Korean J Gastroenterol.
2018 Dec;72(6):304-307. 10.4166/kjg.2018.72.6.304.
Gastric Tuberculosis Presenting as a Subepithelial Mass: A Rare Cause of Gastrointestinal Bleeding
- Affiliations
-
- 1Department of Radiology, Division of Gastroenterology, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea.
- 2Department of Internal Medicine, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea. endoksj@gmail.com
- 3Department of Surgery, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea.
- KMID: 2429947
- DOI: http://doi.org/10.4166/kjg.2018.72.6.304
Abstract
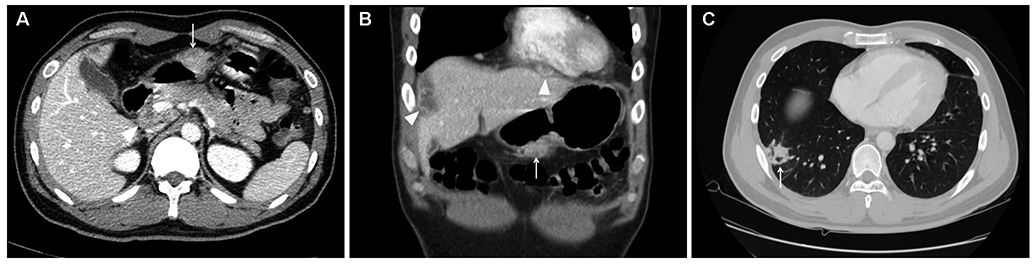
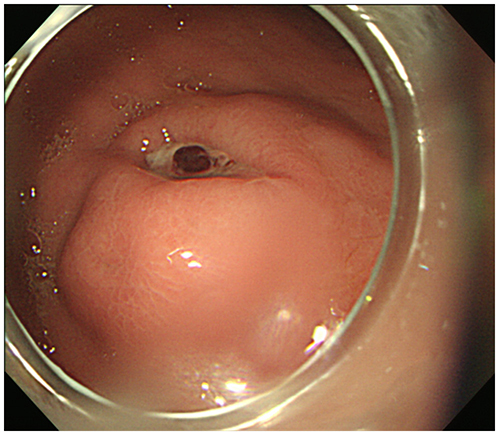
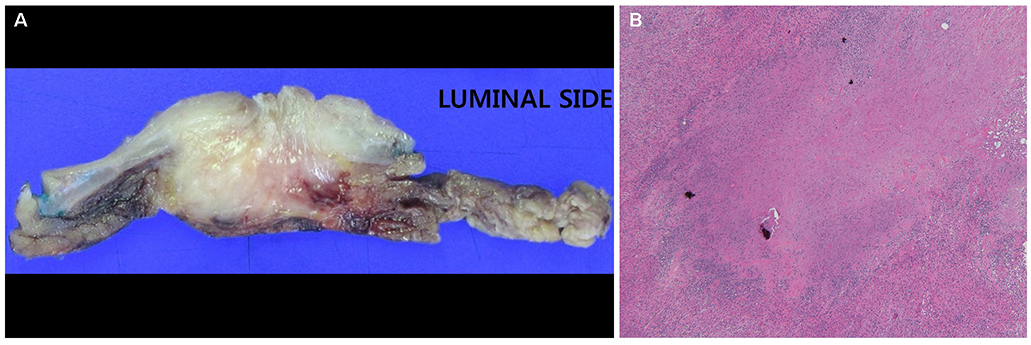
- Gastric tuberculosis accounts for approximately 2% of all cases of gastrointestinal tuberculosis. Diagnosis of gastric tuberculosis is challenging because it can present with various clinical, endoscopic, and radiologic features. Tuberculosis manifesting as a gastric subepithelial tumor is exceedingly rare; only several dozen cases have been reported. A 30-year-old male visited emergency room of our hospital with hematemesis and melena. Abdominal CT revealed a 2.5 cm mass in the gastric antrum, and endoscopy revealed a subepithelial mass with a visible vessel at its center on gastric antrum. Primary gastric tuberculosis was diagnosed by surgical wedge resection. We report a rare case of gastric tuberculosis mimicking a subepithelial tumor with acute gastric ulcer bleeding.
MeSH Terms
Figure
Reference
-
1. Singh V, Jain AK, Agrawal AK, et al. Clinicopathological profile of abdominal tuberculosis. Br J Clin Pract. 1995; 49:22–24.2. Subei I, Attar B, Schmitt G, Levendoglu H. Primary gastric tuberculosis: a case report and literature review. Am J Gastroenterol. 1987; 82:769–772.3. Petroianni A, Mugnaini L, Laurendi G, et al. Abdominal tuberculosis mimicking Crohn's disease: a difficult diagnosis. Report of a case. Panminerva Med. 2002; 44:155–158.4. Talukdar R, Khanna S, Saikia N, Vij JC. Gastric tuberculosis presenting as linitis plastica: a case report and review of the literature. Eur J Gastroenterol Hepatol. 2006; 18:299–303.
Article5. Rana SS, Bhasin DK, Srinivasan R, Singh K. Gastric outlet obstruction caused by tuberculosis and diagnosed by endoscopic ultrasound-guided fine needle aspiration. Endoscopy. 2011; 43:Suppl 2 UCTN. E117–E118.
Article6. Kim SH, Park JH, Kang KH, et al. Gastric tuberculosis presenting as a submucosal tumor. Gastrointest Endosc. 2005; 61:319–322.
Article7. Gupta V, Goel MM, Noushif M, Rai P, Gupta P, Chandra A. Primary gastric tuberculosis mimicking gastrointestinal stromal tumor. Am J Gastroenterol. 2012; 107:1269–1270.
Article8. Ardengh JC, Vaiciunas S, Kemp R, Venco F, Lima-Filho ER, dos Santos JS. Upper endoscopy versus endosonography in differential diagnosis of gastrointestinal bulging. Arq Gastroenterol. 2011; 48:236–241.
Article9. Kruijshaar ME, Abubakar I. Increase in extrapulmonary tuberculosis in England and Wales 1999–2006. Thorax. 2009; 64:1090–1095.
Article10. Tromba JL, Inglese R, Rieders B, Todaro R. Primary gastric tuberculosis presenting as pyloric outlet obstruction. Am J Gastroenterol. 1991; 86:1820–1822.11. Mitchell RS, Bristol LJ. Intestinal tuberculosis: an analysis of 346 cases diagnosed by routine intestinal radiography on 5,529 admissions for pulmonary tuberculosis, 1924–49. Am J Med Sci. 1954; 227:241–249.12. Shibagaki K, Miyaike J, Onji M, et al. Submucosal tumor-like lesion originating from colon tuberculosis: a case report and review of the literature. Clin J Gastroenterol. 2015; 8:207–211.
Article13. Kim DY, Bang S, Park BK, et al. Tuberculous mesenteric lymphadenitis involving the gastric wall: case report. Gastrointest Endosc. 2005; 62:799–802.
Article14. Lee TH, Cho JY, Bok GH, Cho WY, Jin SY. Intra-abdominal tuberculous lymphadenitis diagnosed using an endoscopic ultrasonography-guided Procore needle biopsy. Clin Endosc. 2013; 46:77–80.
Article15. Paustian FF, Marshall JB. Intestinal tuberculosis. In : Berk JE, editor. Gastroenteroscopy. Volume 3. 4th ed. Philadelphia: WB Saunders;1985. p. 2018–2036.16. Gaines W, Steinbach HL, Lowenhaupt E. Tuberculosis of the stomach. Radiology. 1952; 58:808–819.
Article17. Rao YG, Pande GK, Sahni P, Chattopadhyay TK. Gastroduodenal tuberculosis management guidelines, based on a large experience and a review of the literature. Can J Surg. 2004; 47:364–368.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Gastric Calcifying Fibrous Tumor Presenting as a Subepithelial Tumor
- Incidental Gastrointestinal Subepithelial Mass
- Gastric Ulcer Bleeding associated with a Left Gastric Artery Pseudoaneurysm
- A Case of Gastric Candidiasis Presented as Subepithelial Mass in an Immunocompromised Host
- Diagnosis of Gastric Subepithelial Tumor: Focusing on Endoscopic Ultrasonography