Korean Circ J.
2019 Jan;49(1):84-96. 10.4070/kcj.2018.0195.
The Accuracy and Clinical Applicability of a Sensor Based Electromagnetic Non-fluoroscopic Catheter Tracking System
- Affiliations
-
- 1Division of Cardiology, Department of Medicine, Taipei Veterans General Hospital, Taipei, Taiwan. epsachen@ms41.hinet.net
- 2Department of Cardiovascular Medicine, Fukushima Medical University, Fukushima, Japan.
- 3Department of Medicine, National Yang-Ming University School of Medicine, Taipei, Taiwan.
- KMID: 2430751
- DOI: http://doi.org/10.4070/kcj.2018.0195
Abstract
- BACKGROUND AND OBJECTIVES
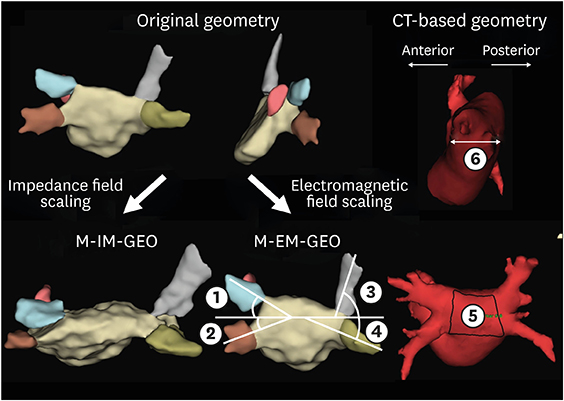
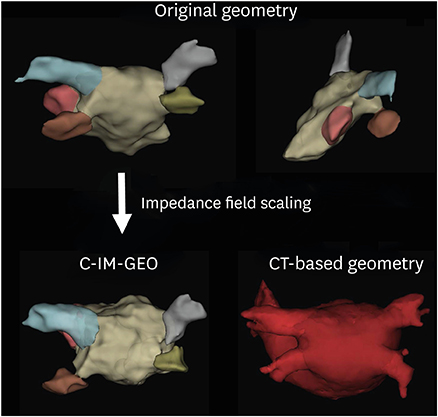
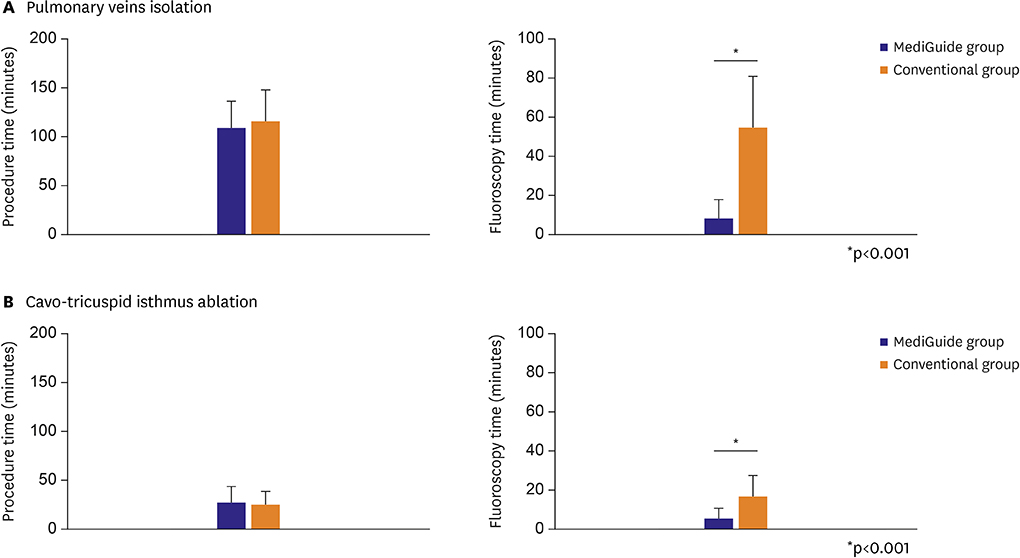
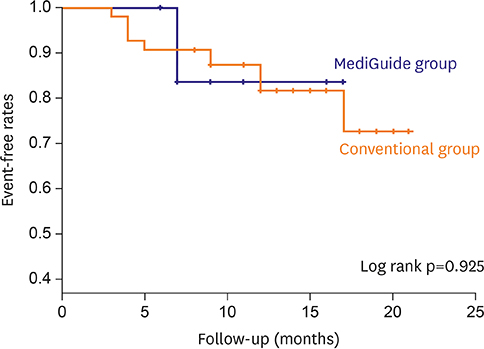
The differences between electromagnetic-based mapping (EM) and impedance-based mapping (IM) in 3D anatomical reconstruction have not been fully clarified. We aimed to investigate the anatomical accuracy between EM (MediGuideâ„¢) and IM (EnSite Velocityâ„¢) systems.
METHODS
We investigated 15 consecutive patients (10 males, mean age 58±9 years) who underwent pulmonary veins (PVs) isolation for paroxysmal atrial fibrillation (PAF). Contrast-enhanced computed tomography (CT) image of the left atrium (LA) was acquired before ablation and the 3D geometry of the LA was constructed using EM during ablation procedure. We measured the 4 PV angles between the main trunk of each PV and the posterior LA after field scaling. Additionally, the posterior LA surface area was measured. The variables were compared to those of CT-based geometry. A control group of 40 patients who underwent conventional PVs isolation using IM were also evaluated.
RESULTS
The actual and relative changes of EM and CT-based geometry in all PV angles and posterior LA were significantly smaller compared to those of IM and CT-based geometry. Intraclass correlation coefficient (ICC) between EM and CT-based geometry were 0.871 (right superior pulmonary vein [RSPV]), 0.887 (right inferior pulmonary vein [RIPV]), 0.853 (left superior pulmonary vein [LSPV]), 0.911 (left inferior pulmonary vein [LIPV]), and 0.833 (posterior LA). On the other hand, ICC between IM and CT-based geometry were 0.548 (RSPV), 0.639 (RIPV), 0.691 (LSPV), 0.706 (LIPV), and 0.568 (posterior LA).
CONCLUSIONS
Image integration with EM enables high accurate visualization of cardiac anatomy compared to IM in PAF ablation.
MeSH Terms
Figure
Reference
-
1. Cappato R, Calkins H, Chen SA, et al. Updated worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circ Arrhythm Electrophysiol. 2010; 3:32–38.
Article2. Estner HL, Deisenhofer I, Luik A, et al. Electrical isolation of pulmonary veins in patients with atrial fibrillation: reduction of fluoroscopy exposure and procedure duration by the use of a non-fluoroscopic navigation system (NavX). Europace. 2006; 8:583–587.
Article3. Rolf S, Sommer P, Gaspar T, et al. Ablation of atrial fibrillation using novel 4-dimensional catheter tracking within autoregistered left atrial angiograms. Circ Arrhythm Electrophysiol. 2012; 5:684–690.
Article4. Sommer P, Rolf S, Piorkowski C, et al. Nonfluoroscopic catheter visualization in atrial fibrillation ablation: experience from 375 consecutive procedures. Circ Arrhythm Electrophysiol. 2014; 7:869–874.5. Bourier F, Fahrig R, Wang P, et al. Accuracy assessment of catheter guidance technology in electrophysiology procedures: a comparison of a new 3D-based fluoroscopy navigation system to current electroanatomic mapping systems. J Cardiovasc Electrophysiol. 2014; 25:74–83.6. Bourier F, Reents T, Ammar-Busch S, et al. Sensor-based electromagnetic navigation (Mediguide®): how accurate is it? A phantom model study. J Cardiovasc Electrophysiol. 2015; 26:1140–1145.7. Tsao HM, Hu WC, Wu MH, et al. The impact of catheter ablation on the dynamic function of the left atrium in patients with atrial fibrillation: insights from four-dimensional computed tomographic images. J Cardiovasc Electrophysiol. 2010; 21:270–277.
Article8. Brooks AG, Wilson L, Kuklik P, et al. Image integration using NavX Fusion: initial experience and validation. Heart Rhythm. 2008; 5:526–535.
Article9. Mansour M, Holmvang G, Sosnovik D, et al. Assessment of pulmonary vein anatomic variability by magnetic resonance imaging: implications for catheter ablation techniques for atrial fibrillation. J Cardiovasc Electrophysiol. 2004; 15:387–393.
Article10. Chang SL, Tai CT, Lin YJ, et al. Comparison of cooled-tip versus 4-mm-tip catheter in the efficacy of acute ablative tissue injury during circumferential pulmonary vein isolation. J Cardiovasc Electrophysiol. 2009; 20:1113–1118.
Article11. Chang SL, Tai CT, Lin YJ, et al. Biatrial substrate properties in patients with atrial fibrillation. J Cardiovasc Electrophysiol. 2007; 18:1134–1139.
Article12. Calkins H, Kuck KH, Cappato R, et al. 2012 HRS/EHRA/ECAS Expert Consensus Statement on Catheter and Surgical Ablation of Atrial Fibrillation: recommendations for patient selection, procedural techniques, patient management and follow-up, definitions, endpoints, and research trial design. Europace. 2012; 14:528–606.
Article13. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–174.
Article14. Pillarisetti J, Kanmanthareddy A, Reddy YM, Lakkireddy D. MediGuide-impact on catheter ablation techniques and workflow. J Interv Card Electrophysiol. 2014; 40:221–227.
Article15. Fahmy TS, Mlcochova H, Wazni OM, et al. Intracardiac echo-guided image integration: optimizing strategies for registration. J Cardiovasc Electrophysiol. 2007; 18:276–282.
Article16. Roguin A, Goldstein J, Bar O, Goldstein JA. Brain and neck tumors among physicians performing interventional procedures. Am J Cardiol. 2013; 111:1368–1372.
Article17. Sommer P, Piorkowski C, Gaspar T, et al. MediGuide in supraventricular tachycardia: initial experience from a multicentre registry. Europace. 2013; 15:1292–1297.
Article18. Chida K, Saito H, Otani H, et al. Relationship between fluoroscopic time, dose-area product, body weight, and maximum radiation skin dose in cardiac interventional procedures. AJR Am J Roentgenol. 2006; 186:774–778.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Electromagnetic tracking-based ultrasound/computed tomography fusion imaging in dogs: preliminary application to ocular and periocular regions
- Non-fluoroscopic Catheter Tracking System for Atrial Fibrillation Ablation
- Development of a Real-Time Internal and External Marker Based Gating System for Proton Therapy
- Accuracy Verification of Optical Tracking System for the Maxillary Displacement Estimation by Using of Triangulation
- A Comparative Analysis of C-arm Fluoroscopic Guided and Computed Tomography-guided Stereotactic Catheter Drainage of Hypertensive Intracerebral Hematoma