Ann Rehabil Med.
2018 Oct;42(5):767-772. 10.5535/arm.2018.42.5.767.
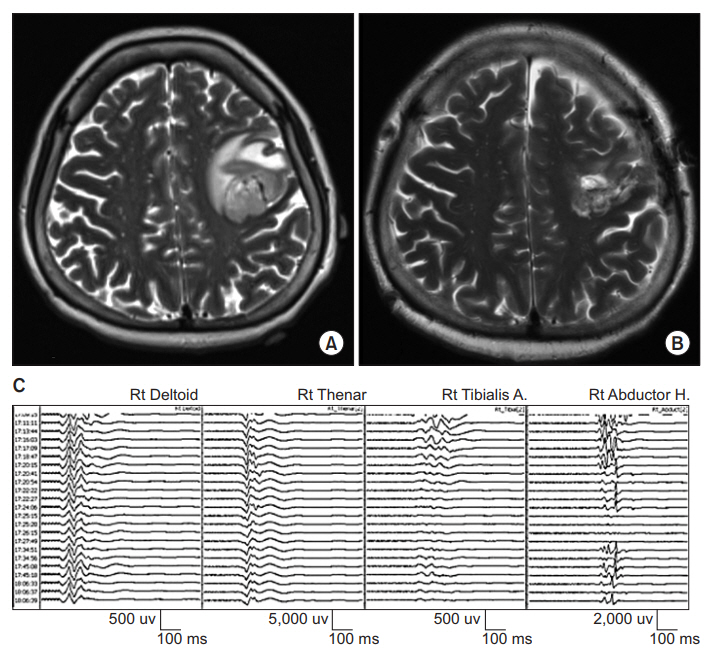
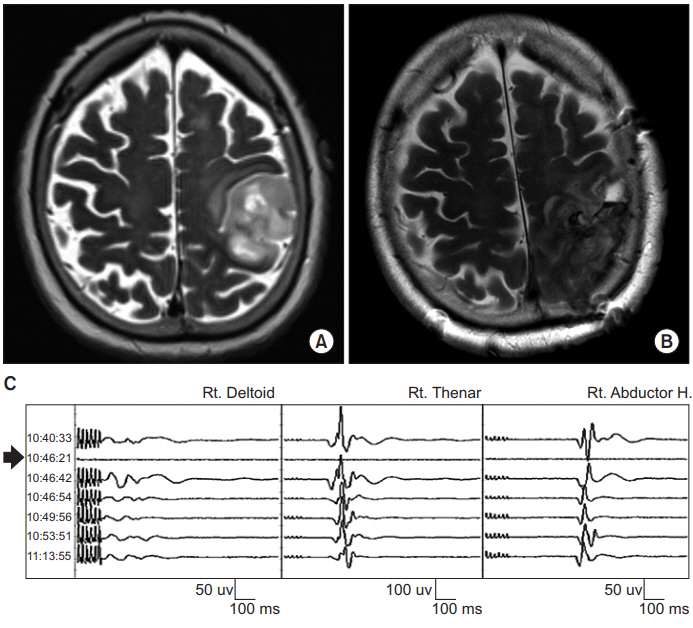
Limitation of Intraoperative Transcranial Electrical Stimulation-Motor Evoked Potential Monitoring During Brain Tumor Resection Adjacent to the Primary Motor Cortex
- Affiliations
-
- 1Department of Rehabilitation Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. seunghak@gmail.com
- 2Department of Neurosurgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Neurosurgery, Seoul National University Hospital, Seoul, Korea.
- KMID: 2429206
- DOI: http://doi.org/10.5535/arm.2018.42.5.767
Abstract
- Transcranial electrical stimulation-motor evoked potential (TES-MEP) is a valuable intraoperative monitoring technique during brain tumor surgery. However, TES can stimulate deep subcortical areas located far from the motor cortex. There is a concern about false-negative results from the use of TES-MEP during resection of those tumors adjacent to the primary motor cortex. Our study reports three cases of TES-MEP monitoring with false-negative results due to deep axonal stimulation during brain tumor resection. Although no significant change in TES-MEP was observed during surgery, study subjects experienced muscle weakness after surgery. Deep axonal stimulation of TES could give false-negative results. Therefore, a combined method of TES-MEP and direct cortical stimulation-motor evoked potential (DCS-MEP) or direct subcortical stimulation should be considered to overcome the limitation of TES-MEP.
MeSH Terms
Figure
Reference
-
1. Zhou HH, Kelly PJ. Transcranial electrical motor evoked potential monitoring for brain tumor resection. Neurosurgery. 2001; 48:1075–81.
Article2. Neuloh G, Pechstein U, Cedzich C, Schramm J. Motor evoked potential monitoring with supratentorial surgery. Neurosurgery. 2004; 54:1061–72.
Article3. Rothwell J, Burke D, Hicks R, Stephen J, Woodforth I, Crawford M. Transcranial electrical stimulation of the motor cortex in man: further evidence for the site of activation. J Physiol. 1994; 481(Pt 1):243–50.
Article4. Holdefer RN, Sadleir R, Russell MJ. Predicted current densities in the brain during transcranial electrical stimulation. Clin Neurophysiol. 2006; 117:1388–97.
Article5. Szelenyi A, Kothbauer K, de Camargo AB, Langer D, Flamm ES, Deletis V. Motor evoked potential monitoring during cerebral aneurysm surgery: technical aspects and comparison of transcranial and direct cortical stimulation. Neurosurgery. 2005; 57(4 Suppl):331–8.6. Macdonald DB. Intraoperative motor evoked potential monitoring: overview and update. J Clin Monit Comput. 2006; 20:347–77.
Article7. Boex C, Haemmerli J, Momjian S, Schaller K. Prognostic values of motor evoked potentials in insular, precental, or postcentral resections. J Clin Neurophysiol. 2016; 33:51–9.
Article8. Motoyama Y, Kawaguchi M, Yamada S, Nakagawa I, Nishimura F, Hironaka Y, et al. Evaluation of combined use of transcranial and direct cortical motor evoked potential monitoring during unruptured aneurysm surgery. Neurol Med Chir (Tokyo). 2011; 51:15–22.
Article9. Keles GE, Lundin DA, Lamborn KR, Chang EF, Ojemann G, Berger MS. Intraoperative subcortical stimulation mapping for hemispherical perirolandic gliomas located within or adjacent to the descending motor pathways: evaluation of morbidity and assessment of functional outcome in 294 patients. J Neurosurg. 2004; 100:369–75.10. Saito T, Muragaki Y, Maruyama T, Tamura M, Nitta M, Okada Y. Intraoperative functional mapping and monitoring during glioma surgery. Neurol Med Chir (Tokyo). 2015; 55:1–13.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Optimal Condition for Activation of Motor Cortex by Peripheral Electrical Stimulation in Rat
- Motor Evoked Potentials by Transcranial Magnetic Stimulation
- Changes in Activity of Human Motor Cortex Caused by Hyperbaric Air Therapy
- Monitoring of Motor and Somatosensory Evoked Potentials During Spine Surgery: Intraoperative Changes and Postoperative Outcomes
- Motor Evoked Potentials in Masseter, and Anterior Belly of Digastric Induced by Transcranial Magnetic Stimulation