Comparison of Second and Third Editions of the Bayley Scales in Children With Suspected Developmental Delay
- Affiliations
-
- 1Department of Rehabilitation Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 2Department of Physical Medicine and Rehabilitation, Division of Pediatric Rehabilitation Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. iysung56@gmail.com
- KMID: 2432202
- DOI: http://doi.org/10.5535/arm.2018.42.2.313
Abstract
OBJECTIVE
To compare the scores of the Bayley Scales of Infant Development second edition (BSID-II) and the third edition, Bayley-III, in children with suspected developmental delay and to determine the cutoff score for developmental delay in the Bayley-III.
METHODS
Children younger than 42 months (n=62) with suspected developmental delay who visited our department between 2014 and 2015 were assessed with both the BSID-II and Bayley-III tests.
RESULTS
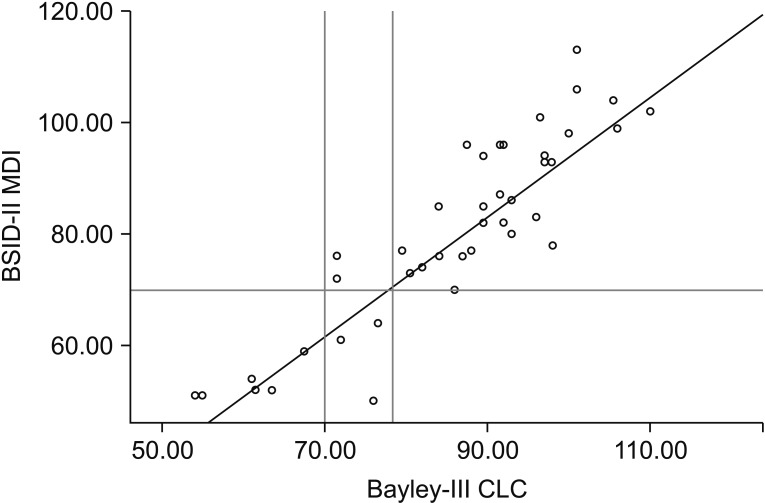
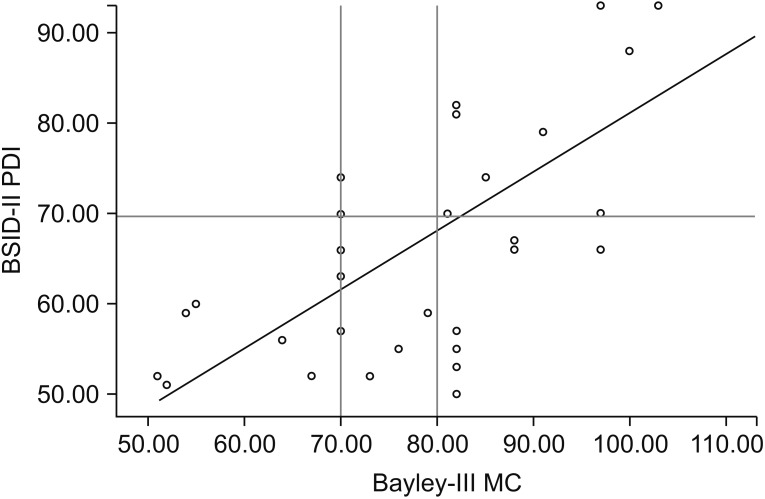
The mean Bayley-III Cognitive Language Composite (CLC) score was 5.8 points higher than the mean BSID-II Mental Developmental Index (MDI) score, and the mean Bayley-III Motor Composite (MC) score was 7.9 points higher than the mean BSID-II Psychomotor Developmental Index (PDI) score. In receiver operating characteristic (ROC) analysis of a BSID-II MDI score < 70, Bayley-III CLC scores showed a cutoff of 78.0 (96.6% sensitivity and 93.9% specificity). In ROC analysis of a BSID-II PDI score < 70, the Bayley-III MC score showed a cutoff of 80.
CONCLUSION
There was a strong correlation between the BSID-II and Bayley-III in children with suspected developmental delay. The Bayley-III identified fewer children with developmental delay. The recommended cutoff value for developmental delay increased from a BSID-II score of 70 to a Bayley-III CLC score of 78 and Bayley-III MC score of 80.
Keyword
Figure
Cited by 3 articles
-
The Predictive Value of Language Scales: Bayley Scales of Infant and Toddler Development Third Edition in Correlation With Korean Sequenced Language Scale for Infant
Joung Hyun Doh, Soo A Kim, Kiyoung Oh, Yuntae Kim, Nodam Park, Siha Park, Nam Hun Heo
Ann Rehabil Med. 2020;44(5):378-385. doi: 10.5535/arm.19198.Neurodevelopmental Outcomes and Brain Volumetric Analysis of Low-Grade Intraventricular Hemorrhage
Seul Gi Park, Hyo Ju Yang, Soo Yeon Lim, Seh Hyun Kim, Seung Han Shin, Ee-Kyung Kim, Han-Suk Kim
Neonatal Med. 2023;30(2):42-48. doi: 10.5385/nm.2023.30.2.42.Antenatal Magnesium Sulfate Is Not Associated With Improved Long-Term Neurodevelopment and Growth in Very Low Birth Weight Infants
Ga Won Jeon, So Yoon Ahn, Su Min Kim, Misun Yang, Se In Sung, Ji-Hee Sung, Soo-young Oh, Cheong-Rae Roh, Suk-Joo Choi, Yun Sil Chang
J Korean Med Sci. 2023;38(44):e350. doi: 10.3346/jkms.2023.38.e350.
Reference
-
1. Lindsey JC, Brouwers P. Intrapolation and extrapolation of age-equivalent scores for the Bayley II: a comparison of two methods of estimation. Clin Neuropharmacol. 1999; 22:44–53. PMID: 10047934.2. Johnson S, Marlow N. Developmental screen or developmental testing? Early Hum Dev. 2006; 82:173–183. PMID: 16504424.
Article3. Acton BV, Biggs WS, Creighton DE, Penner KA, Switzer HN, Thomas JH, et al. Overestimating neurodevelopment using the Bayley-III after early complex cardiac surgery. Pediatrics. 2011; 128:e794–e800. PMID: 21949148.
Article4. Anderson PJ, De Luca CR, Hutchinson E, Roberts G, Doyle LW. Victorian Infant Collaborative Group. Underestimation of developmental delay by the new Bayley-III Scale. Arch Pediatr Adolesc Med. 2010; 164:352–356. PMID: 20368488.
Article5. Bayley N. Bayley scales of infant and toddler development. 3rd ed. San Antonio: Pearson;2006.6. Hilden J. The area under the ROC curve and its competitors. Med Decis Making. 1991; 11:95–101. PMID: 1865785.
Article7. Vohr BR, Stephens BE, Higgins RD, Bann CM, Hintz SR, Das A, et al. Are outcomes of extremely preterm infants improving? Impact of Bayley assessment on outcomes. J Pediatr. 2012; 161:222–228. PMID: 22421261.
Article8. Reuner G, Fields AC, Wittke A, Lopprich M, Pietz J. Comparison of the developmental tests Bayley-III and Bayley-II in 7-month-old infants born preterm. Eur J Pediatr. 2013; 172:393–400. PMID: 23224346.
Article9. Moore T, Johnson S, Haider S, Hennessy E, Marlow N. Relationship between test scores using the second and third editions of the Bayley Scales in extremely preterm children. J Pediatr. 2012; 160:553–558. PMID: 22048046.
Article10. Silveira RC, Filipouski GR, Goldstein DJ, O'Shea TM, Procianoy RS. Agreement between Bayley Scales second and third edition assessments of very low-birth-weight infants. Arch Pediatr Adolesc Med. 2012; 166:1075–1076. PMID: 23007841.
Article11. Jary S, Whitelaw A, Walloe L, Thoresen M. Comparison of Bayley-2 and Bayley-3 scores at 18 months in term infants following neonatal encephalopathy and therapeutic hypothermia. Dev Med Child Neurol. 2013; 55:1053–1059. PMID: 23927586.12. Trahan LH, Stuebing KK, Fletcher JM, Hiscock M. The Flynn effect: a meta-analysis. Psychol Bull. 2014; 140:1332–1360. PMID: 24979188.
Article13. Lowe JR, Erickson SJ, Schrader R, Duncan AF. Comparison of the Bayley II Mental Developmental Index and the Bayley III Cognitive Scale: are we measuring the same thing? Acta Paediatr. 2012; 101:e55–e58. PMID: 22054168.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Assessment of Children with Developmental Delay: Korean-Ages & Stages Questionnaires(K-ASQ) and Bayley Scales of Infant Development test II(BSID-II)
- Assessment of children with developmental delay: Korean infant and child development test (KICDT) and Korean Bayley scale of infant development-II (K-BSID-II)
- Language Development of Non-handicapped Low Birth Weight Infants
- Visual Evoked Potential in Children With Developmental Disorders: Correlation With Neurodevelopmental Outcomes
- Relationship of Perinatal Risk Factors and Neonatal Complications with Bayley Scales in Asphyxiated Newborns