Korean J Orthod.
2019 Jan;49(1):59-69. 10.4041/kjod.2019.49.1.59.
Long-term stability after multidisciplinary treatment involving maxillary distraction osteogenesis, and sagittal split ramus osteotomy for unilateral cleft lip and palate with severe occlusal collapse and gingival recession: A case report
- Affiliations
-
- 1Orthodontic Science, Department of Oral Health Sciences, Graduate School of Medical and Dental Sciences, Tokyo Medical and Dental University, Tokyo, Japan. skokai.orts.paper@gmail.com
- 2Private Practice, Yokohama, Japan.
- 3Department of Oral and Maxillofacial Surgery, Yokohama City University Medical Center, Yokohama, Japan.
- 4Department of Plastic and Aesthetic Surgery, Kitasato University, School of Medicine, Kanagawa, Japan.
- KMID: 2431081
- DOI: http://doi.org/10.4041/kjod.2019.49.1.59
Abstract
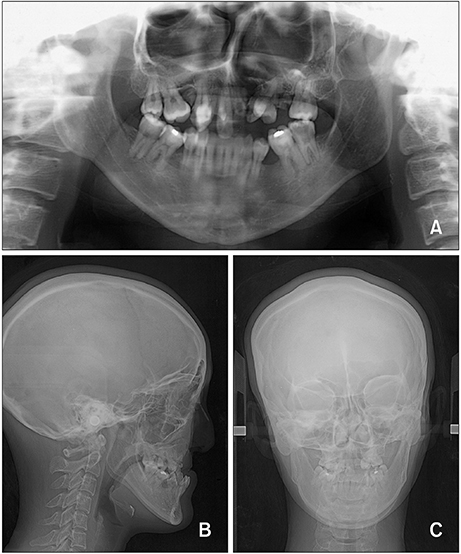
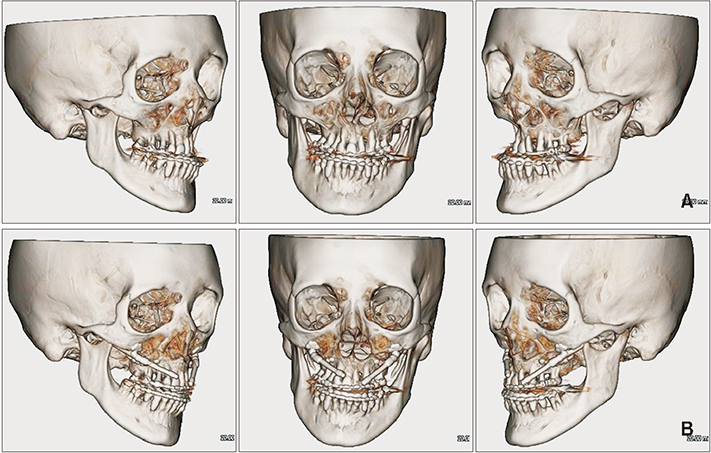
- In this report, we describe a case involving a 34-year-old woman who showed good treatment outcomes with long-term stability after multidisciplinary treatment for unilateral cleft lip and palate (CLP), maxillary hypoplasia, severe maxillary arch constriction, severe occlusal collapse, and gingival recession. A comprehensive treatment approach was developed with maximum consideration of strong scar constriction and gingival recession; it included minimum maxillary arch expansion, maxillary advancement by distraction osteogenesis using an internal distraction device, and mandibular setback using sagittal split ramus osteotomy. Her post-treatment records demonstrated a balanced facial profile and occlusion with improved facial symmetry. The patient's profile was dramatically improved, with reduced upper lip retrusion and lower lip protrusion as a result of the maxillary advancement and mandibular setback, respectively. Although gingival recession showed a slight increase, tooth mobility was within the normal physiological range. No tooth hyperesthesia was observed after treatment. There was negligible osseous relapse, and the occlusion remained stable after 5 years of post-treatment retention. Our findings suggest that such multidisciplinary approaches for the treatment of CLP with gingival recession and occlusal collapse help in improving occlusion and facial esthetics without the need for prostheses such as dental implants or bridges; in addition, the results show long-term post-treatment stability.
Keyword
MeSH Terms
Figure
Reference
-
1. Figueroa AA, Polley JW, Ko EW. Maxillary distraction for the management of cleft maxillary hypoplasia with a rigid external distraction system. Semin Orthod. 1999; 5:46–51.
Article2. Ross RB. Treatment variables affecting facial growth in complete unilateral cleft lip and palate. Cleft Palate J. 1987; 24:5–77.3. Yang CJ, Pan XG, Qian YF, Wang GM. Impact of rapid maxillary expansion in unilateral cleft lip and palate patients after secondary alveolar bone grafting: review and case report. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012; 114:e25–e30.
Article4. Akcam MO, Evirgen S, Uslu O, Memikoğlu UT. Dental anomalies in individuals with cleft lip and/or palate. Eur J Orthod. 2010; 32:207–213.
Article5. Schultes G, Gaggl A, Kärcher H. Comparison of periodontal disease in patients with clefts of palate and patients with unilateral clefts of lip, palate, and alveolus. Cleft Palate Craniofac J. 1999; 36:322–327.
Article6. Rachmiel A, Aizenbud D, Peled M. Long-term results in maxillary deficiency using intraoral devices. Int J Oral Maxillofac Surg. 2005; 34:473–479.
Article7. Vasant MR, Menon S, Kannan S. Maxillary expansion in cleft lip and palate using quad helix and rapid palatal expansion screw. Med J Armed Forces India. 2009; 65:150–153.
Article8. Vanarsdall RL, Secchi AG. Periodontal-orthodontics interrelationships. In : Graber TM, Vanarsdall RL, editors. Orthodontics, current principles and techniques. 5th ed. St. Louis: Mosby;2012. p. 807–841.9. Iannetti G, Cascone P, Saltarel A, Ettaro G. Le Fort I in cleft patients: 20 years' experience. J Craniofac Surg. 2004; 15:662–669.
Article10. Welch TB. Stability in the correction of dentofacial deformities: a comprehensive review. J Oral Maxillofac Surg. 1989; 47:1142–1149.
Article11. Figueroa AA, Polley JW. Management of severe cleft maxillary deficiency with distraction osteogenesis: procedures and results. Am J Orthod Dentofacial Orthop. 1999; 115:1–12.
Article12. Kessler P, Wiltfang J, Schultze-Mosgau S, Hirschfelder U, Neukam FW. Distraction osteogenesis of the maxilla and midface using a subcutaneous device: report of four cases. Br J Oral Maxillofac Surg. 2001; 39:13–21.
Article13. Mofid MM, Manson PN, Robertson BC, Tufaro AP, Elias JJ, Vander Kolk CA. Craniofacial distraction osteogenesis: a review of 3278 cases. Plast Reconstr Surg. 2001; 108:1103–1114.
Article14. Figueroa AA, Polley JW, Friede H, Ko EW. Long-term skeletal stability after maxillary advancement with distraction osteogenesis using a rigid external distraction device in cleft maxillary deformities. Plast Reconstr Surg. 2004; 114:1382–1392.
Article15. Scolozzi P. Distraction osteogenesis in the management of severe maxillary hypoplasia in cleft lip and palate patients. J Craniofac Surg. 2008; 19:1199–1214.
Article16. Tomita D, Omura S, Ozaki S, Shimazaki K, Fukuyama E, Tohnai I, et al. Maxillary movement in distraction osteogenesis using internal devices in cleft palate patients. Cleft Palate Craniofac J. 2011; 48:161–166.
Article17. Al-Gunaid T, Asahito T, Yamaki M, Hanada K, Takagi R, Ono K, et al. Relapse tendency in maxillary arch width in unilateral cleft lip and palate patients with different maxillary arch forms. Cleft Palate Craniofac J. 2008; 45:278–283.
Article18. Johal A, Katsaros C, Kiliaridis S, Leitao P, Rosa M, Sculean A, et al. State of the science on controversial topics: orthodontic therapy and gingival recession (a report of the Angle Society of Europe 2013 meeting). Prog Orthod. 2013; 11:14–16.
Article19. Bassarelli T, Dalstra M, Melsen B. Changes in clinical crown height as a result of transverse expansion of the maxilla in adults. Eur J Orthod. 2005; 27:121–128.
Article20. Chua HD, Hägg MB, Cheung LK. Cleft maxillary distraction versus orthognathic surgery-which one is more stable in 5 years? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 109:803–814.
Article21. Saltaji H, Major MP, Altalibi M, Youssef M, Flores-Mir C. Long-term skeletal stability after maxillary advancement with distraction osteogenesis in cleft lip and palate patients. Angle Orthod. 2012; 82:1115–1122.
Article22. Kumar A, Gabbay JS, Nikjoo R, Heller JB, O'Hara CM, Sisodia M, et al. Improved outcomes in cleft patients with severe maxillary deficiency after Le Fort I internal distraction. Plast Reconstr Surg. 2006; 117:1499–1509.
Article23. Gulsen A, Ozmen S, Tuncer S, Aslan BI, Kale S, Yavuzer R. Maxillary advancement with internal distraction device in cleft palate patients. J Craniofac Surg. 2007; 18:177–185.
Article24. Aikawa T, Iida S, Isomura ET, Namikawa M, Matsuoka Y, Yamada C, et al. Breakage of internal maxillary distractor: considerable complication of maxillary distraction osteogenesis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 106:e1–e7.
Article25. Bevilacqua RG, Ritoli EL, Kang C, Mabry K, Castiglione CL. Midmaxillary internal distraction osteogenesis: ideal surgery for the mature cleft patient. Plast Reconstr Surg. 2008; 121:1768–1778.
Article26. Nakagawa K, Ueki K, Takatsuka S, Marukawa K, Yamamoto E. A device for determining the position of intraoral distractors for protracting the maxilla. J Craniomaxillofac Surg. 2003; 31:234–237.
Article27. Lauwers F, Mayorca-Guiliani A, Lopez R, Woisard-Bassols V, Paoli JR, Boutault F. Maxillofacial intraoral distraction osteogenesis followed by elastic traction in cleft maxillary deformity. Int J Oral Maxillofac Surg. 2005; 34:85–88.
Article28. Van Sickels JE, Madsen MJ, Cunningham LL Jr, Bird D. The use of internal maxillary distraction for maxillary hypoplasia: a preliminary report. J Oral Maxillofac Surg. 2006; 64:1715–1720.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unilateral bimaxillary vertical elongation by maxillary distraction osteogenesis and mandibular sagittal split ramus osteotomy: a case report
- Maxillary distraction osteogenesis in the management of cleft lip and palate: report of 2 cases
- Long-term follow-up of early cleft maxillary distraction
- Stability of orthognathic surgery for cleft lip and palate patients
- Distraction osteogenesis in patients with hemifacial microsomia