Chonnam Med J.
2016 Sep;52(3):212-216. 10.4068/cmj.2016.52.3.212.
Association between Vitamin D Status and Risk of Peripheral Arterial Disease: The Dong-gu Study
- Affiliations
-
- 1Department of Preventive Medicine, Chonnam National University Medical School, Gwangju, Korea. mhshinx@paran.com
- 2Jeonnam Regional Cancer Center, Chonnam National University, Hwasun Hospital, Hwasun, Korea.
- 3Department of Preventive Medicine & Institute of Wonkwang Medical Science, Wonkwang University College of Medicine, Iksan, Korea.
- 4Department of Preventive Medicine, Chungnam National University Medical School, Daejeon, Korea.
- 5Department of Neurology & Research Institute of Clinical Medicine, Chonbuk National University-Biomedical Institute of Chonbuk National University Hospital, Jeonju, Korea.
- 6Department of Preventive Medicine, Seonam University College of Medicine, Namwon, Korea.
- 7Department of Preventive Medicine, Chosun University Medical School, Gwangju, Korea.
- KMID: 2432272
- DOI: http://doi.org/10.4068/cmj.2016.52.3.212
Abstract
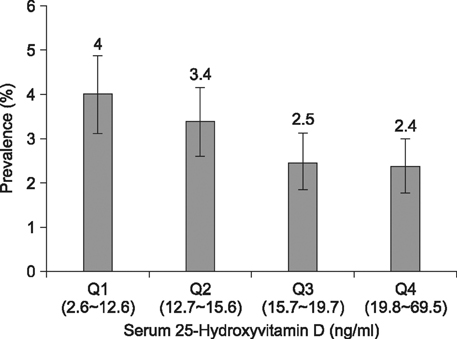
- Low levels of vitamin D have been associated with increased cardiovascular disease risk. However, few studies have evaluated the association between vitamin D status and peripheral arterial disease (PAD). We therefore aimed to investigate whether low 25-hydroxyvitamin D (25(OH)D) levels were associated with increased risk of PAD in the Korean population. This cross-sectional study was conducted among 8,960 subjects aged 50 years or older without known myocardial infarction or stroke. PAD was defined by an ankle brachial blood pressure index <0.9. Multivariate logistic regression was used to evaluate the association between serum 25(OH)D levels and risk of PAD. Of the 8,960 subjects, 3.0% had PAD and the age and sex adjusted prevalence of PAD decreased with the increasing 25(OH)D quartile. After adjusting for potential confounders and parathyroid hormones, serum 25(OH)D levels were associated with a significantly decreased risk of PAD (OR for one SD increase, 0.98; 95% CI, 0.95-1.0, P for trend=0.040). Compared with the first 25(OH)D quartile, the odds of PAD were 0.86 (95% CI, 0.62-1.21), 0.67 (95% CI, 0.46-0.97), and 0.71 (95% CI, 0.49-1.04) for the second, third, and fourth quartiles, respectively. In this cross-sectional study, we found that low serum 25(OH)D levels were associated with an increased risk of PAD, independent of traditional cardiovascular risk factors and parathyroid hormone. Our findings suggest that low vitamin D levels may contribute to PAD in the Korean population.
MeSH Terms
Figure
Reference
-
1. Chua GT, Chan YC, Cheng SW. Vitamin D status and peripheral arterial disease: evidence so far. Vasc Health Risk Manag. 2011; 7:671–675.2. Kim J. Association between serum vitamin D, parathyroid hormone and metabolic syndrome in middle-aged and older Korean adults. Eur J Clin Nutr. 2015; 69:425–430.
Article3. Liew JY, Sasha SR, Ngu PJ, Warren JL, Wark J, Dart AM, et al. Circulating vitamin D levels are associated with the presence and severity of coronary artery disease but not peripheral arterial disease in patients undergoing coronary angiography. Nutr Metab Cardiovasc Dis. 2015; 25:274–279.
Article4. Joo NS, Dawson-Hughes B, Yeum KJ. 25-Hydroxyvitamin D, calcium intake, and bone mineral content in adolescents and young adults: analysis of the fourth and fifth Korea National Health and Nutrition Examination Survey (KNHANES IV-2, 3, 2008-2009 and V-1, 2010). J Clin Endocrinol Metab. 2013; 98:3627–3636.
Article5. Joo NS, Dawson-Hughes B, Kim YS, Oh K, Yeum KJ. Impact of calcium and vitamin D insufficiencies on serum parathyroid hormone and bone mineral density: analysis of the fourth and fifth Korea National Health and Nutrition Examination Survey (KNHANES IV-3, 2009 and KNHANES V-1, 2010). J Bone Miner Res. 2013; 28:764–770.
Article6. May HT, Bair TL, Lappé DL, Anderson JL, Horne BD, Carlquist JF, et al. Association of vitamin D levels with incident depression among a general cardiovascular population. Am Heart J. 2010; 159:1037–1043.
Article7. Barnard K, Colón-Emeric C. Extraskeletal effects of vitamin D in older adults: cardiovascular disease, mortality, mood, and cognition. Am J Geriatr Pharmacother. 2010; 8:4–33.
Article8. Makariou S, Liberopoulos EN, Elisaf M, Challa A. Novel roles of vitamin D in disease: what is new in 2011? Eur J Intern Med. 2011; 22:355–362.
Article9. Rosen CJ. Clinical practice. Vitamin D insufficiency. N Engl J Med. 2011; 364:248–254.10. Reis JP, von Mühlen D, Michos ED, Miller ER 3rd, Appel LJ, Araneta MR, et al. Serum vitamin D, parathyroid hormone levels, and carotid atherosclerosis. Atherosclerosis. 2009; 207:585–590.
Article11. Aronow WS. Peripheral arterial disease in the elderly. Clin Interv Aging. 2007; 2:645–654.
Article12. Kim DH, Sabour S, Sagar UN, Adams S, Whellan DJ. Prevalence of hypovitaminosis D in cardiovascular diseases (from the National Health and Nutrition Examination Survey 2001 to 2004). Am J Cardiol. 2008; 102:1540–1544.
Article13. Melamed ML, Muntner P, Michos ED, Uribarri J, Weber C, Sharma J, et al. Serum 25-hydroxyvitamin D levels and the prevalence of peripheral arterial disease: results from NHANES 2001 to 2004. Arterioscler Thromb Vasc Biol. 2008; 28:1179–1185.
Article14. van de Luijtgaarden KM, Voûte MT, Hoeks SE, Bakker EJ, Chonchol M, Stolker RJ, et al. Vitamin D deficiency may be an independent risk factor for arterial disease. Eur J Vasc Endovasc Surg. 2012; 44:301–306.
Article15. Reis JP, Michos ED, von Mühlen D, Miller ER 3rd. Differences in vitamin D status as a possible contributor to the racial disparity in peripheral arterial disease. Am J Clin Nutr. 2008; 88:1469–1477.
Article16. Amer M, Narotsky DL, Qayyum R. 25-Hydroxyvitamin D and ankle-brachial blood pressure index in adults without peripheral artery disease. Clin Transl Sci. 2014; 7:391–395.
Article17. McDermott MM, Liu K, Ferrucci L, Tian L, Guralnik J, Kopp P, et al. Vitamin D status, functional decline, and mortality in peripheral artery disease. Vasc Med. 2014; 19:18–26.
Article18. Veronese N, De Rui M, Bolzetta F, Toffanello ED, Coin A, Zambon S, et al. Serum 25-hydroxyvitamin D and the incidence of peripheral artery disease in the elderly: yhe Pro.V.A study. J Atheroscler Thromb. 2015; 22:726–734.
Article19. Nsengiyumva V, Fernando ME, Moxon JV, Krishna SM, Pinchbeck J, Omer SM, et al. The association of circulating 25-hydroxyvitamin D concentration with peripheral arterial disease: a meta-analysis of observational studies. Atherosclerosis. 2015; 243:645–651.
Article20. Choi EY. 25(OH)D status and demographic and lifestyle determinants of 25(OH)D among Korean adults. Asia Pac J Clin Nutr. 2012; 21:526–535.21. Kweon SS, Shin MH, Jeong SK, Nam HS, Lee YH, Park KS, et al. Cohort Profile: The Namwon Study and the Dong-gu Study. Int J Epidemiol. 2014; 43:558–567.
Article22. Tomiyama H, Yamashina A, Arai T, Hirose K, Koji Y, Chikamori T, et al. Influences of age and gender on results of noninvasive brachial-ankle pulse wave velocity measurement--a survey of 12517 subjects. Atherosclerosis. 2003; 166:303–309.
Article23. Forman JP, Giovannucci E, Holmes MD, Bischoff-Ferrari HA, Tworoger SS, Willett WC, et al. Plasma 25-hydroxyvitamin D levels and risk of incident hypertension. Hypertension. 2007; 49:1063–1069.
Article24. Vaidya A, Williams JS. The relationship between vitamin D and the renin-angiotensin system in the pathophysiology of hypertension, kidney disease, and diabetes. Metabolism. 2012; 61:450–458.
Article25. Zagura M, Serg M, Kampus P, Zilmer M, Eha J, Unt E, et al. Aortic stiffness and vitamin D are independent markers of aortic calcification in patients with peripheral arterial disease and in healthy subjects. Eur J Vasc Endovasc Surg. 2011; 42:689–695.
Article26. Wikström J, Hansen T, Johansson L, Lind L, Ahlström H. Ankle brachial index <0.9 underestimates the prevalence of peripheral artery occlusive disease assessed with whole-body magnetic resonance angiography in the elderly. Acta Radiol. 2008; 49:143–149.
Article27. Moyer VA. U.S. Preventive Services Task Force. Screening for peripheral artery disease and cardiovascular disease risk assessment with the ankle-brachial index in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013; 159:342–348.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intermittent Claudication in Peripheral Arterial Disease
- Vitamin D status and its association with cardiometabolic risk factors in Korean adults based on a 2008-2010 Korean National Health and Nutrition Examination Survey
- Epidemiology of Peripheral Arterial Diseases in Individuals with Diabetes Mellitus
- Premature Peripheral Arterial Disease with the 5th Toe Necrotizing Lesion after Workout: A Case Report
- A clinical study of peripheral arterial disease