Korean Circ J.
2019 Feb;49(2):183-191. 10.4070/kcj.2018.0214.
Infliximab Treatment for Intravenous Immunoglobulin-resistant Kawasaki Disease: a Multicenter Study in Korea
- Affiliations
-
- 1Department of Pediatrics, Inje University, Haeundae Paik Hospital, Busan, Korea. msped@hanmail.net
- 2Department of Pediatrics, Ewha Womans University, Mokdong Hospital, Seoul, Korea.
- 3Department of Pediatrics, Busan National University, Children's Hospital, Busan, Korea.
- 4Department of Pediatrics, Seoul National University, Children's Hospital, Seoul, Korea.
- 5Department of Pediatrics, Chonnam National University, Children's Hospital, Gwangju, Korea.
- 6Department of Pediatrics, Kyung Hee University Hospital at Gangdong, Seoul, Korea.
- 7Department of Pediatrics, Chonbuk National University Medical School, Children's Hospital, Cheonju, Korea.
- 8Department of Pediatrics, Kyungpook National University, School of Medicine, Daegu, Korea.
- 9Department of Pediatrics, Inje University, Busan Paik Hospital, Busan, Korea.
- KMID: 2432137
- DOI: http://doi.org/10.4070/kcj.2018.0214
Abstract
- BACKGROUND AND OBJECTIVES
We investigated the status of infliximab use in intravenous immunoglobulin (IVIG)-resistant Kawasaki disease (KD) patients and the incidence of coronary artery aneurysms (CAAs) according to treatment regimens.
METHODS
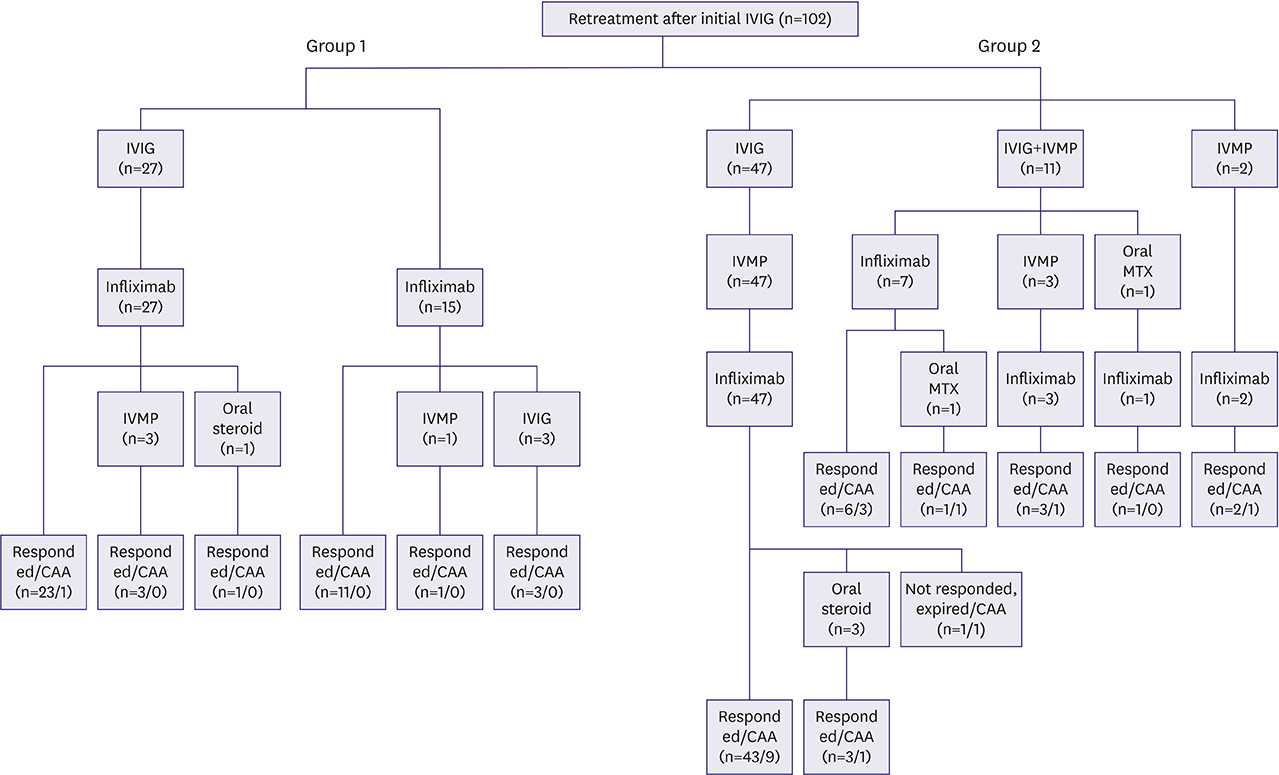
Between March 2010 and February 2017, 16 hospitals participated in this study. A total of 102 (32.3±19.9 months, 72 males) who received infliximab at any time after first IVIG treatment failure were enrolled. Data were retrospectively collected using a questionnaire.
RESULTS
Subjects were divided into two groups according to the timing of infliximab administration. Early treatment (group 1) had shorter fever duration (10.5±4.4 days) until infliximab infusion than that in late treatment (group 2) (16.4±4.5 days; p < 0.001). We investigated the response rate to infliximab and the incidence of significant CAA (z-score >5). Overall response rate to infliximab was 89/102 (87.3%) and the incidence of significant CAA was lower in group 1 than in group 2 (1/42 [2.4%] vs. 17/60 [28.3%], p < 0.001).
CONCLUSIONS
This study suggests that the early administration of infliximab may reduce the incidence of significant CAA in patients with IVIG-resistant KD. However, further prospective randomized studies with larger sample sizes are required.
MeSH Terms
Figure
Cited by 1 articles
-
Infliximab, Is It Really a New Horizon for the Treatment of Kawasaki Disease?
Lucy Youngmin Eun
Korean Circ J. 2019;49(2):192-193. doi: 10.4070/kcj.2018.0460.
Reference
-
1. McCrindle BW, Rowley AH, Newburger JW, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation. 2017; 135:e927–e929.
Article2. Burns JC, Capparelli EV, Brown JA, Newburger JW, Glode MP. US/Canadian Kawasaki Syndrome Study Group. Intravenous gamma-globulin treatment and retreatment in Kawasaki disease. Pediatr Infect Dis J. 1998; 17:1144–1148.
Article3. Wallace CA, French JW, Kahn SJ, Sherry DD. Initial intravenous gammaglobulin treatment failure in Kawasaki disease. Pediatrics. 2000; 105:E78.
Article4. Song MS, Lee SB, Sohn S, et al. Infliximab treatment for refractory Kawasaki disease in Korean children. Korean Circ J. 2010; 40:334–338.
Article5. Burns JC, Mason WH, Hauger SB, et al. Infliximab treatment for refractory Kawasaki syndrome. J Pediatr. 2005; 146:662–667.
Article6. Tremoulet AH, Jain S, Jaggi P, et al. Infliximab for intensification of primary therapy for Kawasaki disease: a phase 3 randomised, double-blind, placebo-controlled trial. Lancet. 2014; 383:1731–1738.
Article7. Olivieri L, Arling B, Friberg M, Sable C. The calculation of z-score for coronary artery measurements were accomplished using the z-score calculator. J Am Soc Echocardiogr. 2009; 22:159–164.8. Friedman KG, Gauvreau K, Hamaoka-Okamoto A, et al. Coronary artery aneurysms in Kawasaki disease: risk factors for progressive disease and adverse cardiac events in the US population. J Am Heart Assoc. 2016; 5:e003289.
Article9. Kato H, Koike S, Yokoyama T. Kawasaki disease: effect of treatment on coronary artery involvement. Pediatrics. 1979; 63:175–179.10. Wright DA, Newburger JW, Baker A, Sundel RP. Treatment of immune globulin-resistant Kawasaki disease with pulsed doses of corticosteroids. J Pediatr. 1996; 128:146–149.
Article11. Wardle AJ, Connolly GM, Seager MJ, Tulloh RM. Corticosteroids for the treatment of Kawasaki disease in children. Cochrane Database Syst Rev. 2017; 1:CD011188.
Article12. Miura M, Ohki H, Yoshiba S, et al. Adverse effects of methylprednisolone pulse therapy in refractory Kawasaki disease. Arch Dis Child. 2005; 90:1096–1097.
Article13. Azmoon S, Atkinson D, Budoff MJ. Refractory progression of coronary aneurysms, a case of delayed onset Kawasaki disease as depicted by cardiac computed tomography angiography. Congenit Heart Dis. 2010; 5:321–326.
Article14. Sivakumar K, Pavithran S. Extensive coronary aneurysms with thrombosis in resistant Kawasaki disease. Pediatr Cardiol. 2013; 34:444–446.
Article15. Lee J, Kim GB, Kwon BS, Bae EJ, Noh CI. Two cases of super-giant coronary aneurysms after Kawasaki disease. Korean Circ J. 2014; 44:54–58.
Article16. Micallef ES, Attard MS, Grech V. A case of atypical Kawasaki disease with giant coronary artery aneurysm containing thrombus. Images Paediatr Cardiol. 2016; 18:9–15.17. Kibata T, Suzuki Y, Hasegawa S, et al. Coronary artery lesions and the increasing incidence of Kawasaki disease resistant to initial immunoglobulin. Int J Cardiol. 2016; 214:209–215.
Article18. Hyams JS, Dubinsky MC, Baldassano RN, et al. Infliximab is not associated with increased risk of malignancy or hemophagocytic lymphohistiocytosis in pediatric patients with inflammatory bowel disease. Gastroenterology. 2017; 152:1901–1914.e3.
Article19. Son MB, Gauvreau K, Burns JC, et al. Infliximab for intravenous immunoglobulin resistance in Kawasaki disease: a retrospective study. J Pediatr. 2011; 158:644–649.e1.
Article20. Youn Y, Kim J, Hong YM, Sohn S. Infliximab as the first retreatment in patients with Kawasaki disease resistant to initial intravenous immunoglobulin. Pediatr Infect Dis J. 2016; 35:457–459.
Article21. Mori M, Hara T, Kikuchi M, et al. Infliximab versus intravenous immunoglobulin for refractory Kawasaki disease: a phase 3, randomized, open-label, active-controlled, parallel-group, multicenter trial. Sci Rep. 2018; 8:1994.
Article22. Furukawa T, Kishiro M, Akimoto K, Nagata S, Shimizu T, Yamashiro Y. Effects of steroid pulse therapy on immunoglobulin-resistant Kawasaki disease. Arch Dis Child. 2008; 93:142–146.
Article23. Crandall WV, Mackner LM. Infusion reactions to infliximab in children and adolescents: frequency, outcome and a predictive model. Aliment Pharmacol Ther. 2003; 17:75–84.
Article24. Keane J, Gershon S, Wise RP, et al. Tuberculosis associated with infliximab, a tumor necrosis factor alpha-neutralizing agent. N Engl J Med. 2001; 345:1098–1104.25. Minozzi S, Bonovas S, Lytras T, et al. Risk of infections using anti-TNF agents in rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis: a systematic review and meta-analysis. Expert Opin Drug Saf. 2016; 15:11–34.
Article26. Jang H, Kim KY, Kim DS. Clinical outcomes of low-dose methotrexate therapy as a second-line drug for intravenous immunoglobulin-resistant Kawasaki disease. Yonsei Med J. 2018; 59:113–118.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Predictors and management of intravenous immunoglobulin-resistant Kawasaki disease
- History and Future of Treatment for Acute Stage Kawasaki Disease
- Infliximab treatment for a patient with refractory Kawasaki disease
- Gram-negative Septicemia after Infliximab Treatment in an Infant with Refractory Kawasaki Disease
- Efficacy of Dexamethasone Therapy for Coronary Lesion after Immunoglobulin-retreated Kawasaki Disease