Blood Res.
2018 Dec;53(4):307-313. 10.5045/br.2018.53.4.307.
Clinical presentation and treatment outcomes of primary ocular adnexal MALT lymphoma in Thailand
- Affiliations
-
- 1Department of Ophthalmology, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand.
- 2Division of Hematology, Department of Medicine, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand. Lalita.n@cmu.ac.th
- 3Department of Ophthalmology, Faculty of Medicine, King Chulalongkorn Memorial Hospital, Bangkok, Thailand.
- 4Division of Hematology, Department of Medicine, Faculty of Medicine, King Chulalongkorn Memorial Hospital, Bangkok, Thailand.
- KMID: 2429305
- DOI: http://doi.org/10.5045/br.2018.53.4.307
Abstract
- BACKGROUND
Primary ocular adnexal extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (POML) is the most common subtype of lymphoma involving the eyes in Thailand. We sought to assess the characteristics and treatment outcomes of patients with POML in Thailand.
METHODS
We retrospectively reviewed patient data and included patients diagnosed with POML between January 2004 and December 2016 at Chiang Mai University Hospital and King Chulalongkorn Memorial Hospital, Thailand. We collected and analyzed patients' clinical characteristics and treatment outcomes.
RESULTS
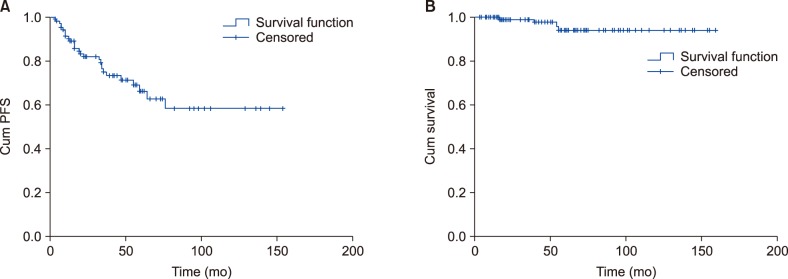
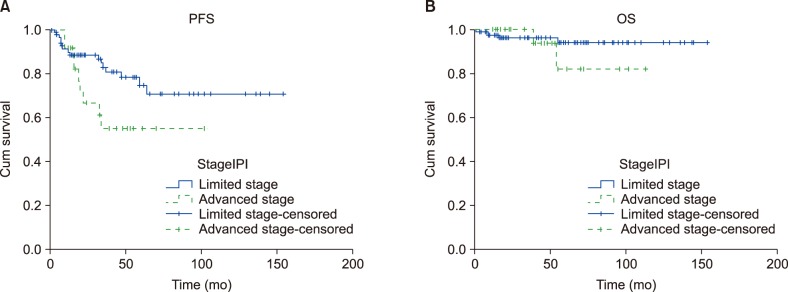
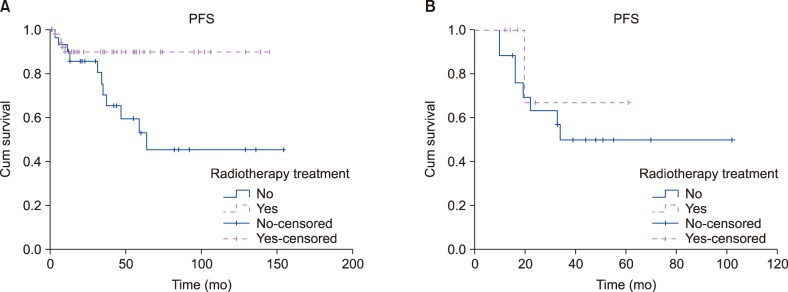
Among 146 patients with lymphoma involving the eyes, 121 (82%) were diagnosed with POML. Sixty-four (52.9%) were women with median age 58 (range, 22-86) years. The most common presenting symptom was orbital mass (71.1%). Common sites of origin were the orbit (46.3%) and lacrimal gland (34.7%). At presentation, 22.3% of patients had bilateral eye involvement. About half of patients had stage I disease (N=59, 56.2%) and 20% had stage IV. Most patients (73.3%) had a low-risk International Prognostic Index. Radiotherapy was the main treatment for patients with limited-stage disease (66.7% in stage I and 56.5% in stage II). The overall response rate was 100% with complete response rates 80%, 77.3%, and 64.7% for stages I, II, and IV, respectively. Five-year progression-free survival (PFS) and overall survival were 66.1% and 94.0%, respectively. For patients with limited-stage disease, radiotherapy significantly improved PFS compared with treatment not involving radiotherapy (5-year PFS 89.9% vs. 37.3%, P=0.01).
CONCLUSION
We revealed that POML has good response to treatment, especially radiotherapy, with excellent long-term outcome.
Keyword
MeSH Terms
Figure
Reference
-
1. Margo CE, Mulla ZD. Malignant tumors of the orbit. Analysis of the Florida Cancer Registry. Ophthalmology. 1998; 105:185–190. PMID: 9442797.2. Freeman C, Berg JW, Cutler SJ. Occurrence and prognosis of extranodal lymphomas. Cancer. 1972; 29:252–260. PMID: 5007387.
Article3. White WL, Ferry JA, Harris NL, Grove AS Jr. Ocular adnexal lymphoma. A clinicopathologic study with identification of lymphomas of mucosa-associated lymphoid tissue type. Ophthalmology. 1995; 102:1994–2006. PMID: 9098307.4. McKelvie PA, McNab A, Francis IC, Fox R, O'Day J. Ocular adnexal lymphoproliferative disease: a series of 73 cases. Clin Exp Ophthalmol. 2001; 29:387–393. PMID: 11778809.
Article5. Yen MT, Bilyk JR, Wladis EJ, Bradley EA, Mawn LA. Treatments for ocular adnexal lymphoma: a report by the american academy of ophthalmology. Ophthalmology. 2018; 125:127–136. PMID: 28712656.6. Ferreri AJ, Dolcetti R, Du MQ, et al. Ocular adnexal MALT lymphoma: an intriguing model for antigen-driven lymphomagenesis and microbial-targeted therapy. Ann Oncol. 2008; 19:835–846. PMID: 17986622.
Article7. Desai A, Joag MG, Lekakis L, et al. Long-term course of patients with primary ocular adnexal MALT lymphoma: a large single-institution cohort study. Blood. 2017; 129:324–332. PMID: 27789481.
Article8. Bayraktar S, Bayraktar UD, Stefanovic A, Lossos IS. Primary ocular adnexal mucosa-associated lymphoid tissue lymphoma (MALT): single institution experience in a large cohort of patients. Br J Haematol. 2011; 152:72–80. PMID: 21083656.
Article9. Graue GF, Finger PT, Maher E, et al. Ocular adnexal lymphoma staging and treatment: American Joint Committee on Cancer versus Ann Arbor. Eur J Ophthalmol. 2013; 23:344–355. PMID: 23397158.
Article10. Smiljanic M, Milosevic R, Antic D, et al. Orbital and ocular adnexal Mucosa-Associated Lymphoid Tissue (MALT) lymphomas: a single-center 10-year experience. Med Oncol. 2013; 30:722. PMID: 24026660.
Article11. Portell CA, Aronow ME, Rybicki LA, Macklis R, Singh AD, Sweetenham JW. Clinical characteristics of 95 patients with ocular adnexal and uveal lymphoma: treatment outcomes in extranodal marginal zone subtype. Clin Lymphoma Myeloma Leuk. 2014; 14:203–210. PMID: 24417911.
Article12. Ferreri AJ, Govi S, Pasini E, et al. Chlamydophila psittaci eradication with doxycycline as first-line targeted therapy for ocular adnexae lymphoma: final results of an international phase II trial. J Clin Oncol. 2012; 30:2988–2994. PMID: 22802315.13. Uno T, Isobe K, Shikama N, et al. Radiotherapy for extranodal, marginal zone, B-cell lymphoma of mucosa-associated lymphoid tissue originating in the ocular adnexa: a multiinstitutional, retrospective review of 50 patients. Cancer. 2003; 98:865–871. PMID: 12910532.
Article14. Tanimoto K, Kaneko A, Suzuki S, et al. Primary ocular adnexal MALT lymphoma: a long-term follow-up study of 114 patients. Jpn J Clin Oncol. 2007; 37:337–344. PMID: 17562719.
Article15. Han JJ, Kim TM, Jeon YK, et al. Long-term outcomes of first-line treatment with doxycycline in patients with previously untreated ocular adnexal marginal zone B cell lymphoma. Ann Hematol. 2015; 94:575–581. PMID: 25338969.
Article16. Harada K, Murakami N, Kitaguchi M, et al. Localized ocular adnexal mucosa-associated lymphoid tissue lymphoma treated with radiation therapy: a long-term outcome in 86 patients with 104 treated eyes. Int J Radiat Oncol Biol Phys. 2014; 88:650–654. PMID: 24521680.
Article17. Lee JL, Kim MK, Lee KH, et al. Extranodal marginal zone B-cell lymphomas of mucosa-associated lymphoid tissue-type of the orbit and ocular adnexa. Ann Hematol. 2005; 84:13–18. PMID: 15309523.
Article18. Son SH, Choi BO, Kim GW, et al. Primary radiation therapy in patients with localized orbital marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue (MALT Lymphoma). Int J Radiat Oncol Biol Phys. 2010; 77:86–91. PMID: 19632068.
Article19. Fung CY, Tarbell NJ, Lucarelli MJ, et al. Ocular adnexal lymphoma: clinical behavior of distinct World Health Organization classification subtypes. Int J Radiat Oncol Biol Phys. 2003; 57:1382–1391. PMID: 14630277.
Article20. Cahill M, Barnes C, Moriarty P, Daly P, Kennedy S. Ocular adnexal lymphoma-comparison of MALT lymphoma with other histological types. Br J Ophthalmol. 1999; 83:742–747. PMID: 10340987.
Article21. Wenzel C, Fiebiger W, Dieckmann K, Formanek M, Chott A, Raderer M. Extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue of the head and neck area: high rate of disease recurrence following local therapy. Cancer. 2003; 97:2236–2241. PMID: 12712477.22. Ferreri AJ, Guidoboni M, Ponzoni M, et al. Evidence for an association between Chlamydia psittaci and ocular adnexal lymphomas. J Natl Cancer Inst. 2004; 96:586–594. PMID: 15100336.
Article23. Nam H, Ahn YC, Kim YD, Ko Y, Kim WS. Prognostic significance of anatomic subsites: results of radiation therapy for 66 patients with localized orbital marginal zone B cell lymphoma. Radiother Oncol. 2009; 90:236–241. PMID: 18950885.
Article24. Hata M, Omura M, Koike I, et al. Treatment effects and sequelae of radiation therapy for orbital mucosa-associated lymphoid tissue lymphoma. Int J Radiat Oncol Biol Phys. 2011; 81:1387–1393. PMID: 20950950.
Article25. Coupland SE, Hellmich M, Auw-Haedrich C, Lee WR, Anagnostopoulos I, Stein H. Plasmacellular differentiation in extranodal marginal zone B cell lymphomas of the ocular adnexa: an analysis of the neoplastic plasma cell phenotype and its prognostic significance in 136 cases. Br J Ophthalmol. 2005; 89:352–359. PMID: 15722318.
Article26. Cho EY, Han JJ, Ree HJ, et al. Clinicopathologic analysis of ocular adnexal lymphomas: extranodal marginal zone b-cell lymphoma constitutes the vast majority of ocular lymphomas among Koreans and affects younger patients. Am J Hematol. 2003; 73:87–96. PMID: 12749009.
Article27. Auw-Haedrich C, Coupland SE, Kapp A, Schmitt-Gräff A, Buchen R, Witschel H. Long term outcome of ocular adnexal lymphoma subtyped according to the REAL classification. Revised European and American lymphoma. Br J Ophthalmol. 2001; 85:63–69. PMID: 11133714.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ocular adnexal mucosa-associated lymphoid tissue lymphoma: a narrative review
- Comparison of Ocular Adnexal Mantle Cell Lymphoma and MALT Lymphoma
- The Prognosis of Ocular-adnexal Lymphoproliferative Lesions
- MALT (mucosa associated lymphoid tissue) type Lymphoma of the Ocular Adnexa
- Recurrent Extranodal Marginal Zone B-Cell Lymphoma Presenting as a Huge Cheek Mass after Radiotherapy on Ocular Adnexal Lymphoma