Kosin Med J.
2018 Dec;33(2):171-180. 10.7180/kmj.2018.33.2.171.
The effect of short-term particular matter(2.5) exposure on asthma attacks in asthma children in Fukuoka, Japan
- Affiliations
-
- 1Department of Pediatrics, Busan St. Mary's Hospital, Busan, Korea. thdgks33@naver.com
- 2Department of Pediatrics, Fukuoka National Hospital, Japan.
- KMID: 2430732
- DOI: http://doi.org/10.7180/kmj.2018.33.2.171
Abstract
OBJECTIVES
We investigated whether asthma attacks in asthmatic children were caused by short-term exposure to particulate matter(PM)2.5.
METHODS
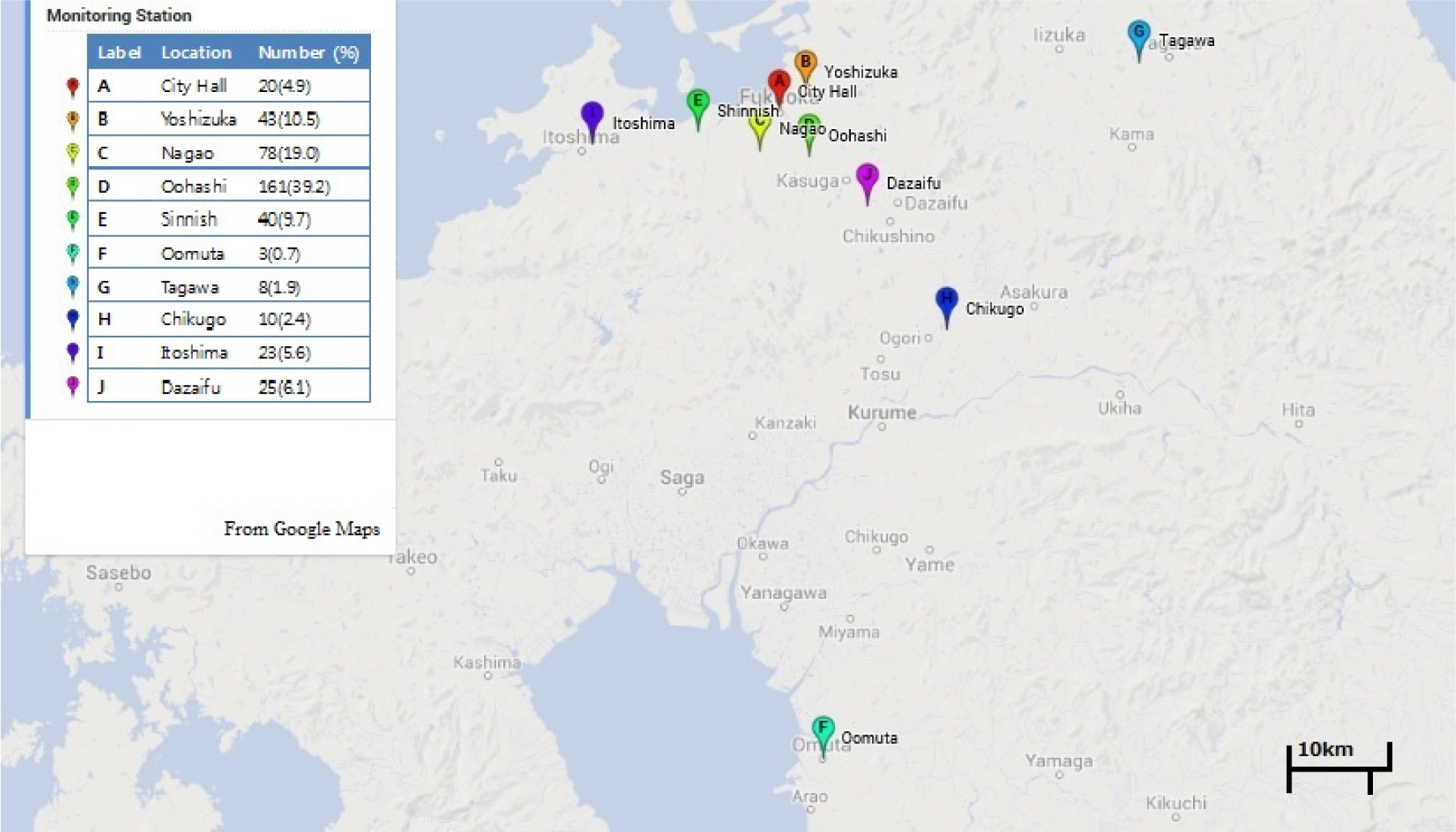
Subjects were 411 patients who received inhalation therapy in National Fukuoka Hospital, from March to May 2013. All subjects were outpatients. We surveyed the air quality measurement results in the stations closest to the address of the patients. Data were used from the City of Fukuoka website data on air pollution. We carried out a case-crossover study and compared PM2.5 concentration between 7 days after asthma attack occurred and the day asthma attack occurred and 1, 2 and 3 days before asthma attack occurred.
RESULTS
Highest hourly concentration of the day (OR 1.013, 95%CI 1.000-1.025) showed a significant association with 1 day before PM2.5 concentration statistically. And 0-1 year-old infants were more vulnerable to the highest concentration of 1 day before PM2.5 concentration(P < 0.05). Average concentration of NO2 and O3 and asthma attack also showed a significant association.
CONCLUSIONS
Maximal daily PM2.5 concentrations within 24 hours prior to the attack affect asthma exacerbation. 0-1 year-old infants are particularly vulnerable to PM2.5 concentration. Asthma exacerbation is aggravated by NO2 and O3 concentration on the day of the asthma attack.
Keyword
Figure
Reference
-
1.United States Environmental Protection Agency (2012). viewed April 17 2013. http://www.epa.gov.2.Bateson TF., Schwartz J. Children's response to air pollutants. J Toxicol Environ Health A. 2008. 71:238–43.
Article3.Strickland MJ., Darrow LA., Klein M., Flanders WD., Sarnat JA., Waller LA, et al. Short-term associations between ambient air pollutants and pediatric asthma emergency department visits. Am J Respir Crit Care Med. 2010. 182:307–16.
Article4.Yamazaki S., Shima M., Ando M., Nitta H., Watanabe H., Nishimuta T. Effect of hourly concentration of particulate matter on peak expiratory flow in hospitalized children: a panel study. Environ Health. 2011. 10:15.
Article5.Kelly FJ., Fussell JC. Air pollution and airway disease. Clin Exp Allergy. 2011. 41:1059–71.
Article6.Nishimuta T., Kondo N., Hamasaki Y., Morikawa A., Nishima S. Japanese guideline for childhood asthma. Allergology International. 2011. 60:147–69.
Article7.Ueda K., Nitta H., Odajima H. The effects of weather, air pollutants, and Asian dust on hospitalization for asthma in Fukuoka. Environ Health Prev Med. 2010. 15:350–7.
Article8.Odajima H., Yamazaki S., Nitta H. Decline in peak expiratory flow according to hourly short-term concentration of particulate matter in asthmatic children. Inhal Toxicol. 2008. 20:1263–72.
Article9.Iskandar A. Andersen ZJ, Bonnelykke K, Ellermann T, Andersen KK, Bisgaard H. Coarse and fine particles but not ultrafine particles in urban air trigger hospital admission for asthma in children. Thorax. 2012. 67:252–7.10.Lin S., Liu X., Le LH., Hwang SA. Chronic exposure to ambient ozone and asthma hospital admissions among children. Environ Health Perspect. 2008. 116:1725–30.
Article11.Meng YY., Rull RP., Wilhelm M., Lombardi C., Balmes J., Ritz B. Outdoor air pollution and uncontrolled asthma in the San Joaquin Valley, California. J Epidemiol Community Health. 2010. 64:142–7.
Article12.Lipsett M., Hurley S., Ostro B. Air pollution and emergency room visits for asthma in Santa Clara Country, California. Environ Health Perspect. 1997. 105:216–22.13.Gauderman WJ., Avol E., Lurmann F., Kuenzli N., Gilliland F., Peters J, et al. Childhood asthma and exposure to traffic and nitrogen dioxide. Epidemiology. 2005. 16:737–43.
Article14.Selgrade MK., Plopper CG., Gilmour MI., Conolly RB., Foos BSP. Assessing the health effects and risks associated with children's inhalation exposures: asthma and allergy. J Toxicol Environ Health A. 2008. 71:196–207.15.Trasande L., Thurston GD. The role of air pollution in asthma and other pediatric morbidities. J Allergy Clin Immunol. 2005. 115:689–99.
Article16.Gaudeman WJ., Avol E., Gilliland F., Vora H., Thomas D., Berhane K, et al. The effect of air pollution on lung development from 10 to 18 years of age. N Engl J Med. 2004. 351:1057–67.
Article17.Song S., Lee K., Lee YM., Lee JH., Lee SI., Yu SD, et al. Acute health effects of urban fine and ultrafine particles on children with atopic dermatitis. Environ Res. 2011. 111:394–9.
Article18.Konishi S., Ng CFS., Stickley A., Nishihata S., Shinsugi C., Ueda K, et al. Particulate matter modifies the association between airborne pollen and daily medical consultations for pollinosis in Tokyo. Sci Total Environ. 2014. 499:125–32.
Article19.Lim JM., Jeong JH., Lee JH., Moon JH., Chung YS., Kim KH. The analysis of PM2.5 and associated elements and their indoor/outdoor pollution status in an urban area. Indoor Air. 2011. 2:145–55.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- PM(2.5) and pediatric asthma
- Omalizumab and unmet needs in severe asthma and allergic comorbidities in Japanese children
- Evolution of Asthma Concept and Effect of Current Asthma Management Guidelines
- Short-term Effect of Fine Particulate Matter on Children's Hospital Admissions and Emergency Department Visits for Asthma: A Systematic Review and Meta-analysis
- Occupational asthma in Japan