Ewha Med J.
2019 Jan;42(1):6-9. 10.12771/emj.2019.42.1.6.
Transient Pseudohypoaldosteronism in a 5-Month-old Infant Manifested as a Failure to Thrive
- Affiliations
-
- 1Department of Pediatrics, Ewha Womans University College of Medicine, Seoul, Korea. hyesk@ewha.ac.kr
- KMID: 2433550
- DOI: http://doi.org/10.12771/emj.2019.42.1.6
Abstract
- Pseudohypoaldosteronism (PHA) in infants is manifested by presence of hyperkalemia, hyponatremia, and metabolic acidosis. At initial stages, PAH is generally suspected as congenital adrenal hyperplasia. Transient PHA has been reported in infants with urinary tract infection and urinary tract malformation. We report a case of 5-month-old infant with failure to thrive and finally diagnosed with transient PHA due to urinary tract infection with vesicoureteral reflux.
Keyword
MeSH Terms
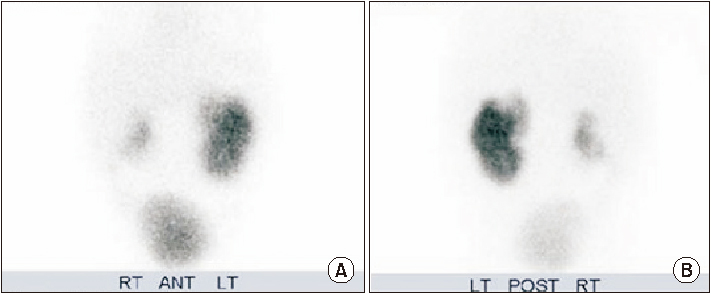
Figure
Reference
-
1. Geller DS. Mineralocorticoid resistance. Clin Endocrinol (Oxf). 2005; 62:513–520.
Article2. Bogdanovic R, Stajic N, Putnik J, Paripovic A. Transient type 1 pseudo-hypoaldosteronism: report on an eight-patient series and literature review. Pediatr Nephrol. 2009; 24:2167–2175.
Article3. Dolezel Z, Starha J, Novotna D, Dostalkova D. Secondary pseudohypoaldosteronism in an infant with pyelonephritis. Bratisl Lek Listy. 2004; 105:435–437.4. Hanukoglu A. Type I pseudohypoaldosteronism includes two clinically and genetically distinct entities with either renal or multiple target organ defects. J Clin Endocrinol Metab. 1991; 73:936–944.
Article5. Zennaro MC, Lombes M. Mineralocorticoid resistance. Trends Endocrinol Metab. 2004; 15:264–270.
Article6. Pujo L, Fagart J, Gary F, Papadimitriou DT, Claes A, Jeunemaitre X, et al. Mineralocorticoid receptor mutations are the principal cause of renal type 1 pseudohypoaldosteronism. Hum Mutat. 2007; 28:33–40.
Article7. Rodriguez-Soriano J, Vallo A, Oliveros R, Castillo G. Transient pseudohypoaldosteronism secondary to obstructive uropathy in infancy. J Pediatr. 1983; 103:375–380.8. Proctor G, Linas S. Type 2 pseudohypoaldosteronism: new insights into renal potassium, sodium, and chloride handling. Am J Kidney Dis. 2006; 48:674–693.
Article9. Watanabe T. Reversible secondary pseudohypoaldosteronism. Pediatr Nephrol. 2003; 18:486.
Article10. Belot A, Ranchin B, Fichtner C, Pujo L, Rossier BC, Liutkus A, et al. Pseudohypoaldosteronisms, report on a 10-patient series. Nephrol Dial Transplant. 2008; 23:1636–1641.
Article11. Melzi ML, Guez S, Sersale G, Terzi F, Secco E, Marra G, et al. Acute pyelonephritis as a cause of hyponatremia/hyperkalemia in young infants with urinary tract malformations. Pediatr Infect Dis J. 1995; 14:56–59.
Article12. Bowden SA, Cozzi C, Hickey SE, Thrush DL, Astbury C, Nuthakki S. Autosomal dominant pseudohypoaldosteronism type 1 in an infant with salt wasting crisis associated with urinary tract infection and obstructive uropathy. Case Rep Endocrinol. 2013; 2013:524647.
Article13. Fujinaga S, Ohtomo Y, Someya T, Shimizu T, Yamashiro Y. Transient pseudohypoaldosteronism complicating acute renal failure in an infant with vesico-ureteral reflux and pyelonephritis. Pediatr Int. 2009; 51:744–746.
Article14. Delhikumar CG, Narayanan P, Mahadevan S. Pseudohypoaldosteronism masquerading as congenital adrenal hyperplasia. Indian J Pediatr. 2012; 79:115–116.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Transient Pseudohypoaldosteronism in an Infant with Vesicoureteral Reflux
- Two Cases of Pseudohypoaldosteronism Type I
- A case of pseudohypoaldosteronism type 1 with a mutation in the mineralocorticoid receptor gene
- Pseudohypoaldosteronism Type 1 with a NovelMutation in the NR3C2 Gene: A Case Report
- A Case of Diencephalic Syndrome Presented as Failure to Thrive from Three Month of Age