J Gastric Cancer.
2018 Dec;18(4):392-399. 10.5230/jgc.2018.18.e39.
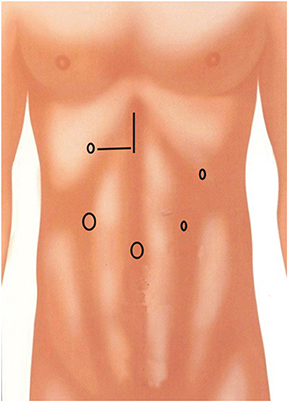
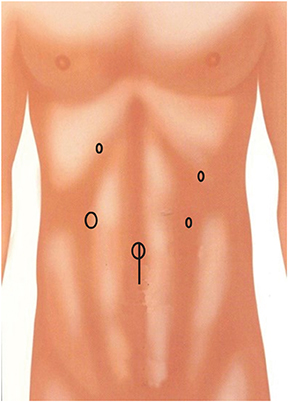
Risk Factors for the Development of Incisional Hernia in Mini-laparotomy Wounds Following Laparoscopic Distal Gastrectomy in Patients with Gastric Cancer
- Affiliations
-
- 1Department of Surgery, Dong-A University College of Medicine, Busan, Korea. mckim@dau.ac.kr
- KMID: 2429885
- DOI: http://doi.org/10.5230/jgc.2018.18.e39
Abstract
- PURPOSE
To determine the incidence of incisional hernia (IH) in mini-laparotomy wounds and analyze the risk factors of IH following laparoscopic distal gastrectomy in patients with gastric cancer.
MATERIALS AND METHODS
A total of 565 patients who underwent laparoscopic distal gastrectomy for gastric cancer at Dong-A University Hospital, Busan, South Korea, between June 2010 and December 2015, were enrolled. IH was diagnosed through physical examination or computed tomography imaging. Incidence rate and risk factors of IH were evaluated through a long-term follow-up.
RESULTS
Of those enrolled, 16 patients (2.8%) developed IH. The median duration of follow-up was 58 months (range, 25-90 months). Of the 16 patients with IH, 15 (93.7%) were diagnosed within 12 months postoperatively. Multivariate analysis showed that female sex (odds ratio [OR], 3.869; 95% confidence interval [CI], 1.325-11.296), higher body mass index (BMI; OR, 1.229; 95% CI, 1.048-1.422), and presence of comorbidity (OR, 3.806; 95% CI, 1.212-11.948) were significant risk factors of IH. The vast majority of IH cases (15/16 patients, 93.7%) developed in the totally laparoscopic distal gastrectomy (TLDG) group. However, the type of surgery (i.e., TLDG or laparoscopy-assisted distal gastrectomy) did not significantly affect the development of IH (P=0.060).
CONCLUSIONS
A median follow-up of 58 months showed that the overall incidence of IH in mini-laparotomy wounds was 2.8%. Multivariate analysis showed that female sex, higher BMI, and presence of comorbidity were significant risk factors of IH. Thus, surgeons should monitor the closure of mini-laparotomy wounds in patients with risk factors of IH undergoing laparoscopic distal gastrectomy.
Keyword
MeSH Terms
Figure
Reference
-
1. Mullassery D, Pedersen A, Robb A, Smith N. Incisional hernia in pediatric surgery - experience at a single UK tertiary centre. J Pediatr Surg. 2016; 51:1791–1794.
Article2. Itatsu K, Yokoyama Y, Sugawara G, Kubota H, Tojima Y, Kurumiya Y, et al. Incidence of and risk factors for incisional hernia after abdominal surgery. Br J Surg. 2014; 101:1439–1447.
Article3. Paya K, Wurm J, Fakhari M, Felder-Puig R, Puig S. Trocar-site hernia as a typical postoperative complication of minimally invasive surgery among preschool children. Surg Endosc. 2008; 22:2724–2727.
Article4. Cost NG, Lee J, Snodgrass WT, Harrison CB, Wilcox DT, Baker LA. Hernia after pediatric urological laparoscopy. J Urol. 2010; 183:1163–1167.
Article5. Lee L, Mata J, Droeser RA, Kaneva P, Liberman S, Charlebois P, et al. Incisional hernia after midline versus transverse specimen extraction incision: a randomized trial in patients undergoing laparoscopic colectomy. Ann Surg. 2018; 268:41–47.6. Dakour Aridi H, Alami R, Tamim H, Shamseddine G, Fouani T, Safadi B. Long-term outcomes of laparoscopic sleeve gastrectomy: a Lebanese center experience. Surg Obes Relat Dis. 2016; 12:1689–1696.
Article7. Kim W, Kim HH, Han SU, Kim MC, Hyung WJ, Ryu SW, et al. Decreased morbidity of laparoscopic distal gastrectomy compared with open distal gastrectomy for stage I gastric cancer: short-term outcomes from a multicenter randomized controlled trial (KLASS-01). Ann Surg. 2016; 263:28–35.8. Hu Y, Huang C, Sun Y, Su X, Cao H, Hu J, et al. Morbidity and mortality of laparoscopic versus open D2 distal gastrectomy for advanced gastric cancer: a randomized controlled trial. J Clin Oncol. 2016; 34:1350–1357.
Article9. Hiki N, Katai H, Mizusawa J, Nakamura K, Nakamori M, Yoshikawa T, et al. Long-term outcomes of laparoscopy-assisted distal gastrectomy with suprapancreatic nodal dissection for clinical stage I gastric cancer: a multicenter phase II trial (JCOG0703). Gastric Cancer. 2018; 21:155–161.
Article10. Chen K, Mou YP, Xu XW, Pan Y, Zhou YC, Cai JQ, et al. Comparison of short-term surgical outcomes between totally laparoscopic and laparoscopic-assisted distal gastrectomy for gastric cancer: a 10-y single-center experience with meta-analysis. J Surg Res. 2015; 194:367–374.
Article11. Han G, Park JY, Kim YJ. Comparison of short-term postoperative outcomes in totally laparoscopic distal gastrectomy versus laparoscopy-assisted distal gastrectomy. J Gastric Cancer. 2014; 14:105–110.
Article12. Cybulska P, Schiavone MB, Sawyer B, Gardner GJ, Zivanovic O, Brown CL, et al. Trocar site hernia development in patients undergoing robotically assisted or standard laparoscopic staging surgery for endometrial cancer. Gynecol Oncol. 2017; 147:371–374.
Article13. Yahchouchy-Chouillard E, Aura T, Picone O, Etienne JC, Fingerhut A. Incisional hernias. I. Related risk factors. Dig Surg. 2003; 20:3–9.14. Mingoli A, Puggioni A, Sgarzini G, Luciani G, Corzani F, Ciccarone F, et al. Incidence of incisional hernia following emergency abdominal surgery. Ital J Gastroenterol Hepatol. 1999; 31:449–453.15. Tang T, Peng W, Zhang L, Zuo Z, Cao D, Huang J, et al. Effectiveness and safety of total laparoscopic distal gastrectomy versus laparoscopy-assisted distal gastrectomy for gastric cancer: a retrospective cohort study. Am J Surg. 2018; 216:528–533.
Article16. Caglià P, Tracia A, Borzì L, Amodeo L, Tracia L, Veroux M, et al. Incisional hernia in the elderly: risk factors and clinical considerations. Int J Surg. 2014; 12:Suppl 2. S164–S169.
Article17. Patel SV, Paskar DD, Nelson RL, Vedula SS, Steele SR. Closure methods for laparotomy incisions for preventing incisional hernias and other wound complications. Cochrane Database Syst Rev. 2017; 11:CD005661.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of a Postoperative Pain in Laparoscopy-Assisted Distal Gastrectomy and Totally Laparoscopic Distal Gastrectomy according to the Location of the Mini-Laparotomy Site
- Risk of incisional hernia after laparoscopic colorectal surgery: surgeon’s worries and challenges
- Intracorporeal Anastomosis in Laparoscopic Gastric Cancer Surgery
- Incisional hernia after minimally invasive gastrectomy in gastric cancer patients
- Laparoscopic Distal Gastrectomy for Gastric Cancer