J Korean Orthop Assoc.
2018 Jun;53(3):264-270. 10.4055/jkoa.2018.53.3.264.
Complications of Allograft Reconstruction following Wide Resection of Malignant Bone Tumors in Long Bones
- Affiliations
-
- 1Department of Orthopaedic Surgery, Eulji University College of Medicine, Daejeon, Korea. oskkj@eulji.ac.kr
- KMID: 2429175
- DOI: http://doi.org/10.4055/jkoa.2018.53.3.264
Abstract
- PURPOSE
We evaluated the results of allograft reconstruction following wide resection of malignant bone tumors in long bone, retrospectively.
MATERIALS AND METHODS
Seven patients were included. The mean age was 44 years old. Male was 4 cases, and female was 3 cases. Mean follow-up period was 38 months. The mean Musculoskeletal Tumor Society (MSTS) score at final follow-up was evaluated. Postoperative complications were evaluated via periodic radiologic follow-up. Oncologic results were analyzed at final follow-up.
RESULTS
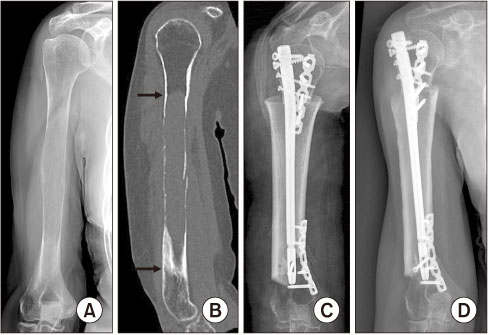
The primary malignancies occurred at femur in 5 cases, humerus in 1 case and tibia in 1 case. Pathologic diagnoses were osteosarcoma in 4 cases, multiple myeloma in 2 cases and adamantinoma in 1 case. Mean length of allograft was 165 mm. Fixations of allograft were intramedullary nailing with additional plate in 4 cases, intramedullary nailing in 2 cases, and screw fixation in 1 case. Mean time to union was 14.5 weeks. Mean MSTS score at final follow-up was 20 (67%). Postoperative complications were nonunion in 3 cases, implant failure in 1 case, and infection in 1 case. Oncologic outcomes were continuous disease free in 5 cases and alive with disease in 2 cases at final follow-up. Autologous bone graft and hemi-cortical onlay graft were performed in 2 cases of nonunion.
CONCLUSION
Allograft reconstruction following wide resection of malignant bone tumors in long bone was effective surgical option. However, the possibility of nonunion between host bone and allograft should be considered.
Keyword
MeSH Terms
Figure
Reference
-
1. Gitelis S, Piasecki P. Allograft prosthetic composite arthroplasty for osteosarcoma and other aggressive bone tumors. Clin Orthop Relat Res. 1991; (270):197–201.
Article2. Izawa H, Hachiya Y, Kawai T, et al. The effect of heat-treated human bone morphogenetic protein on clinical implantation. Clin Orthop Relat Res. 2001; (390):252–258.
Article3. Rougraff BT, Simon MA, Kneisl JS, Greenberg DB, Mankin HJ. Limb salvage compared with amputation for osteosarcoma of the distal end of the femur. A long-term oncological, functional, and quality-of-life study. J Bone Joint Surg Am. 1994; 76:649–656.
Article4. Cannon SR. Massive prostheses for malignant bone tumours of the limbs. J Bone Joint Surg Br. 1997; 79:497–506.
Article5. Glasser DB, Lane JM. Stage IIB osteogenic sarcoma. Clin Orthop Relat Res. 1991; (270):29–39.
Article6. Tsuchiya H, Tomita K, Minematsu K, Mori Y, Asada N, Kitano S. Limb salvage using distraction osteogenesis. A classification of the technique. J Bone Joint Surg Br. 1997; 79:403–411.7. Tsuchiya H, Wan SL, Sakayama K, Yamamoto N, Nishida H, Tomita K. Reconstruction using an autograft containing tumour treated by liquid nitrogen. J Bone Joint Surg Br. 2005; 87:218–225.
Article8. Kim KJ, Kim HS, Kang HG, et al. Reconstruction with replantation of the resected bone after low heat treatment for malignant pelvic bone tumors. J Korean Orthop Assoc. 2006; 41:519–526.
Article9. Han CS, Wood MB, Bishop AT, Cooney WP 3rd. Vascularized bone transfer. J Bone Joint Surg Am. 1992; 74:1441–1449.
Article10. Alman BA, De Bari A, Krajbich JI. Massive allografts in the treatment of osteosarcoma and Ewing sarcoma in children and adolescents. J Bone Joint Surg Am. 1995; 77:54–64.
Article11. Gebhardt MC, Roth YF, Mankin HJ. Osteoarticular allografts for reconstruction in the proximal part of the humerus after excision of a musculoskeletal tumor. J Bone Joint Surg Am. 1990; 72:334–345.
Article12. Chen TH, Chen WM, Huang CK. Reconstruction after intercalary resection of malignant bone tumours: comparison between segmental allograft and extracorporeally-irradiated autograft. J Bone Joint Surg Br. 2005; 87:704–709.13. Ehara S, Nishida J, Shiraishi H, Tamakawa Y. Pasteurized intercalary autogenous bone graft: radiographic and scintigraphic features. Skeletal Radiol. 2000; 29:335–339.
Article14. Manabe J, Ahmed AR, Kawaguchi N, Matsumoto S, Kuroda H. Pasteurized autologous bone graft in surgery for bone and soft tissue sarcoma. Clin Orthop Relat Res. 2004; (419):258–266.
Article15. Rong Y, Sato K, Sugiura H, et al. Effect of elevated temperature on experimental swarm rat chondrosarcoma. Clin Orthop Relat Res. 1995; (311):227–231.16. Aho AJ, Ekfors T, Dean PB, Aro HT, Ahonen A, Nikkanen V. Incorporation and clinical results of large allografts of the extremities and pelvis. Clin Orthop Relat Res. 1994; (307):200–213.17. Asada N, Tsuchiya H, Kitaoka K, Mori Y, Tomita K. Massive autoclaved allografts and autografts for limb salvage surgery. A 1-8 year follow-up of 23 patients. Acta Orthop Scand. 1997; 68:392–395.18. Hornicek FJ, Gebhardt MC, Tomford WW, et al. Factors affecting nonunion of the allograft-host junction. Clin Orthop Relat Res. 2001; (382):87–98.
Article19. Ortiz-Cruz E, Gebhardt MC, Jennings LC, Springfield DS, Mankin HJ. The results of transplantation of intercalary allografts after resection of tumors. A long-term follow-up study. J Bone Joint Surg Am. 1997; 79:97–106.
Article20. Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993; (286):241–246.
Article21. Brien EW, Terek RM, Healey JH, Lane JM. Allograft reconstruction after proximal tibial resection for bone tumors. An analysis of function and outcome comparing allograft and prosthetic reconstructions. Clin Orthop Relat Res. 1994; (303):116–127.22. Gebhardt MC, Flugstad DI, Springfield DS, Mankin HJ. The use of bone allografts for limb salvage in high-grade extremity osteosarcoma. Clin Orthop Relat Res. 1991; (270):181–196.
Article23. Mnaymneh W, Malinin TI, Lackman RD, Hornicek FJ, Ghandur-Mnaymneh L. Massive distal femoral osteoarticular allografts after resection of bone tumors. Clin Orthop Relat Res. 1994; (303):103–115.
Article24. Mankin HJ, Gebhardt MC, Jennings LC, Springfield DS, Tomford WW. Long-term results of allograft replacement in the management of bone tumors. Clin Orthop Relat Res. 1996; (324):86–97.
Article25. Jeon DG, Song WS, Cho WH, et al. Overlapping allograft for primary or salvage bone tumor reconstruction. J Surg Oncol. 2014; 110:366–371.
Article26. Judas F, Saavedra MJ, Mendes AF, Dias R. Cortical strut allografting in reconstructive orthopaedic surgery. Acta Reumatol Port. 2011; 36:24–28.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Allograft Reconstruction Following the Segmental Resection of Malignant Bone Tumors in the Long Bones
- Bone Reconstruction: Structural Allograft and Autograft
- Reconstruction of Large Bone Defect after Wids Segmental Resection of Long Bone Tumors Using the Free Vascularized Fibular Graft
- Recent Advances in Malignant Bone Tumor Treatment
- Surgical Resection of Malignant Bone Tumors