J Korean Soc Spine Surg.
2018 Dec;25(4):147-153. 10.4184/jkss.2018.25.4.147.
The Therapeutic Effect of Postganglionic Nerve Block for Symptomatic Schmorl Nodule: A Retrospective Case Series
- Affiliations
-
- 1Department of Orthopedic Surgery, Konkuk University Medical Center, Seoul, Korea.
- 2Department of Orthopedic Surgery, Seoul Red Cross Hospital, Seoul, Korea.
- 3Department of Orthopedic Surgery, Seoul Chuk Hospital, Gyeonggi-do, Korea. orthopedicspinae@gmail.com
- KMID: 2430139
- DOI: http://doi.org/10.4184/jkss.2018.25.4.147
Abstract
- STUDY DESIGN: Retrospective case series.
OBJECTIVES
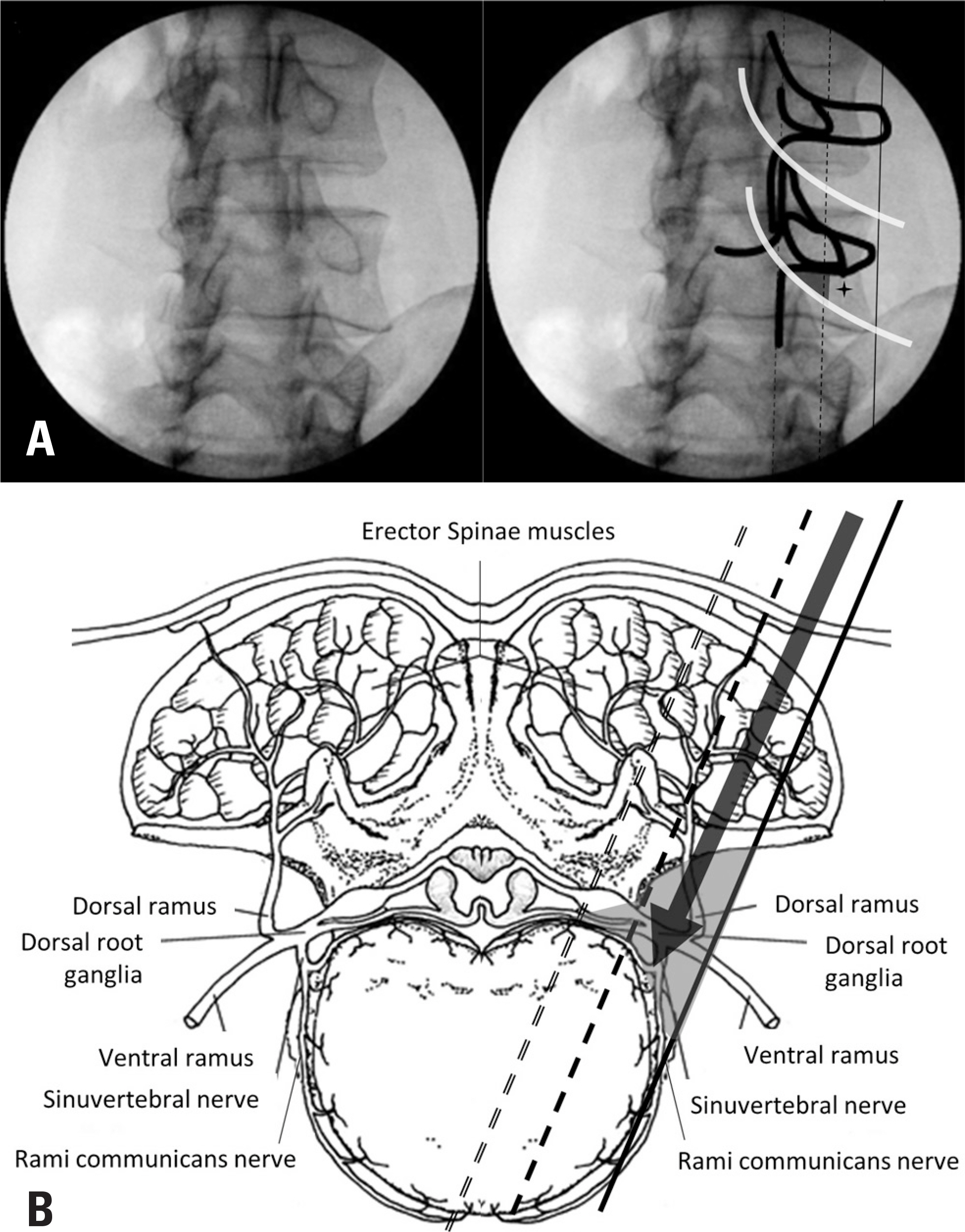
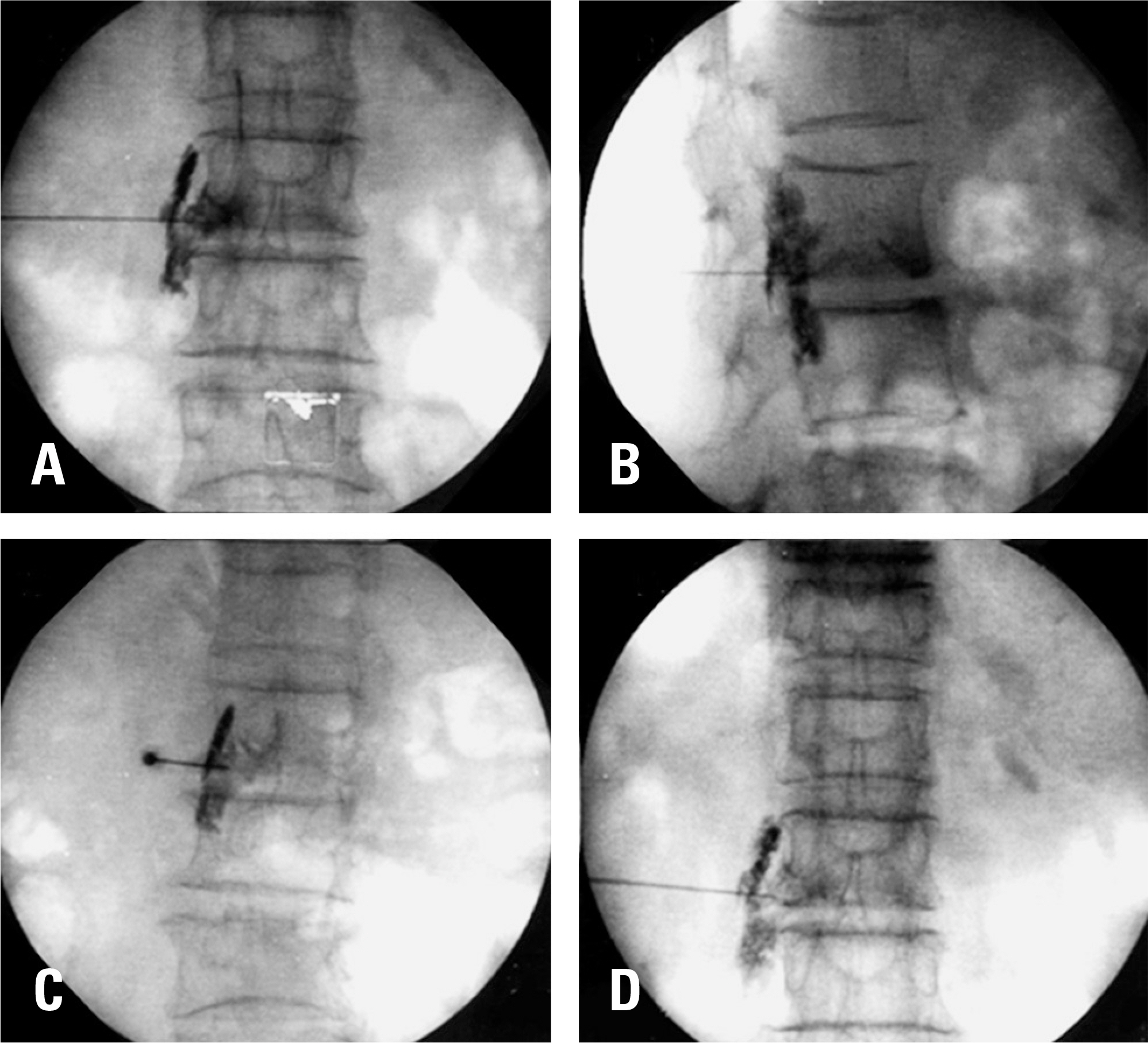
We retrospectively evaluated the clinical efficacy of postganglionic nerve block in symptomatic Schmorl nodules (SNs). SUMMARY OF LITERATURE REVIEW: SNs are common lesions that are often asymptomatic. In certain cases, SNs have been reported to cause severe axial back pain, thereby considerably impacting patients' quality of life. No consensus currently exists on the treatment of symptomatic SNs.
MATERIALS AND METHODS
From October 2015 to October 2017, a total of 21 patients with symptomatic SNs diagnosed by magnetic resonance imaging (MRI) that did not respond to conservative treatment after 4 weeks were included in the study. All patients received postganglionic nerve block. We evaluated effective pain relief (improvement of back pain of more than 50% compared with before the intervention) and functional improvements, assessed by visual analogue scale (VAS) and Oswestry Disability Index scores obtained at 4 hours, 4 weeks, 8 weeks, 3 months, and 6 months after the procedure.
RESULTS
Symptomatic SNs were more common at the L2-3 level, and the lower end plate was more commonly involved than the upper end plate. Eighteen of the 21 patients (85.7%) showed effective pain relief, and no deterioration was observed within the follow-up period. Throughout the follow-up period, the VAS remained significantly improved compared to before the procedure (p < 0.05). Complications were not reported in any cases.
CONCLUSIONS
Postganglionic nerve block for symptomatic SNs that do not respond to conservative treatment is a non-invasive modality for pain relief.
MeSH Terms
Figure
Reference
-
1. Hamanishi C, Kawabata T, Yosii T, et al. Schmorl's nodes on magnetic resonance imaging. Their incidence and clinical relevance. Spine. 1994 Feb; 19(4):450–3. DOI: 10.1097/00007632-199402001-00012.2. Jensen MC, Brant-Zawadzki MN, Obuchowski N, et al. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med. 1994 July; 331(2):6973. DOI: 10.1056/NEJM199407143310201.
Article3. Resnick D, Niwayama G. Intravertebral disk herniations: cartilaginous (Schmorl's) nodes. Radiology. 1978 Jan; 126(1):57–65. DOI: 10.1148/126.1.57.
Article4. Schmorl G. Ü ber die an den wirbelbandscheiben vorkom-menden ausdehnungs und zerreissungsvorgä nge und die dadurch an ihnen und der wirbelspongiosa hervorgerufenen verä nderungen. Verh Dtsch Ges Pathol. 1927; 22:250.5. Hasegawa K, Ogose A, Morita T, et al. Painful Schmorl's node treated by lumbar interbody fusion. Spinal Cord. 2004 Feb; 42(2):124. DOI: 10.1038/sj.sc.3101506.
Article6. Takahashi K, Takata K. A large painful Schmorl's node: a case report. J Spinal Disord. 1994 Feb; 7(1):77–81. DOI: 10.1097/00002517-199407010-00011.7. Grivé E, Rovira A, Capellades J, et al. Radiologic findings in two cases of acute Schmö rl's nodes. Am J Neuroradiol. 1999 Oct; 20(9):1717–21.8. Ohnari H, Takino T, Takahashi LK, et al. Schmorl's nodes and low-back pain. Analysis of magnetic resonance imaging findings in symptomatic and asymptomatic individu-als. Eur Spine J. 1994 Dec; 4(1):56–9. DOI: 10.1007/bf00298420.9. Jang JS, Kwon HK, Lee JJ, et al. Rami communicans nerve block for the treatment of symptomatic schmorl's nodes-A case report. Korean J Pain. 2010 Dec; 23(4):262–5. DOI: 10.3344/kjp.2010.23.4.262.10. Peng B, Chen J, Kuang Z, et al. Diagnosis and surgical treatment of back pain originating from endplate. Eur Spine J. 2009 July; 18(7):1035–40. DOI: 10.1007/s00586-009-0938-4.
Article11. Wenger M, Markwalder T-M. Fluoronavigation-assisted, lumbar vertebroplasty for a painful Schmorl node. J Clin Neurosci. 2009 Sep; 16(9):1250–1. DOI: 10.1016/j.jocn.2008.11.016.
Article12. Garcia-Cosamalon J, del Valle ME, Calavia MG, et al. Intervertebral disc, sensory nerves and neurotrophins: who is who in discogenic pain? J Anat. 2010 Jul; 217(1):1–15. DOI: 10.1111/j.1469-7580.2010.01227.x.13. Suseki K, Takahashi Y, Takahashi K, et al. Sensory nerve fibres from lumbar intervertebral discs pass through rami communicantes. A possible pathway for discogenic low back pain. J Bone Joint Surg Br. 1998 Jul; 80(4):737–42. DOI: 10.1302/0301-620X.80B4.0800737.14. Williams F, Manek N, Sambrook P, et al. Schmorl's nodes: common, highly heritable, and related to lumbar disc disease. Arthritis Care Res (Hoboken). 2007 May; 57(5):855–60. DOI: 10.1002/art.22789.
Article15. Teraguchi M, Yoshimura N, Hashizume H, et al. The asso-ciation of combination of disc degeneration, end plate signal change, and Schmorl node with low back pain in a large population study: the Wakayama Spine Study. Spine J. 2015 Apr; 15(4):622–8. DOI: 10.1016/j.spinee.2014.11.012.
Article16. Jayson M, Herbert C, Barks J. Intervertebral discs: nuclear morphology and bursting pressures. Ann Rheum Dis. 1973 Jul; 32(4):308–15. DOI: DOI:10.1136/ard.32.4.308.
Article17. Liu J, Hao L, Zhang X, et al. Painful Schmorl's nodes treated by discography and discoblock. Eur Spine J. 2018 Jan; 27(1):13–8. DOI: DOI:10.1007/s00586-017-4996-8.
Article18. Park P, Tran N, Gala V, et al. The radiographic evolution of a Schmorl's node. British journal of neurosurgery. 2007; 21(2):224–7. DOI: 10.1080/02688690701317169.
Article19. Koshi T, Ohtori S, Inoue G, et al. Lumbar posterolateral fusion inhibits sensory nerve ingrowth into punctured lumbar intervertebral discs and upregulation of CGRP immunore-active DRG neuron innervating punctured discs in rats. Eur Spine J. 2010 Apr; 19(4):593–600. DOI: 10.1007/s00586-009-1237-9.
Article20. Takahashi K, Aoki Y, Ohtori S. Resolving discogenic pain. Eur Spine J. 2008 Dec; 17(4 Suppl):428–31. DOI: 10.1007/s00586-008-0752-4.
Article21. He SC, Zhong BY, Zhu HD, et al. Percutaneous vertebroplasty for symptomatic Schmorl's nodes: 11 cases with long-term follow-up and a literature review. Pain Physician. 2017 Feb; 20(2):69–76.22. Masala S, Pipitone V, Tomassini M, et al. Percutaneous vertebroplasty in painful schmorl nodes. Cardiovasc Intervent Radiol. 2006 Feb; 29(1):97–101. DOI: 10.1007/s00270-005-0153-6.
Article23. Cuellar JM, Stauff MP, Herzog RJ, et al. Does provocative discography cause clinically important injury to the lumbar intervertebral disc? A 10-year matched cohort study. Spine J. 2016 Mar; 16(3):273–80. DOI: 10.1016/j.spinee.2015.06.051.
Article24. Masoud Hashemi M, Mofrad MK. Anatomical flow pattern of contrast in lumbar epidural space: a human study with a midline vs. parasagittal interlaminar approach under fluoroscopy. Pain Physician. 2015 Jul-Aug; 18(4):317–24.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Rami Communicans Nerve Block for the Treatment of Symptomatic Schmorl's Nodes: A Case Report
- Schmorl’s Node Accompanying Multiple Osteonecroses
- Complete Separation of the Vertebral Body Associated with a Schmorl's Node Accompanying Severe Osteoporosis
- Acute Schmorl Node in Dorsal Spine: An Unusual Cause of a Sudden Onset of Severe Back Pain in a Young Female
- The Frequency-Dependence of Pre- and Postganglionic Nerve Stimulation of Pig and Rat Bladder