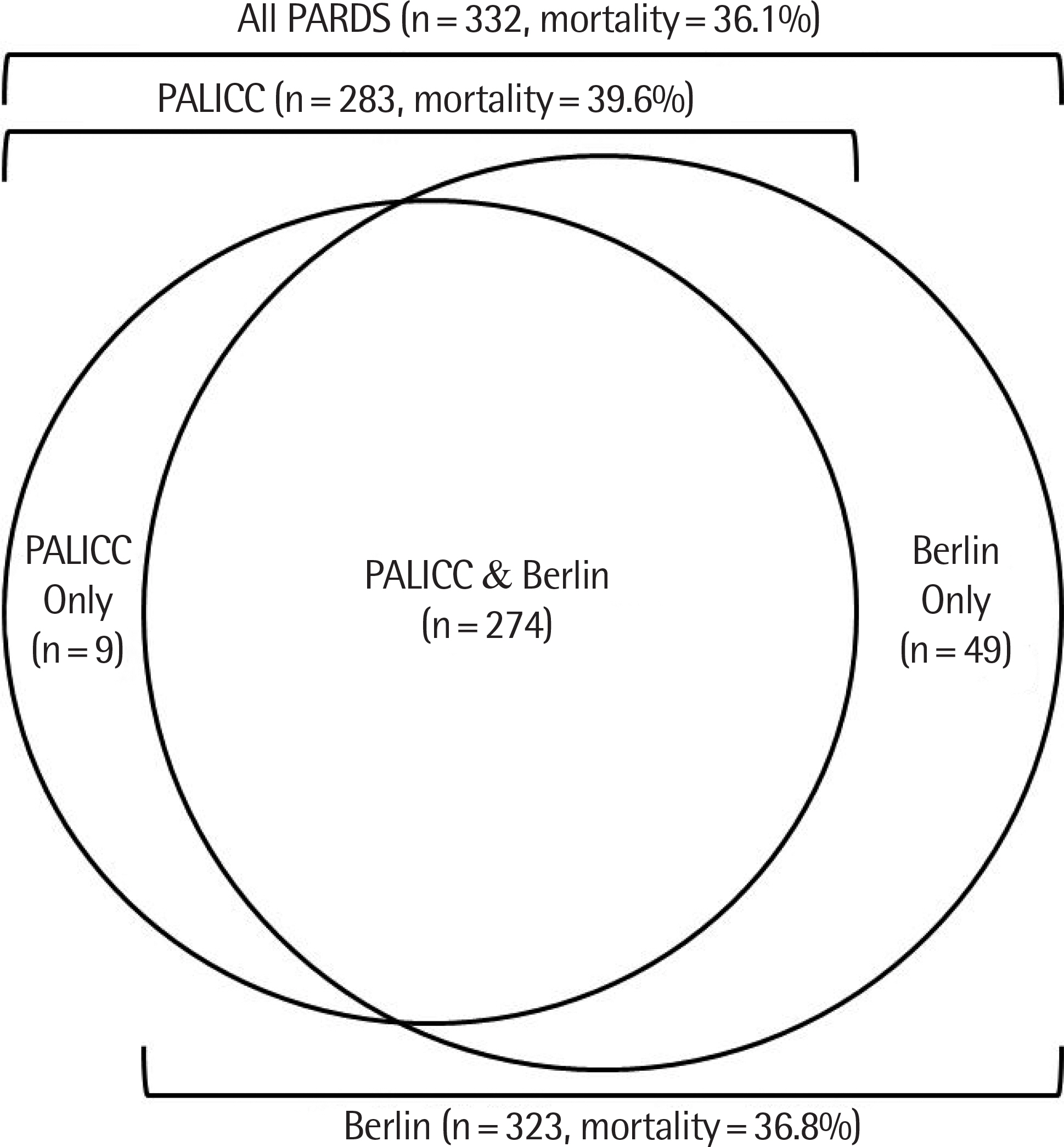
Total 332 patients who admitted to the intensive care unit at Severance Hospital from January 2009 to December 2016 and diagnosed as having ARDS by either the PALICC definition or the Berlin definition were retrospectively analyzed. Patient characteristics and mortality rates were compared between the individual severity groups according to both definitions.
RESULTS
The overall mortality rate was 36.1%. The mortality rate increased across the severity classes according to both definitions (26% in mild, 37% in moderate and 68% in severe by the PALICC definition [P<0.001]; 20% in mild, 32% in moderate and 64% in severe by the Berlin definition [P<0.001]). The mortality risk increased only for severe ARDS in both definitions (hazard ratio [95% confidence interval]: 2.279 [1.414-3.672], P=0.001 by the PALICC definition; 2.674 [1.518-4.712], P=0.001 by the Berlin definition). There was no significant difference in mortality discrimination between the 2 definitions (difference in integrated area under the curve: 0.017 [−0.018 to 0.049]).
CONCLUSION
The PALICC definition demonstrated similar discrimination power on PARDS' severity and mortality as the Berlin definition.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Ashbaugh DG, Bigelow DB, Petty TL, Levine BE. Acute respiratory distress in adults. Lancet. 1967; 2:319–23.
Article2. Zimmerman JJ, Akhtar SR, Caldwell E, Rubenfeld GD. Incidence and outcomes of pediatric acute lung injury. Pediatrics. 2009; 124:87–95.
Article3. Erickson S, Schibler A, Numa A, Nuthall G, Yung M, Pascoe E, et al. Acute lung injury in pediatric intensive care in Australia and New Zealand: a prospective, multicenter, observational study. Pediatr Crit Care Med. 2007; 8:317–23.4. Heidemann SM, Nair A, Bulut Y, Sapru A. Pathophysiology and management of acute respiratory distress syndrome in children. Pediatr Clin North Am. 2017; 64:1017–37.
Article5. Yu WL, Lu ZJ, Wang Y, Shi LP, Kuang FW, Qian SY, et al. The epidemiology of acute respiratory distress syndrome in pediatric intensive care units in China. Intensive Care Med. 2009; 35:136–43.
Article6. Wong JJ, Loh TF, Testoni D, Yeo JG, Mok YH, Lee JH. Epidemiology of pediatric acute respiratory distress syndrome in singapore: risk factors and predictive respiratory indices for mortality. Front Pediatr. 2014; 2:78.
Article7. Wong JJ, Phan HP, Phumeetham S, Ong JS, Chor YK, Qian S, et al. Risk stratification in pediatric acute respiratory distress syndrome: a multicenter observational study. Crit Care Med. 2017; 45:1820–8.8. Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, et al. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994; 149(3 Pt 1):818–24.
Article9. Villar J, Pérez-Méndez L, Kacmarek RM. Current definitions of acute lung injury and the acute respiratory distress syndrome do not reflect their true severity and outcome. Intensive Care Med. 1999; 25:930–5.
Article10. Villar J, Pérez-Méndez L, López J, Belda J, Blanco J, Saralegui I, et al. An early PEEP/FIO2 trial identifies different degrees of lung injury in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2007; 176:795–804.11. ARDS Definition Task Force. Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012; 307:2526–33.12. Khemani RG, Wilson DF, Esteban A, Ferguson ND. Evaluating the Berlin definition in pediatric ARDS. Intensive Care Med. 2013; 39:2213–6.
Article13. De Luca D, Piastra M, Chidini G, Tissieres P, Calderini E, Essouri S, et al. The use of the Berlin definition for acute respiratory distress syndrome during infancy and early childhood: multicenter evaluation and expert consensus. Intensive Care Med. 2013; 39:2083–91.
Article14. Ferguson ND, Kacmarek RM, Chiche JD, Singh JM, Hallett DC, Mehta S, et al. Screening of ARDS patients using standardized ventilator settings: influence on enrollment in a clinical trial. Intensive Care Med. 2004; 30:1111–6.
Article15. Santschi M, Randolph AG, Rimensberger PC, Jouvet P. Pediatric Acute Lung Injury Mechanical Ventilation Investigators; Pediatric Acute Lung Injury and Sepsis Investigators Network. Mechanical ventilation strategies in children with acute lung injury: a survey on stated practice pattern*. Pediatr Crit Care Med. 2013; 14:e332–7.16. Cheifetz IM. Pediatric acute respiratory distress syndrome. Respir Care. 2011; 56:1589–99.
Article17. Thomas NJ, Jouvet P, Willson D. Acute lung injury in children–kids really aren't just “little adults”. Pediatr Crit Care Med. 2013; 14:429–32.
Article18. Pediatric Acute Lung Injury Consensus Conference Group. Pediatric acute respiratory distress syndrome: consensus recommendations from the Pediatric Acute Lung Injury Consensus Conference. Pediatr Crit Care Med. 2015; 16:428–39.19. Khemani RG, Smith LS, Zimmerman JJ, Erickson S. Pediatric Acute Lung Injury Consensus Conference Group. Pediatric acute respiratory distress syndrome: definition, incidence, and epidemiology: proceedings from the Pediatric Acute Lung Injury Consensus Conference. Pediatr Crit Care Med. 2015; 16(5 Suppl 1):S23–40.20. Parvathaneni K, Belani S, Leung D, Newth CJ, Khemani RG. Evaluating the performance of the pediatric acute lung injury consensus conference definition of acute respiratory distress syndrome. Pediatr Crit Care Med. 2017; 18:17–25.
Article21. Gupta S, Sankar J, Lodha R, Kabra SK. Comparison of prevalence and outcomes of pediatric acute respiratory distress syndrome using Pediatric Acute Lung Injury Consensus Conference Criteria and Berlin Definition. Front Pediatr. 2018; 6:93.
Article22. Pollack MM, Patel KM, Ruttimann UE. The Pediatric Risk of Mortality III–Acute Physiology Score (PRISM III-APS): a method of assessing physiologic instability for pediatric intensive care unit patients. J Pediatr. 1997; 131:575–81.23. Straney L, Clements A, Parslow RC, Pearson G, Shann F, Alexander J, et al. Paediatric index of mortality 3: an updated model for predicting mortality in pediatric intensive care*. Pediatr Crit Care Med. 2013; 14:673–81.24. López-Fernández Y, Azagra AM, de la Oliva P, Modesto V, Sánchez JI, Parrilla J, et al. Pediatric acute lung injury epidemiology and natural history study: incidence and outcome of the acute respiratory distress syndrome in children. Crit Care Med. 2012; 40:3238–45.25. Cheifetz IM. Pediatric ARDS. Respir Care. 2017; 62:718–31.
Article26. Hu X, Qian S, Xu F, Huang B, Zhou D, Wang Y, et al. Incidence, management and mortality of acute hypoxemic respiratory failure and acute respiratory distress syndrome from a prospective study of Chinese paediatric intensive care network. Acta Paediatr. 2010; 99:715–21.
Article27. Lodha R, Kabra SK, Pandey RM. Acute respiratory distress syndrome: experience at a tertiary care hospital. Indian Pediatr. 2001; 38:1154–9.28. Fuchs H, Mendler MR, Scharnbeck D, Ebsen M, Hummler HD. Very low tidal volume ventilation with associated hypercapnia–effects on lung injury in a model for acute respiratory distress syndrome. PLoS One. 2011; 6:e23816.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- New Definition of Acute Respiratory Distress Syndrome
- Application of the Berlin definition in children with acute respiratory distress syndrome
- Nonventilatory medical treatments for acute respiratory distress syndrome and acute lung injury
- Effect of Recruiting Maneuvers in a Patient with Acute Lung Injury after Femoral Nailing: A case report
- A Clinical Study of the Acute Respiratory Distress Syndrome in Children