J Korean Orthop Assoc.
2018 Dec;53(6):490-497. 10.4055/jkoa.2018.53.6.490.
Cementless Total Hip Arthroplasty Using Ceramic Femoral Head on Cross-Linked Ultra-High-Molecular Weight Polyethylene Liner in Patients Older than 65 Years: Minimum Five-Year Follow-Up Results
- Affiliations
-
- 1Department of Orthopedic Surgery, VHS Medical Center, Seoul, Korea. 3188yun@naver.com
- KMID: 2430055
- DOI: http://doi.org/10.4055/jkoa.2018.53.6.490
Abstract
- PURPOSE
To evaluate the utility of ceramic-on-polyethylene articular bearing surface when cementless total hip arthroplasty is performed in patients older than 65 years through an analysis of the minimum five-year follow-up results using the ceramic femoral head and cross-linked polyethylene liner.
MATERIALS AND METHODS
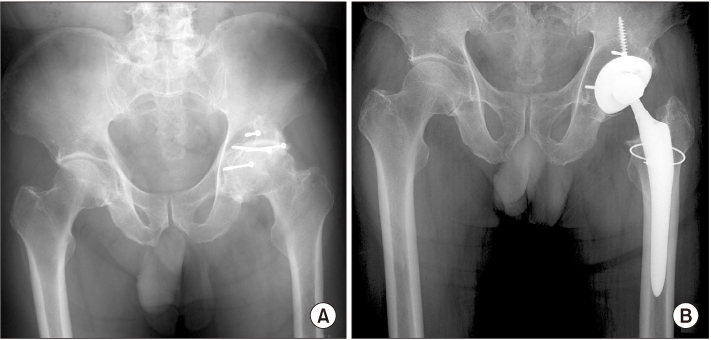
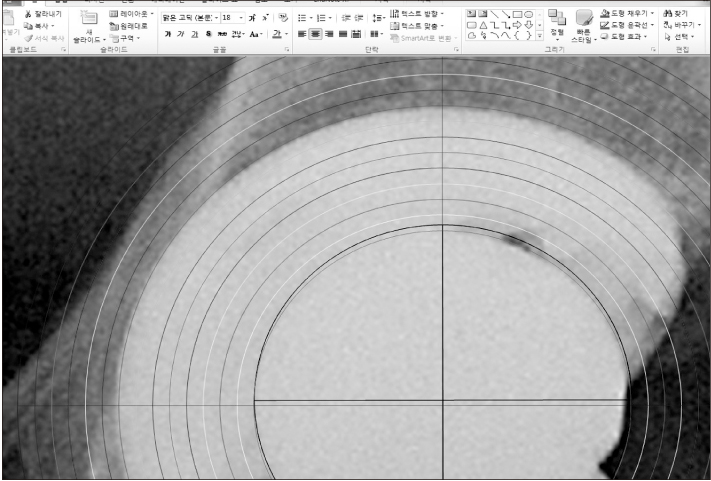
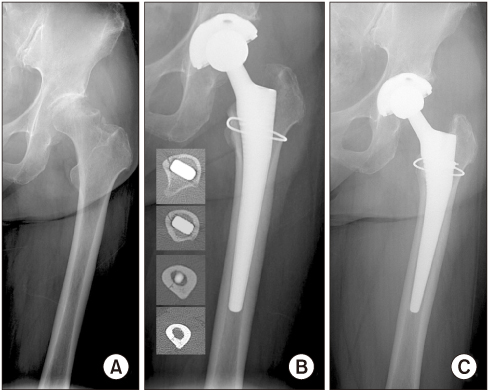
From March 2010 to September 2012, 51 patients (56 hips) who were older than 65 years were enrolled in this retrospective study. The mean age at surgery was 70.9±5.1 years old. A clinical assessment was analyzed using the Harris hip score. For the radiographic assessment, the cup inclination and anteversion, stem alignment, and wear amount were measured. The postoperative complications were also determined.
RESULTS
The mean Harris hip score was improved from preoperative 48 points to postoperative 87 points (p < 0.05). The mean cup inclination was 40.9°±6.4° and the mean cup anteversion was 20.3°±8.1°. The mean cup anteversion of the elevated liner-used group (16 cases) was 14.3°±7.9° and the mean cup anteversion of the neutral liner used group (40 cases) was 22.4°±9.1° (p < 0.05). The mean stem alignment angle was 0° (range, varus 4°-valgus 4°). The mean linear wear amount was 0.458±0.041 mm and the average annual linear wear rate was 0.079±0.032 mm/yr. Six cases (10.7%) of intraoperative periprosthetic femoral fractures were encountered.
CONCLUSION
Based on these results, the use of a ceramic-on-polyethylene articular bearing surface in elderly patients with cementless total hip arthroplasty is beneficial. On the other hand, careful effort is needed to prevent intraoperative periprosthetic femoral fractures.
Keyword
MeSH Terms
Figure
Reference
-
1. Clarke IC, Good V, Anissian L, Gustafson A. Charnley wear model for validation of hip simulators: ball diameter versus polytetrafluoroethylene and polyethylene wear. Proc Inst Mech Eng H. 1997; 211:25–36.
Article2. Sochart DH, Porter ML. The long-term results of Charnley low-friction arthroplasty in young patients who have congenital dislocation, degenerative osteoarthrosis, or rheumatoid arthritis. J Bone Joint Surg Am. 1997; 79:1599–1617.
Article3. Endo M, Tipper JL, Barton DC, Stone MH, Ingham E, Fisher J. Comparison of wear, wear debris and functional biological activity of moderately crosslinked and non-crosslinked polyethylenes in hip prostheses. Proc Inst Mech Eng H. 2002; 216:111–122.
Article4. Galvin A, Kang L, Tipper J, et al. Wear of crosslinked polyethylene under different tribological conditions. J Mater Sci Mater Med. 2006; 17:235–243.
Article5. McKellop H, Shen FW, Lu B, Campbell P, Salovey R. Development of an extremely wear-resistant ultra high molecular weight polyethylene for total hip replacements. J Orthop Res. 1999; 17:157–167.6. Semlitsch M, Lehmann M, Weber H, Doerre E, Willert HG. New prospects for a prolonged functional life-span of artificial hip joints by using the material combination polyethylene/aluminium oxide ceramin/metal. J Biomed Mater Res. 1977; 11:537–552.7. Clarke IC, Gustafson A. Clinical and hip simulator comparisons of ceramic-on-polyethylene and metal-on-polyethylene wear. Clin Orthop Relat Res. 2000; (379):34–40.
Article8. Abdel MP, Heyse TJ, Elpers ME, Mayman DJ, Su EP, Pellicci PM, et al. Ceramic liner fractures presenting as squeaking after primary total hip arthroplasty. J Bone Joint Surg Am. 2014; 96:27–31.
Article9. Baek SH, Kim WK, Kim JY, Kim SY. Do alumina matrix composite bearings decrease hip noises and bearing fractures at a minimum of 5 years after THA? Clin Orthop Relat Res. 2015; 473:3796–3802.
Article10. Davies AP, Willert HG, Campbell PA, Learmonth ID, Case CP. An unusual lymphocytic perivascular infiltration in tissues around contemporary metal-on-metal joint replacements. J Bone Joint Surg Am. 2005; 87:18–27.
Article11. Yoon PW, Yoo JJ, Kim Y, Yoo S, Lee S, Kim HJ. The epidemiology and national trends of bearing surface usage in primary total hip arthroplasty in Korea. Clin Orthop Surg. 2016; 8:29–37.
Article12. Lehil MS, Bozic KJ. Trends in total hip arthroplasty implant utilization in the United States. J Arthroplasty. 2014; 29:1915–1918.
Article13. Rajaee SS, Trofa D, Matzkin E, Smith E. National trends in primary total hip arthroplasty in extremely young patients: a focus on bearing surface usage. J Arthroplasty. 2012; 27:1870–1878.14. Capello WN, D'Antonio JA, Naughton M. Periprosthetic fractures around a cementless hydroxyapatite-coated implant: a new fracture pattern is described. Clin Orthop Relat Res. 2014; 472:604–610.
Article15. Bozic KJ, Ong K, Lau E, et al. Risk of complication and revision total hip arthroplasty among Medicare patients with different bearing surfaces. Clin Orthop Relat Res. 2010; 468:2357–2362.
Article16. Yun HH, Yoon JR, Yang JH, Song SY, Park SB, Lee JW. A validation study for estimation of femoral anteversion using the posterior lesser trochanter line: an analysis of computed tomography measurement. J Arthroplasty. 2013; 28:1776–1780.17. Khan M, Della Valle CJ, Jacofsky DJ, Meneghini RM, Haddad FS. Early postoperative complications after total hip arthroplasty: current strategies for prevention and treatment. Instr Course Lect. 2015; 64:337–346.18. Widmer KH. A simplified method to determine acetabular cup anteversion from plain radiographs. J Arthroplasty. 2004; 19:387–390.
Article19. Yun HH, Shon WY, Yoon JR, Yang JH, Lim DS. Reliability of a PowerPoint method for wear measurement after total hip arthroplasty: a retrieval study using 3-dimensional laser scanning. J Arthroplasty. 2012; 27:1530–1537.20. Yun HH, Jajodia NK, Myung JS, Oh JK, Park SW, Shon WY. Use of slide presentation software as a tool to measure hip arthroplasty wear. J Arthroplasty. 2009; 24:1210–1215.
Article21. Danoff JR, Bobman JT, Cunn G, et al. Redefining the acetabular component safe zone for posterior approach total hip arthroplasty. J Arthroplasty. 2016; 31:506–511.
Article22. Sculco PK, Austin MS, Lavernia CJ, Rosenberg AG, Sierra RJ. Preventing leg length discrepancy and instability after total hip arthroplasty. Instr Course Lect. 2016; 65:225–241.23. Cobb TK, Morrey BF, Ilstrup DM. The elevated-rim acetabular liner in total hip arthroplasty: relationship to postoperative dislocation. J Bone Joint Surg Am. 1996; 78:80–86.24. Cobb TK, Morrey BF, Ilstrup DM. Effect of the elevated-rim acetabular liner on loosening after total hip arthroplasty. J Bone Joint Surg Am. 1997; 79:1361–1364.
Article25. Insull PJ, Cobbett H, Frampton CM, Munro JT. The use of a lipped acetabular liner decreases the rate of revision for instability after total hip replacement: a study using data from the New Zealand Joint Registry. Bone Joint J. 2014; 96:884–888.26. Kim YH, Park JW, Kim JS. Alumina delta-on-highly crosslinked-remelted polyethylene bearing in cementless total hip arthroplasty in patients younger than 50 years. J Arthroplasty. 2016; 31:2800–2804.
Article27. Orradre Burusco I, Romero R, Brun M, López Blasco JJ. Cross-linked ultra-high-molecular weight polyethylene liner and ceramic femoral head in total hip arthroplasty: a prospective study at 5 years follow-up. Arch Orthop Trauma Surg. 2011; 131:1711–1716.28. Wang S, Zhang S, Zhao Y. A comparison of polyethylene wear between cobalt-chrome ball heads and alumina ball heads after total hip arthroplasty: a 10-year follow-up. J Orthop Surg Res. 2013; 8:20.
Article29. Rajpura A, Kendoff D, Board TN. The current state of bearing surfaces in total hip replacement. Bone Joint J. 2014; 96:147–156.
Article30. Berry DJ. Epidemiology: hip and knee. Orthop Clin North Am. 1999; 30:183–190.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Wear Rate and Survivorship in Total Hip Arthroplasty Using a Third-generation Ceramic Head on a Conventional Polyethylene Liner: A Minimum of 15-year Follow-up
- Ceramic Head Fracture in Ceramic-on-Polyethylene Total Hip Arthroplasty
- Failure of a Metal Femoral Head after Revision Total Hip Arthroplasty for a Ceramic Liner Fracture
- A Case of Failure of a Ceramic Head in Total Hip Arthroplasty: A Case Report
- Ceramic on Sandwich Ceramic Bearing Primary Cementless Total Hip Arthroplasty (Result of 2 to 5 years follow up)