Ann Clin Microbiol.
2018 Sep;21(3):51-57. 10.5145/ACM.2018.21.3.51.
Clinical Utility of Fecal Immunochemical Transferrin Test in Gastrointestinal Bleeding Detection
- Affiliations
-
- 1Department of Laboratory Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. yjpk@catholic.ac.kr
- 2Department of Medical Life Science, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 3Department of Pediatrics, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 4Department of Gastroenterology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- KMID: 2429655
- DOI: http://doi.org/10.5145/ACM.2018.21.3.51
Abstract
- BACKGROUND
Gastrointestinal (GI) bleeding can result from various conditions, including ulcers, neoplasms and infectious enterocolitis. The aim of this study was to evaluate the utility of the fecal immunochemical transferrin test compared with the fecal Hb test in various clinical settings.
METHODS
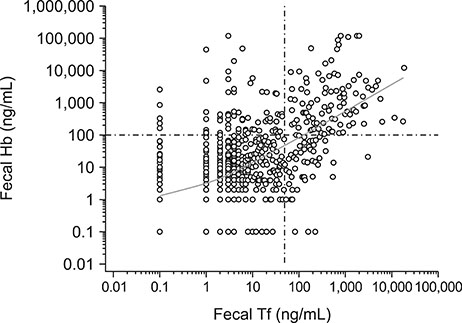
A total of 1,116 clinical stool specimens submitted for fecal occult blood testing were prospectively examined using both FIT Hb and FIT Tf kits (AlfresaPharma, Japan). To verify the specificity of the two tests, stool specimens from 265 health check-up examinees were also included.
RESULTS
A review of medical records revealed that 396 patients had clinical conditions associated with GI bleeding. FIT Hb and FIT Tf results were positive in 156 (39.4%) and 137 (34.6%) cases, respectively, and an additional 194 (49.0%) cases tested positive with either FIT Hb or FIT Tf. The two tests showed a moderate strength of agreement (kappa value; 0.56). Colitis (n=71) was associated with the most GI bleedings, followed by acute gastroenteritis (n=29), GI ulcers (n=27) and GI cancers (n=15). While the first two groups had higher positive rates on FIT Tf, patients in the latter two groups had higher positive rates on FIT Hb. Notably, four of nine specimens from premature babies tested positive only on FIT Tf. The specificity of FIT Hb and FIT Tf was 100% and 99.6%, respectively.
CONCLUSION
Concurrent use of FIT Hb and FIT Tf improved the detection rate of occult GI bleeding, especially in patients with infectious GI disease (such as colitis or gastroenteritis) and in premature babies.
Keyword
MeSH Terms
Figure
Reference
-
1. Camilleri M, Murray JA. Diarrhea and Constipation. In : Kasper D, Fauci A, Hauser S, Longo D, Jameson JL, Loscalzo J, editors. Harrison's Principles of Internal Medicine. 19th ed. New York: McGraw-Hill Education;2015. p. 264–274.2. Young GP, Symonds EL, Allison JE, Cole SR, Fraser CG, Halloran SP, et al. Advances in fecal occult blood tests: the FIT revolution. Dig Dis Sci. 2015; 60:609–622.
Article3. Demian WLL, Collins S, Fowler C, McGrath J, Antle S, Moores Z, et al. Evaluation of the analytical performance of the novel NS-Prime system and examination of temperature stability of fecal transferrin compared with fecal hemoglobin as biomarkers in a colon cancer screening program. Pract Lab Med. 2015; 2:29–36.
Article4. Jin P, Sheng JQ, Wu ZT, Meng MM, Wang X, Wang XW, et al. Combined fecal transferrin test and immuno fecal occult blood test for detecting colorectal cancer and advanced adenoma in asymptomatic and symptomatic populations. J Cancer Sci Ther. 2012; 4:243–248.5. Fletcher RH, Ransohoff DF, Imperiale TF. Comparison of a brush-sampling fecal immunochemical test for hemoglobin with a sensitive guaiac-based fecal occult blood test in detection of colorectal neoplasia. Cancer. 2007; 109:1925–1926. author reply 1926.
Article6. Aisen P, Listowsky I. Iron transport and storage proteins. Annu Rev Biochem. 1980; 49:357–393.
Article7. Uchida K, Matsuse R, Miyachi N, Okuda S, Tomita S, Miyoshi H, et al. Immunochemical detection of human blood in feces. Clin Chim Acta. 1990; 189:267–274.
Article8. Miyoshi H, Oka M, Sugi K, Saitoh O, Katsu K, Uchida K. Accuracy of detection of colorectal neoplasia using an immunochemical occult blood test in symptomatic referred patients: comparison of retrospective and prospective studies. Intern Med. 2000; 39:701–706.9. Takashima Y, Shimada T, Yokozawa T. Clinical benefit of measuring both haemoglobin and transferrin concentrations in faeces: demonstration during a large-scale colorectal cancer screening trial in Japan. Diagnosis (Berl). 2015; 2:53–59.
Article10. Levy BT, Bay C, Xu Y, Daly JM, Bergus G, Dunkelberg J, et al. Test characteristics of faecal immunochemical tests (FIT) compared with optical colonoscopy. J Med Screen. 2014; 21:133–143.
Article11. Imperiale TF, Ransohoff DF, Itzkowitz SH, Levin TR, Lavin P, Lidgard GP, et al. Multitarget stool DNA testing for colorectal-cancer screening. N Engl J Med. 2014; 370:1287–1297.
Article12. Chen JG, Cai J, Wu HL, Xu H, Zhang YX, Chen C, et al. Colorectal cancer screening: comparison of transferrin and immuno fecal occult blood test. World J Gastroenterol. 2012; 18:2682–2688.
Article13. Sheng JQ, Li SR, Wu ZT, Xia CH, Wu X, Chen J, et al. Transferrin dipstick as a potential novel test for colon cancer screening: a comparative study with immuno fecal occult blood test. Cancer Epidemiol Biomarkers Prev. 2009; 18:2182–2185.
Article14. Lai CC, Ji DD, Wu FT, Mu JJ, Yang JR, Jiang DD, et al. Etiology and risk factors of acute gastroenteritis in a Taipei emergency department: clinical features for bacterial gastroenteritis. J Epidemiol. 2016; 26:216–223.
Article15. Maayan-Metzger A, Ghanem N, Mazkereth R, Kuint J. Characteristics of neonates with isolated rectal bleeding. Arch Dis Child Fetal Neonatal Ed. 2004; 89:F68–F70.
Article16. Rayhorn N, Thrall C, Silber G. A review of the causes of lower gastrointestinal tract bleeding in children. Gastroenterol Nurs. 2001; 24:77–82. quiz 82-3.
Article17. Lackmann GM, Schnieder C, Bohner J. Gestational age-dependent reference values for iron and selected proteins of iron metabolism in serum of premature human neonates. Biol Neonate. 1998; 74:208–213.
Article18. Soldin OP, Bierbower LH, Choi JJ, Choi JJ, Thompson-Hoffman S, Soldin SJ. Serum iron, ferritin, transferrin, total iron binding capacity, hs-CRP, LDL cholesterol and magnesium in children; new reference intervals using the Dade Dimension Clinical Chemistry System. Clin Chim Acta. 2004; 342:211–217.
Article19. Pickering A, White R, Davis NL. Routine fecal occult blood testing does not predict necrotizing enterocolitis in very low birth weight neonates. J Neonatal Perinatal Med. 2016; 9:171–178.
Article20. Orkin SH, Nathan DG, Ginsburg D, Look AT, Fisher DE, Lux S. Nathan and Oski's Hematology of Infancy and Childhood. 7th ed. Philadelphia: Saunders/Elsevier;2009. p. 1778.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Usefulness of fecal immunochemical test and fecal calprotectin for detection of active ulcerative colitis
- The Significance of Fecal Immunochemical Test in National Cancer Screening Program
- Single Immunochemical Fecal Occult Blood Test for Detection of Colorectal Neoplasia
- Population Screening for Colorectal Cancer Means Getting FIT: The Past, Present, and Future of Colorectal Cancer Screening Using the Fecal Immunochemical Test for Hemoglobin (FIT)
- The Significance of Fecal Immunochemical Test to Screen for Colorectal Cancer in National Cancer Screening Program