J Korean Med Assoc.
2019 Jan;62(1):37-46. 10.5124/jkma.2019.62.1.37.
Updated treatment guideline of chronic spontaneous urticaria
- Affiliations
-
- 1Department of Dermatology, Gil Medical Center, Gachon University School of Medicine, Incheon, Korea. jyroh1@gilhospital.com
- KMID: 2431993
- DOI: http://doi.org/10.5124/jkma.2019.62.1.37
Abstract
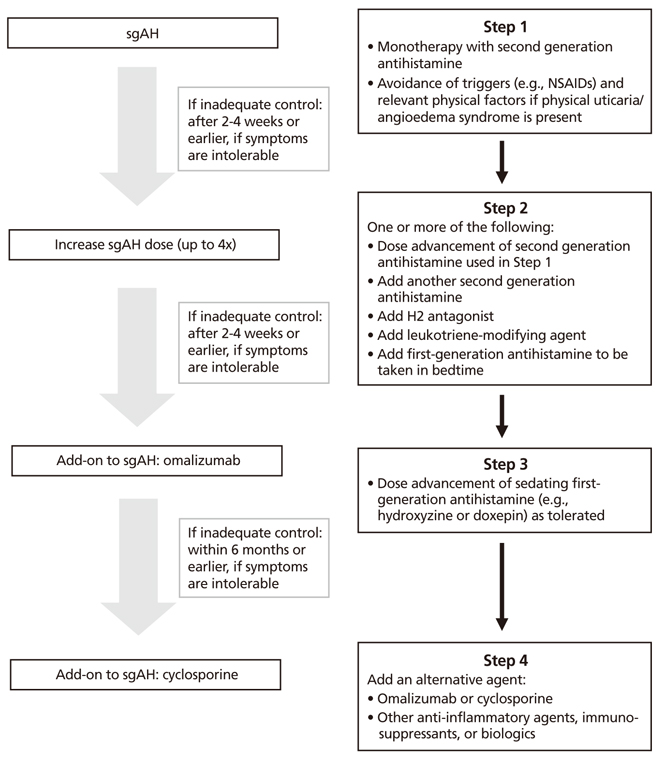
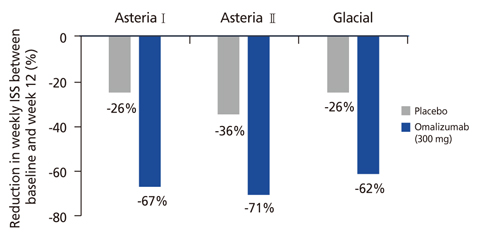
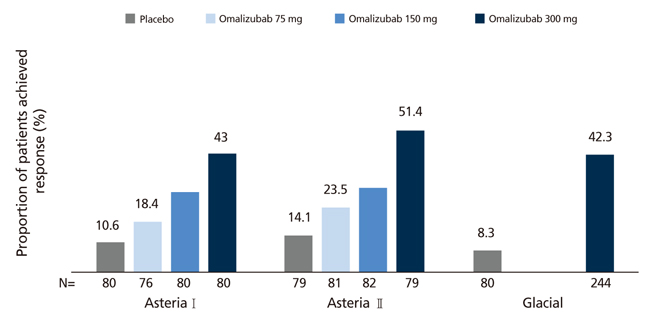
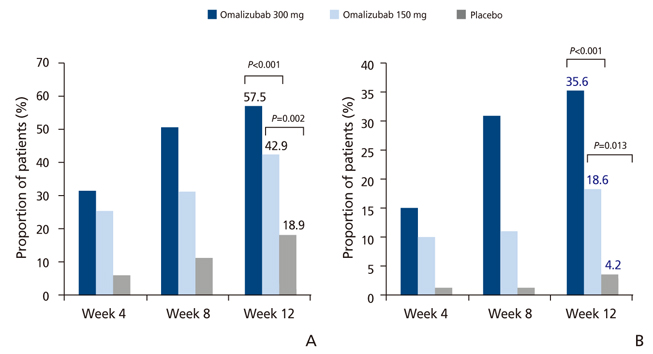
- Chronic spontaneous urticaria (CSU), also known as chronic idiopathic urticaria, is a common chronic inflammatory skin disorder that has a prevalence of 0.5% to 1% in the general population. It affects daily normal life and work productivity, with significant impacts on quality of life. Generally, the management of CSU uses a step-wise approach. Although second-generation H1 antihistamines are an effective mainstay of CSU, approximately 20% of patients are resistant to conventional antihistamine monotherapy. Evidence-based and expert consensus-based treatment guidelines of CSU can be a useful resource for primary care physicians and specialists. This review presents diverse information to support decision-making for individualized treatment plans in this special population. Several major therapeutic advances have occurred in recent years. Omalizumab, an immunoglobulin G humanized monoclonal anti-immunoglobulin E antibody that prevents binding of immunoglobulin E to the high-affinity immunoglobulin E receptor has shown safety and efficacy in patients with intractable CSU. In well-controlled clinical trials in patients with refractory CSU who received add-on therapy with subcutaneous omalizumab (300 mg every 4 weeks for 12 or 24 weeks), the rates of complete response were significantly higher in the omalizumab group (relative risk, 4.55; P < 0.0001). The introduction of omalizumab as an add-on therapy to H1 antihistamines as a management option has markedly improved the therapeutic possibilities for CSU and the quality of life of CSU patients. Nevertheless, many patients still do not tolerate or benefit from existing therapies, including omalizumab. There are ongoing studies investigating the treatment potential of novel therapeutic targets in CSU.
Keyword
MeSH Terms
Figure
Reference
-
1. Zuberbier T, Aberer W, Asero R, Abdul Latiff AH, Baker D, Ballmer-Weber B, Bernstein JA, Bindslev-Jensen C, Brzoza Z, Buense Bedrikow R, Canonica GW, Church MK, Craig T, Danilycheva IV, Dressler C, Ensina LF, Gimenez-Arnau A, Godse K, Gonçalo M, Grattan C, Hebert J, Hide M, Kaplan A, Kapp A, Katelaris CH, Kocaturk E, Kulthanan K, Larenas-Linnemann D, Leslie TA, Magerl M, Mathelier-Fusade P, Meshkova RY, Metz M, Nast A, Nettis E, Oude-Elberink H, Rosumeck S, Saini SS, Sanchez-Borges M, Schmid-Grendelmeier P, Staubach P, Sussman G, Toubi E, Vena GA, Vestergaard C, Wedi B, Werner RN, Zhao Z, Maurer M. Endorsed by the following societies: AAAAI, AAD, AAIITO, ACAAI, AEDV, APAAACI, ASBAI, ASCIA, BAD, BSACI, CDA, CMICA, CSACI, DDG, DDS, DGAKI, DSA, DST, EAACI, EIAS, EDF, EMBRN, ESCD, GA2LEN, IAACI, IADVL, JDA, NVvA, MSAI, ÖGDV, PSA, RAACI, SBD, SFD, SGAI, SGDV, SIAAIC, SIDeMaST, SPDV, TSD, UNBB, UNEV and WAO. The EAACI/GA2LEN/EDF/WAO guideline for the definition, classification, diagnosis and management of urticaria. Allergy. 2018; 73:1393–1414.
Article2. Lee N, Lee JD, Lee HY, Kang DR, Ye YM. Epidemiology of chronic urticaria in Korea using the Korean health insurance database, 2010–2014. Allergy Asthma Immunol Res. 2017; 9:438–445.
Article3. Kim YS, Park SH, Han K, Bang CH, Lee JH, Park YM. Prevalence and incidence of chronic spontaneous urticaria in the entire Korean adult population. Br J Dermatol. 2018; 178:976–977.
Article4. Lee SJ, Ha EK, Jee HM, Lee KS, Lee SW, Kim MA, Kim DH, Jung YH, Sheen YH, Sung MS, Han MY. Prevalence and risk factors of urticaria with a focus on chronic urticaria in children. Allergy Asthma Immunol Res. 2017; 9:212–219.
Article5. Kim YS, Park SH, Han K, Lee JH, Kim NI, Roh JY, Seo SJ, Song HJ, Lee MG, Choi JH, Park YM. Clinical course of chronic spontaneous urticaria in the Korean adult population. Allergy Asthma Immunol Res. 2018; 10:83–87.
Article6. Jacques P, Lavoie A, Bédard PM, Brunet C, Hebert J. Chronic idiopathic urticaria: profiles of skin mast cell histamine release during active disease and remission. J Allergy Clin Immunol. 1992; 89:1139–1143.
Article7. Chang TW, Chen C, Lin CJ, Metz M, Church MK, Maurer M. The potential pharmacologic mechanisms of omalizumab in patients with chronic spontaneous urticaria. J Allergy Clin Immunol. 2015; 135:337–342.
Article8. Kowalski ML, Woessner K, Sanak M. Approaches to the diagnosis and management of patients with a history of nonsteroidal anti-inflammatory drug-related urticaria and angioedema. J Allergy Clin Immunol. 2015; 136:245–251.
Article9. Shakouri A, Compalati E, Lang DM, Khan DA. Effectiveness of Helicobacter pylori eradication in chronic urticaria: evidence-based analysis using the Grading of Recommendations Assessment, Development, and Evaluation system. Curr Opin Allergy Clin Immunol. 2010; 10:362–369.
Article10. Varghese R, Rajappa M, Chandrashekar L, Kattimani S, Archana M, Munisamy M, Revathy G, Thappa DM. Association among stress, hypocortisolism, systemic inflammation, and disease severity in chronic urticaria. Ann Allergy Asthma Immunol. 2016; 116:344–348.
Article11. Grattan CE, Francis DM, Slater NG, Barlow RJ, Greaves MW. Plasmapheresis for severe, unremitting, chronic urticaria. Lancet. 1992; 339:1078–1080.
Article12. Wagner N, Dirk D, Peveling-Oberhag A, Reese I, Rady-Pizarro U, Mitzel H, Staubach P. A popular myth: low-histamine diet improves chronic spontaneous urticaria. Fact or fiction? J Eur Acad Dermatol Venereol. 2017; 31:650–655.
Article13. Curto-Barredo L, Silvestre JF, Gimenez-Arnau AM. Update on the treatment of chronic urticaria. Actas Dermosifiliogr. 2014; 105:469–482.
Article14. Bernstein JA, Lang DM, Khan DA, Craig T, Dreyfus D, Hsieh F, Sheikh J, Weldon D, Zuraw B, Bernstein DI, Blessing-Moore J, Cox L, Nicklas RA, Oppenheimer J, Portnoy JM, Randolph CR, Schuller DE, Spector SL, Tilles SA, Wallace D. The diagnosis and management of acute and chronic urticaria: 2014 update. J Allergy Clin Immunol. 2014; 133:1270–1277.
Article15. Beck LA, Bernstein JA, Maurer M. A review of international recommendations for the diagnosis and management of chronic urticaria. Acta Derm Venereol. 2017; 97:149–158.
Article16. Kapp A, Pichler WJ. Levocetirizine is an effective treatment in patients suffering from chronic idiopathic urticaria: a randomized, double-blind, placebo-controlled, parallel, multicenter study. Int J Dermatol. 2006; 45:469–474.
Article17. Grob JJ, Auquier P, Dreyfus I, Ortonne JP. How to prescribe antihistamines for chronic idiopathic urticaria: desloratadine daily vs PRN and quality of life. Allergy. 2009; 64:605–612.
Article18. Guillen-Aguinaga S, Jauregui Presa I, Aguinaga-Ontoso E, Guillen-Grima F, Ferrer M. Updosing nonsedating antihistamines in patients with chronic spontaneous urticaria: a systematic review and meta-analysis. Br J Dermatol. 2016; 175:1153–1165.
Article19. Simons FE, Sussman GL, Simons KJ. Effect of the H2-antagonist cimetidine on the pharmacokinetics and pharmacodynamics of the H1-antagonists hydroxyzine and cetirizine in patients with chronic urticaria. J Allergy Clin Immunol. 1995; 95:685–693.
Article20. Broder MS, Raimundo K, Antonova E, Chang E. Resource use and costs in an insured population of patients with chronic idiopathic/spontaneous urticaria. Am J Clin Dermatol. 2015; 16:313–321.
Article21. Asero R, Tedeschi A. Usefulness of a short course of oral prednisone in antihistamine-resistant chronic urticaria: a retrospective analysis. J Investig Allergol Clin Immunol. 2010; 20:386–390.22. Kim S, Baek S, Shin B, Yoon SY, Park SY, Lee T, Lee YS, Bae YJ, Kwon HS, Cho YS, Moon HB, Kim TB. Influence of initial treatment modality on long-term control of chronic idiopathic urticaria. PLoS One. 2013; 8:e69345.
Article23. de Silva NL, Damayanthi H, Rajapakse AC, Rodrigo C, Rajapakse S. Leukotriene receptor antagonists for chronic urticaria: a systematic review. Allergy Asthma Clin Immunol. 2014; 10:24.
Article24. Bagenstose SE, Levin L, Bernstein JA. The addition of zafirlukast to cetirizine improves the treatment of chronic urticaria in patients with positive autologous serum skin test results. J Allergy Clin Immunol. 2004; 113:134–140.
Article25. Vena GA, Cassano N, Colombo D, Peruzzi E, Pigatto P. Neo-I-30 Study Group. Cyclosporine in chronic idiopathic urticaria: a double-blind, randomized, placebo-controlled trial. J Am Acad Dermatol. 2006; 55:705–709.
Article26. Sagi L, Solomon M, Baum S, Lyakhovitsky A, Trau H, Barzilai A. Evidence for methotrexate as a useful treatment for steroid-dependent chronic urticaria. Acta Derm Venereol. 2011; 91:303–306.
Article27. Sharma VK, Singh S, Ramam M, Kumawat M, Kumar R. A randomized placebo-controlled double-blind pilot study of methotrexate in the treatment of H1 antihistamine-resistant chronic spontaneous urticaria. Indian J Dermatol Venereol Leprol. 2014; 80:122–128.
Article28. Zimmerman AB, Berger EM, Elmariah SB, Soter NA. The use of mycophenolate mofetil for the treatment of autoimmune and chronic idiopathic urticaria: experience in 19 patients. J Am Acad Dermatol. 2012; 66:767–770.
Article29. Bhanja DC, Ghoshal L, Das S, Das S, Roy AK. Azathioprine in autologous serum skin test positive chronic urticaria: a case-control study in a tertiary care hospital of eastern India. Indian Dermatol Online J. 2015; 6:185–188.
Article30. Asero R. Oral cyclophosphamide in a case of cyclosporin and steroid-resistant chronic urticaria showing autoreactivity on autologous serum skin testing. Clin Exp Dermatol. 2005; 30:582–583.
Article31. Maurer M, Rosén K, Hsieh HJ, Saini S, Grattan C, Gimenez-Arnau A, Agarwal S, Doyle R, Canvin J, Kaplan A, Casale T. Omalizumab for the treatment of chronic idiopathic or spontaneous urticaria. N Engl J Med. 2013; 368:924–935.
Article32. Kaplan A, Ledford D, Ashby M, Canvin J, Zazzali JL, Conner E, Veith J, Kamath N, Staubach P, Jakob T, Stirling RG, Kuna P, Berger W, Maurer M, Rosen K. Omalizumab in patients with symptomatic chronic idiopathic/spontaneous urticaria despite standard combination therapy. J Allergy Clin Immunol. 2013; 132:101–109.
Article33. Kaplan A, Ferrer M, Bernstein JA, Antonova E, Trzaskoma B, Raimundo K, Rosen K, Omachi TA, Khalil S, Zazzali JL. Timing and duration of omalizumab response in patients with chronic idiopathic/spontaneous urticaria. J Allergy Clin Immunol. 2016; 137:474–481.
Article34. Hide M, Park HS, Igarashi A, Ye YM, Kim TB, Yagami A, Roh J, Lee JH, Chinuki Y, Youn SW, Lee SK, Inomata N, Choi JH, Fukunaga A, Wang J, Matsushima S, Greenberg S, Khalil S. Efficacy and safety of omalizumab in Japanese and Korean patients with refractory chronic spontaneous urticaria. J Dermatol Sci. 2017; 87:70–78.
Article35. Tharp MD, Bernstein JA, Kavati A, Ortiz B, MacDonald K, Denhaerynck K, Abraham I, Lee CS. Benefits and harms of omalizumab treatment in adolescent and adult patients with chronic idiopathic (spontaneous) urticaria: a meta-analysis of “real-world” evidence. JAMA Dermatol. 2018; 11. 14. [Epub]. DOI: 10.1001/jamadermatol.2018.3447.36. Engin B, Ozdemir M. Prospective randomized non-blinded clinical trial on the use of dapsone plus antihistamine vs. antihistamine in patients with chronic idiopathic urticaria. J Eur Acad Dermatol Venereol. 2008; 22:481–486.
Article37. Orden RA, Timble H, Saini SS. Efficacy and safety of sulfasalazine in patients with chronic idiopathic urticaria. Ann Allergy Asthma Immunol. 2014; 112:64–70.
Article38. Marmor MF, Kellner U, Lai TY, Lyons JS, Mieler WF. American Academy of Ophthalmology. Revised recommendations on screening for chloroquine and hydroxychloroquine retinopathy. Ophthalmology. 2011; 118:415–422.
Article39. Pho LN, Eliason MJ, Regruto M, Hull CM, Powell DL. Treatment of chronic urticaria with colchicine. J Drugs Dermatol. 2011; 10:1423–1428.40. Engin B, Ozdemir M, Balevi A, Mevlitoglu I. Treatment of chronic urticaria with narrowband ultraviolet B phototherapy: a randomized controlled trial. Acta Derm Venereol. 2008; 88:247–251.41. Antia C, Baquerizo K, Korman A, Alikhan A, Bernstein JA. Urticaria: a comprehensive review: treatment of chronic urticaria, special populations, and disease outcomes. J Am Acad Dermatol. 2018; 79:617–633.42. Kar S, Krishnan A, Preetha K, Mohankar A. A review of antihistamines used during pregnancy. J Pharmacol Pharmacother. 2012; 3:105–108.43. Ventura MT, Cassano N, Romita P, Vestita M, Foti C, Vena GA. Management of chronic spontaneous urticaria in the elderly. Drugs Aging. 2015; 32:271–282.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment with biological products for chronic urticaria
- A Case Series Study of Eighty-Five Chronic Spontaneous Urticaria Patients Referred to a Tertiary Care Center
- Dermographism ( III ): Dermographism in Acute and Chronic Urticaria
- Omalizumab on Chronic Spontaneous Urticaria and Chronic Inducible Urticaria: A Real-World Study of Efficacy and Predictors of Treatment Outcome
- Management of chronic urticaria in Asia: 2010 AADV consensus guidelines